Back to Journals » Clinical Ophthalmology » Volume 17
Cataract Surgery Visual Outcome and Associated Factors Among Adults Attended Jimma University Medical Center, Jimma, Southwest Ethiopia
Authors Mohammed J, Assegid S, Fekadu L , Kabeta T
Received 9 August 2023
Accepted for publication 24 October 2023
Published 3 November 2023 Volume 2023:17 Pages 3341—3351
DOI https://doi.org/10.2147/OPTH.S434453
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Jemmal Mohammed,1 Sahilu Assegid,2 Lata Fekadu,2 Teshome Kabeta2
1Department of Ophthalmology, Faculty of Medical Science, Institute of Health, Jimma University, Jimma, Ethiopia; 2Department of Epidemiology, Faculty of Public Health, Institute of Health, Jimma University, Jimma, Ethiopia
Correspondence: Lata Fekadu, Jimma University, Institute of Health, Faculty of Public Health, Department of Epidemiology, PO Box 378, Jimma, Ethiopia, Tel +251911924107, Email [email protected]
Background: Cataract is the leading cause of blindness and the second leading cause of visual impairment worldwide, accounting for 51% and 33% of all cases, respectively, in low- and medium-income countries bearing a disproportionately high burden. Hence, this study aimed to assess the visual outcome of age-related cataract surgery and identify factors associated with patients’ postoperative visual outcomes in Jimma University Medical Center, Southwest Ethiopia.
Methods: An institution-based cross-sectional study design was conducted among 386 cataract surgery patients from January 1, 2016, to December 30, 2017. The study participants were selected using a systematic random sampling technique. Data were collected by reviewing the selected patients’ medical records using a pre-tested checklist, entered into EpiData version 3.1, and exported to SPSS 20 for analysis. Proportions, summary statistics, and tables were used for presentations of the findings. Binary logistic regression was carried out to identify independent predictors of visual outcome. Findings were presented with adjusted odds ratios and their 95% confidence interval. A p-value < 0.05 was used to declare a statistically significant association.
Results: About 231 individuals (59.8%) had poor visual results following cataract surgery. Furthermore, age > 70 (AOR = 3.64; 95% CI [1.35– 9.82]), preoperative ocular co-morbidities (AOR = 2.34; [1.32– 4.15]), incision-based cataract surgery (AOR = 7.11; [3.16– 16.02]), compared phacoemulsification operated by resident surgeons (AOR = 2.19; [1.23– 3.89]), presence of intraoperative complication (AOR = 3.41; [1.47– 7.92]), lens remnant (AOR = 2.91; [1.11– 4.92]), ocular inflammation (OR = 2.56; [1.34– 4.92]), and striate keratopathy/corneal edema (AOR = 1.91; [1.07– 3.44]) were significantly associated with poor visual outcome.
Conclusion: The visual outcome following cataract surgery fall below WHO recommendation. In this study, age, ocular co-morbidities, surgical method, surgeon status, intraoperative complication, SK, and ocular inflammation associated with post-operative Uveitis and anterior chamber reaction were associated with a poor visual outcome.
Keywords: cataract surgery, visual outcome, Jimma University Medical Center
Background
Cataract is the leading cause of blindness and the second leading cause of visual impairment worldwide, accounting for 51% and 33% of all cases, respectively. The huge burden of cataracts found in low- and medium-income countries contributes about 90% of cataract-related blindness to the world.1 Cataract affects mainly old aged people as natural occurring phenomena of aging.2–4 In Ethiopia, where 10% of the population is over 50 years old, cataract accounts for 49.9% of blindness and 42.3% of visual impairment, respectively.5,6 Cataract affects daily activities and independent living that leads to diminished quality of life and also has an adverse effect on the physical and mental health of individuals.7–10 As result, cataract causes sizeable social and economic disadvantages, especially in poor communities, and contributes to the perpetual cycle of poverty.11–13
Cataract surgery is the removal of an opacified lens and is usually replaced with an artificial intraocular lens (IOL), and it is the first and last available management of cataracts.3 It is the most frequently performed elective, effective surgery identified as “Essential Surgeries” by the World Bank.4,14,15 World health organization (WHO) recommends that after surgery at least 80% of the operated eyes should have a presenting visual acuity of 6/6–6/18, which is referred to as a good visual outcome, whereas poor visual outcome cases (less than 6/60) should have less than 5%. After the best correction, at least 90% of the eyes should achieve this level of vision.16 Despite these facts, the outcome of cataract surgery in sub-Saharan countries is below WHO recommendation.17
Provision of high-quality cataract surgery is one of the aims of universal eye health.18 Measuring quality cataract surgery outcomes is increasingly attracting interest since visual outcome matters to the individual patient, community, and finally the surgical uptake of institutions. Post-operative visual acuity is the most popular way to assess the quality of cataract surgery.19 Post-operative visual acuity is a biomarker output indicator of the quality of cataract surgery.20,21
Many factors, including socio-demographic factors, ocular comorbidity, and systemic conditions, intraoperative and postoperative complications (gender, age, surgical technique used, surgical facilities, glaucoma, age-related macular degeneration, and diabetes mellitus), affect the post-operative visual acuity of patients.17–19,22–30 x The introduction of a novel cataract surgery process, phacoemulsification, and then evaluating the influence of the new surgical procedures (procedure) on the visual outcome in the study area prompted us to conduct this study. In addition, the research done in the study area was many years ago which may show the current situation. The current study aimed to evaluate the visual outcome of cataract surgery and to identify the associated factors that affect patients’ post-operative visual outcomes at Jimma University Medical Center.
Materials and Methods
Study Setting and Population
An Institutional-based cross-sectional record review study was conducted at Jimma University Medical Center, Ethiopia, from January 1, 2016, to December 30, 2017. Jimma University Medical Center provides medical and training services. Jimma University Department of Ophthalmology (JUDO) as part of the medical center has a residency training program and offers comprehensive ophthalmic services for the community, having 04 general outpatient departments (OPD), 03 operation rooms, and 04 wards and sub-specialty clinics. The subspecialty clinics are anterior segment, vitreoretinal, glaucoma, and pediatric ophthalmology clinics. New patients examined diagnosed and treated at the general OPD. Some patients might be sent to sub-specialty clinics for further examination and follow-up. Others might link to the OR and ward for admission. It is the only tertiary referral clinic that provides ophthalmic service for more than 10 million people and is the only center performing cataract surgeries in southwest Ethiopia.31 In our setup, auto keratometers and contact A-scan are used for corneal curvature and axial length measurement. Different IOL calculation formulas (SRK/T, Hoffer Q, Holladay, and Haigis) were utilized according to the axial length. In the setup, post-cataract surgery, we usually prescribe steroids (dexamethasone) and antibiotic (ciprofloxacin) eye drops.
The inclusion criterion was having cataract surgery for age-related cataracts from January 1, 2016, to December 30, 2017. The study participants were chosen at random from the cataract surgery registry book. And then the medical records of selected patients were reviewed to extract data. We excluded patients with secondary anterior chamber intraocular lens (AC IOL) if the main surgery was performed during the research period. This is to avoid data duplication. Traumatic cataract and combined surgery cases were excluded. In addition, we excluded patients whose 4–11 weeks post-operative visual acuities were not recorded.
Sample Size and Sampling Procedure
The sample size was determined by using the single population proportion formula. In light of this, P=12.3%, where “P” denotes the percentage of patients with poor vision who underwent cataract surgery in a prior study31 and with a 5% level of significance (α) and a 3% margin of error. Thus, 386 patients were the final sample size determined using EpiInfo statistical software. Two thousands three hundreds ninety-one patients who had cataract operations who met the inclusion criteria in the study period. The Systematic random sample technique was used to choose 386 surgery cases (k = 2391/386 = 6). First, using a surgery registration book, six medical record numbers of cataract surgery patients were identified, and one medical record number was chosen by random. The eligibility of the specified medical record was then examined. After that, every sixth medical record number was chosen. When the first medical record was determined to be ineligible, the next was considered. One eye was chosen by lottery in situations of bilateral cataract surgery.
Data Collection Tool and Procedure
The data extraction checklist was derived from the WHO cataract surgery outcome monitoring form and reviewed works of literature.32 The checklist was tested on 5 medical records and any necessary changes were made. The data was collected by trained optometrists. Socio-demographic characteristics, medical history, pre-operative ocular findings, and intraoperative and post-operative complications related to cataract surgery were collected from selected patients’ medical records. In addition, the post-operative visual acuities of the selected patients at 4–11 weeks were collected from the medical record.
The data collectors were trained about data collection, quality, and confidentiality for one day. Before beginning data collection, all duplicated checklists were extensively reviewed for legibility. During data collection, the data collectors were closely monitored and frequent checks were made to ensure that the information acquired was full and consistent. Before analyzing the data, checking to ensure accuracy, consistency, and the absence of missing values was done.
Data Processing and Analysis
Epi-data version 3.1 was used to enter data, which was then exported to SPSS version 20 for analysis. To summarize socio-demographic, medical history, intraoperative and preoperative, and post-operative features of the patients’ data, descriptive statistics such as, proportion, mean, and standard deviation were utilized.
The visual outcome of cataract surgery was classified into two categories in inferential statistics: good and bad (the WHO classification of borderline and poor visual outcome grouped as poor.16 Additionally, the category of each variable like intra-operative complications (as absent/present), ocular co-morbidities (as absent/present), IOL type (AC, sulcus, and no IOL were grouped and PC IOL, on the other hand), and surgical technique (ICCE, ECCE, and SICS were grouped; named as incision based and PHACO, on the other hand) were regrouped. The reason for grouping the above variables as indicated was for the application of meaningful inferential statistics; since some groups were few. Therefore, the number of variables to be included in the model should be the minimum possible that is parsimonious and delivers optimum information. In this study, the variable selection process begins with the univariable analysis of each independent variable with the response variable separately. Tests to determine whether a systematic relation or association between each predictor variable with patients who underwent age-related cataract surgery existed before the final model was selected. Any variable whose univariable test has a p-value ≤ 0.25 is a candidate for a multiple logistic regression model along with all variables of known statistical importance. Variables that have a P-value of less than 0.05 with a 95% corresponding confidence interval were considered to judge the statistical significance of the variables. Assessing goodness of fit by investigating how close values are predicted by the model with that of observed values. Before interpreting the results of a multiple logistic regression model, the goodness of fit was checked by the Hosmer and Lemeshow chi-square test.
Results
Socio-Demographic Characteristics of Study Participants
A total of 386 patients who underwent cataract surgery in Jimma University Medical Center aged 40 years and above were included in the study, of which 55.2% are males. The majority of patients, 265 (68.7%), came from rural areas. About 149 (38.6%) were in the 60- to 69-year-old age group. In terms of medical conditions, 29 individuals (7.5%) had diabetes mellitus (DM) and 26 (6.7%) had a history of hypertension (HTN) (Table 1).
 |
Table 1 Baseline Socio-Demography Characteristic Patients, Who Underwent Cataract Surgery in Jimma University Medical Center, from January 1, 2016, to December 30, 2017 (N = 386) |
Preoperative Ocular and Preoperative Ocular Comorbidity Characteristic of the Study Participants
Only six (1.6%) of the 386 patients had good eyesight before surgery, according to the WHO categorization of post-operative visual acuity. Nearly three-fourths of the patients, 285 (73.8%), had normal cataract lenses. About 83 (21.5%) of the patients had pseudoexfoliation, iridodonesis, or phacodonesis. Aphakia, or subluxated/dislocated lens, affected eighteen people. Preoperatively 379 individuals (98.2%) had normal intraocular pressure (IOP). Nearly half of the patients 191 (49.5%) had biometry measurements.
In terms of ocular comorbidity, 386 patients (29.27%) had various types of ocular co-morbidities before surgery (preoperatively). A total of 40 patients (10.36%) had corneal opacity, dystrophy, or Pterygium. In 30 (7.77%) of the patients, glaucoma, or optic atrophy was found. Because the posterior section is obscured by the cataract, the posterior segment was not inspected or investigated in 40 (10.36%) of the patients. In addition, 14 (3.63%) of the patients had strabismus. (Tables 2 and 3).
 |
Table 2 Preoperative and Its Comorbidities Among Cataract Patients Who Underwent Surgery in JUMC, January 1, 2016, to December 30, 2017, Jimma, Ethiopia |
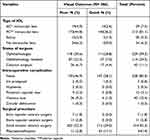 |
Table 3 Intra-Operative Characteristics of Cataract Patients Who Underwent Surgery in JUMC, January 1, 2016, to December 30, 2017, Jimma, Ethiopia |
Surgical-Related Characteristics of Study Participants
SICS with PC IOL 314 was the most commonly utilized procedure (81.3%), followed by PHACO 54 (14%). The majority of the surgeries, 229 (59.3%) eyes, were performed by an ophthalmologist, and 111 (28.8%) eyes had a good outcome 4–11 weeks after surgery. Around 313 (81.1%) of the eyes had a posterior capsular intraocular lens (PC IOL), while 29 (7.5%) of the eyes were aphakic (without IOL). About 140 (36.5%) of individuals who received a PC IOL had a positive outcome. The most common intraoperative complication was the vitreous loss, which occurred in 40 (10.4%) of the eyes, followed by a posterior capsular tear (pc tear) in 12 (3.1%) of the eyes.
Post-Operative Visual Acuity (4–11 Week After Cataract Surgery)
Of the 386 eyes operated for cataracts, about 155 (40%) got good VA ((≥6/18)), 148 (38.3%) were in borderline VA (6/60-6/18), and 83 (21.5%) resulted in poor visual acuity after cataract surgery (Figure 1).
 |
Figure 1 Preoperative and postoperative VA of cataract patients at Jimma Medical Center 2016–2017. |
Factors Associated with Postoperative Visual Outcome
Age, presence of DM, operated eye, ocular comorbidity, lens conditions, type of cataract, biometry measurement, surgical technique, seniority of the surgeon, intraoperative complication, IOL type, corneal edema, post-operative intra-ocular inflammation, IOL dislocation, and lens remnant were found to be significant in bivariable binary logistic regression analysis of each independent variable with the outcome variables and were included in multiple logistic regressions.
Age, ocular comorbidity, surgical technique, surgeon seniority, intraoperative complication, striate keratitis (SK), and post-operative ocular inflammation (anterior chamber reaction and uveitis) were all shown to be significantly (p-value less than 0.05) associated with visual outcome in multiple logistic regression.
Those aged 70 and up had about three times increased odds of a poor outcome compared to those aged 40–49 years (AOR= 3.16 CI [1.19–8.39]). Patients with ocular comorbidity were 2.86 times more likely to have an increased risk of poor visual outcome compared with those without ocular comorbidity (AOR = 2.86, 95% CI [1.60–5.10]). When comparing those who had a small incision cataract surgical procedure to those who had a phacoemulsification (PHACO) treatment, the odds of having a poor outcome were almost seven times higher (AOR = 5.56, [2.48–12.43]). Those who had an intraoperative complication had a 4.49 times higher chance of having a poor outcome (AOR = 4.49, [1.88–10.72]) than others who did not. Patients with postoperative intra-ocular inflammation had 2.63 times (AOR = 2.56, [1.40–4.94]) greater odds of poor outcome than those without (Table 4).
 |
Table 4 Factors Associated with Visual Outcome Among Patients Underwent Cataract Surgery at JUMC, January 1, 2016, to December 30, 2017, Jimma, Ethiopia |
Discussion
The current study has investigated cataract surgery and associated factors at the facility level in southwest Ethiopia. Three-fifths of the patients had poor outcomes after cataract surgery. Poor outcome was associated with old age, presence of ocular comorbidity, incision-based surgical techniques, surgeon seniority, presence of intraoperative complication, striate keratopathy, and post-operative intra-ocular inflammation.
The proportion of patients with a poor outcome did not match the WHO standard, which says that less than 5% of cases should have a poor visual outcome (6/60) – post-cataract surgery.16 The proportion of patients who had a poor outcome is higher than in studies conducted in Malaysia at Sultan Haji Ahmad Shah Hospital, Armenia at Lions Regional Ophthalmic Unit, and India at LV Prasad Eye Institute.23,27,33 This could be due to differences in glass correction among participants in the study, as these studies employed best-corrected visual acuity, whereas we used current visual acuity. The proportion of poor visual outcomes in our findings was lower than those of a study conducted in Gondar, Ethiopia.26,34 In addition to the standard approach used by both institutions, Jimma University Medical Center employs the phacoemulsification surgical technique, which has produced the best outcomes.35 Furthermore, the proportion of poor outcomes in this study is larger than in a previous study at the same center.31 This could be due to the study participants’ varying ages and lack of experience with the new procedure.
When comparing patients aged 40–49 years to those aged greater than 70 years, the likelihood of a poor visual outcome was almost three times fold. Since people get older, their cataracts become denser, making it difficult to see details of the posterior segment. This finding goes to the result of a study done in India.33
According to this study, having an ocular comorbidity increases the odds of a poor outcome by 2.5 times when compared to not having one. This is in line with the findings of studies conducted at the Eastern Regional Health Authority hospital in Trinidad and Tobago, in Gupta, India, and the Aga Khan University Hospital in Pakistan, as well as Uganda.25,36–38
The proportion of SICS with IOL procedure (81.3%) was more common than the proportion of PHACO procedure, which is 14%. The proportion of SICS with IOL procedure in this study was similar to what was found in Ghana (83.8%), Uganda (87.7%), and Gondar (Ethiopia) (91.74%).24,34,37 On the other hand, the proportion of PHACO procedures is lower compared to the proportion of PHACO procedures performed in the Eastern Regional Health Authority hospital in Trinidad and Tobago and the LV Prasad Eye Institute study. This is due to the PHACO procedure being a cutting-edge procedure that requires highly trained and professional personnel. As a result, machines and/or skilled labor will be unavailable in developing countries.39 This could explain why the percentage of PHACO procedures is lower. Some kinds of literature suggest small incision cataract surgery is advised for developing countries since many cases come with matured cataracts.40,41 When surgical methods based on incisions (SICS, ICCE, and ECCE) were compared to PHACO, the odds of a poor outcome increased by 7.11 times.
This might be less induced astigmatism in the case of PHACO compared to SICS and a high complication rate in the case of incision-based procedures.42,43 This is in line with prior research from the Trinidad and Tobago Eastern Regional Health Authority hospital and the LV Prasad Eye Institute. This is because of the astigmatism produced by incision-based surgery.35,44,45
When comparing those who had intraoperative complications to those who did not, the risks of a poor result are around 3.41 times higher. This is comparable to the findings of a study conducted at India’s LV Prasad Eye Institute.33
The proportion of striate keratopathy is commonly observed post-operative complication in this study, as it was in the previous study in Jimma, Ethiopia, but higher than the findings of studies conducted in Gondar, Ethiopia, and the LV Prasad Eye Institute in India.26,31,33 The researcher discovered that those with striate keratopathy/ corneal edema have approximately two times higher odds of poor vision than those without. This is in line with the findings of a study conducted in Gondar, Ethiopia.26
Those who had ocular inflammations (uveitis and anterior chamber reaction) were 2.5 times more likely to have a poor visual outcome than those who did not which was similar to the one reported at Gondar.26
Limitations of the Study
The association between post-operative complications and visual outcome was investigated, which is the study’s strong point. This research has certain drawbacks. To begin, only the current VA was evaluated in this investigation because the post-operative refractive state was not known. Second, because this is a cross-sectional hospital-based study based on medical records, some variables such as income, educational status, and drug adherence were overlooked. Despite these limitations, it is believed that this study adequately identifies factors associated with poor cataract surgery visual outcomes.
Conclusion
The proportion of poor and good results was lower than the WHO recommendation.
Being old age, the presence of ocular co-morbidity, incision-based surgical techniques, operated by resident ophthalmology, the presence of intraoperative complication, the presence of SK, and the presence of ocular inflammation related to Uveitis and anterior chamber reaction were all associated to a poor visual outcome in this study.
Recommendation
The following recommendations were made based on the study’s findings: for Jimma University Medical Center, specifically the Department of Ophthalmology.
It is advised that people over the age of 70 with diabetes mellitus and ocular co-morbidities have a specific emphasis. It is also critical to improve resident follow-up throughout practice, particularly after surgery, to reduce surgery-related complications such as lens remnants and SK. Encourage the use of the PHACO technique. Strengthen (follow the procedure) proper intraoperative prophylactic drug use. It is recommended that patients be referred for post-operative refraction services during follow-up. It is also suggested that every effort be made to ensure that patient’s medical records are as complete and thorough as possible.
Abbreviations
AC IOL, anterior chamber intraocular lens; AOR, adjusted odd ratio; AMD, age-related macular degeneration; COR, crude odd ratio; CI, confidence interval; DM, diabetic mellitus; ECCE, extracapsular cataract surgery; IOL, intraocular lens; IOP, Intraocular pressure; ICCE, intracapsular cataract surgery; JUDO, Jimma University department of ophthalmology; PC IOL, posterior chamber intraocular lens; PHACO, phacoemulsification; PC, posterior capsule; SSA, sub-Saharan Africa; SK, striate keratitis; SICs, small incision cataract surgery; UHC, universal health coverage; VA, visual acuity; WHO, World Health Organization.
Data Sharing Statement
Data will be available upon request from the corresponding author.
Ethics Approval
Ethical approval for the research was obtained from Jimma University, Institute of Health Research Ethics Committee with IRB00097\17 reference number. The consent of the patient to review their medical records was not required by this Ethics Committee and it was conducted according to the waiver of the Declaration of Helsinki for studies on human subjects.
Acknowledgment
We would like to thank Jimma University for its support for the realization of this funding. We are also grateful for Jimma University Medical Center, which provides medical and training services and is the only referral hospital in southwest Ethiopia.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was funded by the Institute of Health of Jimma University as a partial fulfillment of the MPH degree of the first author.
Disclosure
The authors declare that they have no conflicts of interest for this work.
References
1. Pascolini D, Mariotti SP. GLOBAL DATA ON visual impairment. Br J Ophthalmol. 2010;96(5):614–618.
2. Ophthalmology secrets in color by James F. Vander | goodreads. 2022. Available from: https://www.goodreads.com/book/show/23615576-ophthalmology-secrets-in-color.
3. Allen D, Vasavada A. Cataract and surgery for cataract. Br Med J. 2006;333(7559):128–132. doi:10.1136/bmj.333.7559.128
4. Gray Z, Ackland P. Cataract surgical coverage. Int Agency Prev Blind. 2015;2:1–25.
5. Gutu SZ S C A the 2007 population and housing census of Ethiopia; 2008.
6. Gower EW, Berhane Y, Worku A, et al. Prevalence and causes of blindness and low vision in Ethiopia prevalence and causes of blindness and low vision in. EthiopJHealth Dev. 2008;21(3):205–209.
7. Abateneh A, Tesfaye M, Bekele S, Gelaw Y, Wedrich A. Vision loss and psychological distress among Ethiopians adults: a comparative cross-sectional study. PLoS One. 2013;8(10):e78335. doi:10.1371/journal.pone.0078335
8. Polack S, Eusebio C, Mathenge W, et al. The impact of cataract surgery on activities and time-use: results from a longitudinal study in Kenya, Bangladesh and the Philippines. PLoS One. 2010;5(6):e10913. doi:10.1371/journal.pone.0010913
9. Polack S, Kuper H, Mathenge W, Fletcher A, Foster A. Cataract visual impairment and quality of life in a Kenyan population. Br J Ophthalmol. 2007;91(7):927. doi:10.1136/bjo.2006.110973
10. Polack S, Eusebio C, Fletcher A, Foster A, Kuper H. Visual impairment from cataract and health related quality of life: results from a case-control study in the Philippines. Ophthalmic Epidemiol. 2010;17(3):152–159. doi:10.3109/09286581003731536
11. Kuper H, Polack S, Eusebio C, Mathenge W, Wadud Z, Foster A. A case-control study to assess the relationship between poverty and visual impairment from cataract in Kenya, the Philippines, and Bangladesh. PLOS Med. 2008;5(12):e244. doi:10.1371/journal.pmed.0050244
12. Kuper H, Polack S, Mathenge W, et al. Does cataract surgery alleviate poverty? Evidence from a multi-centre intervention study conducted in Kenya, the Philippines and Bangladesh. PLoS One. 2010;5(11):e15431. doi:10.1371/journal.pone.0015431
13. Glick P, Luoto J, Orrs MS, et al. The individual and household impacts of cataract surgery on older blind adults in Ethiopia. Ophthalmic Epidemiol. 2019;26(1):7–18. doi:10.1080/09286586.2018.1504310
14. World Health Organization. World Report on Vision. Vol. 214. World health Organization; 2019:1–160.
15. Burton WHDAFMJ. What are the priorities for improving cataract surgical outcomes in Africa ? Results of a Delphi exercise. Int Ophthalmol. 2017;2017:1.
16. World Health Organization WHO informal consultation on analysis of blindness prevention outcomes (1998: Geneva, Switzerland) & WHO programme for the prevention of blindness and deafness. Informal Consultation on Analysis of Blindness Prevention Outcomes, Geneva, 16–18 16–18 February 1998. World Health Organization; 1998:23. Available from: https://apps.who.int/iris/handle/10665/67843.
17. Lewallen S, Schmidt E, Jolley E, et al. Factors affecting cataract surgical coverage and outcomes: a retrospective cross-sectional study of eye health systems in sub-Saharan Africa. BMC Ophthalmol. 2015;15(1):1–8. doi:10.1186/s12886-015-0063-6
18. Aliyu H, Mustak H, Cook C. Using the postoperative visual acuity to monitor the quality of cataract surgery: does the day one visual acuity following cataract surgery correlate with the final visual acuity ? Middle East Afr J Ophthalmol. 2017;24(2):91–93. doi:10.4103/meajo.MEAJO_279_16
19. Lindfield R. Measuring the outcome of cataract surgery: the importance of the patient perspective. Commu Eye Heal J. 2015;28(89):2–4.
20. Boerma T, AbouZahr C, Evans D, Evans T. Monitoring intervention coverage in the context of universal health coverage. PLoS Med. 2014;11(9):e1001728. doi:10.1371/journal.pmed.1001728
21. Universal Health Coverage Overview; 2022. Available from: https://www.worldbank.org/en/topic/universalhealthcoverage.
22. Khachatryan N Outcomes of Cataract Surgery and Predictors of Poor Outcome in Lions Regional Ophthalmic Unit; 2018. Available from: http://aua.am/chsr/PDF/MPH/2009/Nalbandyan,Marine.pdf.
23. Nalbandyan M, Petrosyan V. Outcomes of cataract surgery and predictors of poor outcome in lions regional ophthalmic unit. Am Univ Armen Sch Public Heal Garo Meghrigian Inst Prev Ophthalmol; 2009. Available from: http://auachsr.com/PDF/MPH/2009/Nalbandyan,Marine.pdf.
24. Ilechie AA, Boadi-kusi BS, Ndudiri OV, Ofori EA. Evaluation of post-operative visual outcomes of cataract surgery in Ghana. Int J Heal Res. 2012;5(1):35–42.
25. Sonron EA, Tripathi V, Bridgemohan P. A retrospective study on the outcomes of cataract surgery in an eastern regional health authority hospital of Trinidad and Tobago. PeerJ. 2015;3:1–13.
26. Desta K, Yoseph S, Assefa Y. Visual outcome and associated factors of patients who underwent age related cataract surgery at University of Gondar, Referral Hospital, Northwest Ethiopia. J Adv Med. 2014;1(1):17–26.
27. Thanigasalam T, Reddy SC. Factors Associated with complications and postoperative visual outcome in cataract patients: a study of 1632 cases. J Ophthalmic Vis Res. 2015;10(1):1–10. doi:10.4103/2008-322X.156082
28. Habtamu E, Eshete Z, Burton MJ. Cataract surgery in Southern Ethiopia: distribution, rates and determinants of service provision. BMC Health Serv Res. 2013;13(480):1–12. doi:10.1186/1472-6963-13-480
29. Ntim-Amponsah CT, Amoaku WMK, Ewusi RK, Idirisuriya-Khair R, Nyatepe-Coo E, Ofosu-Amaah S. Evaluation of risk factors for advanced glaucoma in Ghanaian patients. Eye. 2005;19(5):528–534. doi:10.1038/sj.eye.6701533
30. Thanigasalam T, Reddy S, Zaki R. Factors associated with complications and postoperative visual outcomes of cataract surgery; A study of 1632 cases. J Ophthalmic Vis Res. 2015;10(4):375. doi:10.4103/2008-322X.158892
31. Zelalem A. Patients’ preoperative expectation and outcome of cataract surgery at Jimma University specialized hospital -department of ophthalmology. Ethiop J Heath Sci. 2011;12(1):1.
32. Limburg H. Monitoring cataract surgical outcomes: methods and tools. J Community Eye Heal. 2002;15(44):51–53.
33. Matta S, Park J, Palamaner G, et al. Cataract surgery visual outcomes and associated risk factors in secondary level eye care centers of L V Prasad eye institute, India. PLoS One. 2016;11(1):e0144853. doi:10.1371/journal.pone.0144853
34. Seid M, Legesse K, Assen M, Tilahun G. mohammmed seid husse, kbrom legese gebreselassie Mohammed Assen and Getachew tilahun. Visual outcome of cataract surgery at Gondar University Hospital Tertiary Eye Care and. Clin Optom. 2017;9:19–23. doi:10.2147/OPTO.S122953
35. Elmoddather M. A comparative study between manual small incision cataract surgery, planned extracapsular cataract extraction and phacoemulsification in mature cataract cases. J Am Sci. 2016;10(10):1.
36. Kshitiz K, Vp G, Dhaliwal U. Original articles Causes of sub-optimal cataract surgical outcomes in patients. Nepa J Ophthalmol. 2012;4(7):73–79.
37. Twinamasiko PA Outcomes of Cataract Surgery. Uganda; 2013.
38. Farzeen KH, Qazi AK. Visual outcome of cataract surgery. J Coll Physicians Surg Pakistan. 2013;23(6):448–449.
39. El-Shafy E, El-Sayed S, El-Sobky H, Badawy N. Phacoemulsification versus manual small incision cataract surgery for treatment of cataract. Menoufia Med J. 2015;28(1):191. doi:10.4103/1110-2098.155987
40. Venkatesh R, Tan CSH, Sengupta S, Ravindran RD, Krishnan KT, Chang DF. Phacoemulsification versus manual small-incision cataract surgery for white cataract. J Cataract Refract Surg. 2010;36(11):1849–1854. doi:10.1016/j.jcrs.2010.05.025
41. Khanna R, Pujari S, Sangwan V. Cataract surgery in developing countries. Curr Opin Ophthalmol. 2011;22(1):10–14. doi:10.1097/ICU.0b013e3283414f50
42. Gogate P, Optom JJB, Deshpande S, Naidoo K. Meta-analysis to compare the safety and efficacy of manual small incision cataract surgery and phacoemulsification. Middle East Afr J Ophthalmol. 2015;22(3):362–369. doi:10.4103/0974-9233.159763
43. Khanna RC, Kaza S, Shantha GPS, Sangwan VS. Comparative outcomes of manual small incision cataract surgery and phacoemulsification performed by ophthalmology trainees in a tertiary eye care hospital in India: a retrospective cohort design. BMJ Open. 2012;2(5):e001035. doi:10.1136/bmjopen-2012-001035
44. Ramakrishnan R, Shah P, Shrivastava S, Parikh D, Kadu A. Comparison of corneal changes between SICS and phacoemulsification. Int J Ocul Oncol Oculoplasty. 2017;3(1):50–53.
45. El-sayed SH, El-sobky HMK, Badawy NM, El-shafy EAA. Phacoemulsification versus manual small incision cataract surgery for treatment of cataract. Menoufia Med J Demands. 2015;2015:191–196.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
