Back to Journals » International Medical Case Reports Journal » Volume 16
Case Report: A Closed Loop Obstruction Secondary to Idiopathic Small Bowel Intussusception in an Elderly Woman
Authors Aregawi AB , Girma A
Received 22 November 2022
Accepted for publication 20 January 2023
Published 28 January 2023 Volume 2023:16 Pages 65—72
DOI https://doi.org/10.2147/IMCRJ.S398426
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Ronald Prineas
Alazar Berhe Aregawi,1 Abdulkerim Girma2
1Department of Surgery, Hawassa University Comprehensive Specialized Hospital, Hawassa University, Hawassa, Sidama, Ethiopia; 2Department of Radiology, Yanet Internal Medicine Specialized Centre, Hawassa, Sidama, Ethiopia
Correspondence: Alazar Berhe Aregawi, Tel +251911914624, Email [email protected]
Abstract: Intussusception is primarily a disease of children and is the primary cause of intestinal obstruction in the pediatric age group. It accounts for around 5– 16% of cases of intestinal obstruction in adults of the western population. Most cases of adult intussusception (up to 90%) are secondary to an identified structural lesion or a lead point contrary to pediatric intussusception. Adults with intussusception present with subacute or chronic symptoms of partial obstruction. CT is the best imaging to make a preoperative diagnosis of adult intussusception. The standard treatment for adult intussusception is surgery, and non-operative reduction should not be attempted. Here, we present a rare case of idiopathic small bowel intussusception in a 50-year-old woman. She presented with crampy abdominal pain for one-week duration. It was associated with frequent vomiting of bilious matter. She claimed to have had similar symptoms for the past 2 months and had repeatedly visited nearby health facilities. She had an abdominal CT, which suggested a complicated small bowel intussusception. Exploratory laparotomy was done, and there was a small bowel intussusception and an inflammatory stricture at the end of the intussusceptum, which is believed to form a closed-loop like obstruction. The intussusceptum was resected en-bloc then end-to-end jejuno-jejunal anastomosis was performed. This case report makes physicians aware of this rare condition in adults. So that they have a high index of suspicion when a patient presents with symptoms of subacute or chronic intestinal obstruction and inform that abdominal CT should be done in these circumstances and surgery is the mainstay of treatment. Our case is unique, and there is no report in the literature similar to ours.
Keywords: intussusception, adult, small bowel intussusception, small bowel obstruction
Introduction
Intussusception is primarily a disease of children and is the primary cause of intestinal obstruction in the pediatric age group.1–6 It accounts for around 5–16% of cases of intestinal obstruction in adults of the western population.1,3,7–11 It occurs when a segment of the bowel, the intussusceptum, telescopes into the adjacent segment of the bowel, the intussuscipiens.1,3,7,10–14 Only 5% of intussusceptions occur in adults.2,4,5,7,12,15 Adult intussusception occurs in the age range b/n the second and ninth decade. In many reports, the most typical age is in the fifth decade. There is no sex predilection for adult intussusception.1,3,16,17
Intussusceptions can be classified as enteroenteric (jejuno-jejunal, jejuno-ileal or ileo-ileal), enterocolic (ileo-colic or ileo-cecal), colocolic, or sigmoidorectal (involves the sigmoid colon and the rectum).1,3,7,12,18 More than 90% of adult intussusceptions occur in the small or large bowel; the remaining occurs in surgically created stomas or the stomach.3,4,16,18 The most common location is the small bowel.3,10,13,17–19
Most cases of adult intussusception (up to 90%) are secondary to an identified structural lesion or a lead point contrary to pediatric intussusception.1–6,8,9,11–13,15,20 Neoplasia is the primary lesion identified in around 2/3rd cases of adult intussusception. More than 60% of these are malignant.1,9 Around 25% of cases of adult intussusception are secondary to benign tumors.8 Recent studies show that 60% of small bowel intussusceptions are benign, 30% are malignant, and about 10% are idiopathic.3,8,10,16
There is a significant difference between pediatric and adult intussusception regarding the cause, clinical presentation, diagnosis, and management.1 Clinical diagnosis of adult intussusception is challenging because of its rarity, the manifestations are non-specific, and diagnosis is often made at laparotomy.1,3,7,9,10,12,17 CT is the best imaging to diagnose adult intussusception.10
This is unlike the case with pediatric intussusception, where the presentation is acute with abdominal pain or bloody diarrhea. Adults present with subacute or chronic symptoms of partial obstruction.1,2,7,10 The most frequent presenting symptom is crampy abdominal pain, seen in about 75% to 85% of patients.1,9,16–19 Other symptoms include nausea and vomiting. Bleeding and abdominal mass are rare presentations.1,12,19
The standard treatment for adult intussusception is surgery, and non-operative reduction should not be attempted.8
We report a case of closed-loop obstruction secondary to idiopathic small bowel intussusception and inflammatory stricture. There is no similar report in the literature. This case report makes physicians aware of this rare condition in adults. So that they have a high index of suspicion when a patient presents with symptoms of subacute or chronic intestinal obstruction and inform that abdominal CT should be done in these circumstances and surgery is the mainstay of treatment.
Case Description
We present the case of a 50-year-old woman who came to Hawassa University Comprehensive Specialized Hospital with a referral paper from a private hospital in the city. She presented with crampy abdominal pain of a one-week duration. It was associated with frequent vomiting of bilious matter. Two days previously, she had failed to pass faeces and flatus. She had mild abdominal distension. She claimed to have had similar symptoms for the past 2 months and had repeatedly visited nearby health facilities. She was given IV medication and fluid and was sent home.
Her past medical history was unremarkable.
Physical Examination
She looked acutely sick V/S Pulse rate-115 Respiratory rate-24 Temp.-Afebrile to touch Blood pressure-100/70 mmHg. On HEENT-she had slightly pale conjunctiva and dry buccal mucosa. On abdominal examination- the abdomen was slightly distended, and there was marked tenderness over the epigastric area. The rest of the abdominal examination looked normal. Examination of the rest of the system was normal.
Investigation
On Serology
Complete blood count- White cell count=12.8x103/uL Granulocyte=78.9% Lymphocyte=10.1% -Hgb=10.3 g/dl HCT-33.1 Platelet= 282×103 Bg&Rh=o+ Fasting blood sugar, Blood urea nitrogen, Creatinine, ALP, AST, ALT, and Serum electrolytes were normal.
On Imaging
Abdominal Ultrasound
Distended bowel loops in the upper abdomen measuring up to 8 cm in diameter with marked wall thickening measuring up to 1.5 cm. There are reverberation artifacts seen within the thickened wall suggestive of air (Pneumatosis intestinalis).
Abdominopelvic CT with IV Contrast
There is a long segment (more than 30cm), small bowel intussusception and wall thickening of proximal small bowel loops (jejunal loops). The involved bowel segment has intramural air and decreased contrast enhancement. The supplying artery (branch of the superior mesenteric vessel) is attenuated at its entry point. Proximal small bowel loops were dilated. In conclusion, there was a proximal small bowel (jejunal) long segment intussusception with pneumatosis intestinalis (likely gangrenous) and proximal small bowel obstruction. See Figure 1A–E
The patient was resuscitated with around 4 L of N/S, catheterized, NG tube inserted and taken to the OR for exploration. The abdomen was cleaned and draped, then entered through a vertical midline incision. The proximal small bowel was significantly distended with thickened bowel wall. An intussusception extends from the jejunum about 30cm distal to the ligamentum treitz and extends up to 180 cm proximal to the ileo-cecal junction. Portions of the intussusceptum looked necrotic. No reduction was attempted, the intussusceptum was resected en-bloc, and end-to-end jejuno-jejunal anastomosis was performed. See Figures 2 and 3 There was a marked lumen discrepancy between the proximal and distal segments. No lead point was identified. There was no mesenteric LAP. The rest of the bowel looked normal. Thorough lavage with warm saline was done, and the wound closed in layers after the count was declared correct. The resected bowel was opened up and examined, there was no identifiable mass, and a large segment of the small bowel was intussuscepted. At the distal end, there was a strictured segment of the bowel. It appears to be responsible for the distension of the intussusceptum and the primary cause of obstruction. Intraoperatively the patient was transfused with 1 unit of X-matched blood. The patient was safely transferred to recovery. The resected bowel was sent for pathological examination. See Figures 4A and B The patient had an uneventful post-operative course, and she was discharged on the sixth post-operative day. She was seen on the second and fourth month post-op and was doing fine.
 |
Figure 2 Intraoperative picture of the intussusception. |
 |
Figure 3 The resected Intussusceptum. |
Biopsy Report
-Section shows jejunal tissue lined by bland mucosal glands with a large area of surface ulceration, necrosis, extravasated hemorrhage and fibrin. The lamina propria was infiltrated by mixed inflammatory cells. See Figure 5
 |
Figure 5 Section shows mucosal ulceration, hemorrhage and necrosis which are features of transmural hemorrhagic infarction. |
-Section from the constricted segment see Figure 6, shows ulcerated mucosa, transmural intense neutrophilic infiltrates and thick collagen bundles in the lamina propria and submucosal layer. No features of malignancy or granuloma seen.
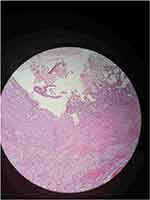 |
Figure 6 Section taken from narrowed segment shows ulcerated mucosa and transmural neutrophilic infiltration. |
Discussion
Adult intussusception is a rare surgical condition.2,8,9,12,15–17 The overall incidence of adult intussusception is 2–3 cases/1,000,000 of the general population per year.6,16,18 Malignancy is noted when it is colonic intussusception accounting for more than 65% of cases.1,2,5–7 In the small bowel, the common malignant lead point is metastasis.1,3,6,19
It has been reported that 8–20% of adult intussusceptions are idiopathic and are primarily enteroenteric type.2,7,15,18 In Tropical countries, there is a higher frequency of adult intussusception compared to the western figure, and malignant causes are less common. And the proportion of idiopathic cases is high.1,19,21 This higher incidence is due to the high prevalence of diarrheal diseases, believed to alter bowel peristalsis and result in intussusception.1,21 No associated pathology was identified in about 2/3rd of cases of adult intussusception in a study conducted in Papua, New Guinea.1 In this study, there was no identified lead point so we considered it idiopathic.
According to several reports, a definitive preoperative diagnosis of intussusception was made only in 32–50% of cases.1,6,18 Plain abdominal X-ray lacks the specificity and sensitivity to diagnose adult intussusception, although it can identify whether there is an intestinal obstruction or not.3,16 Unlike the case with the pediatric population, there is a limitation to abdominal ultrasound to diagnose adult intussusception as gaseous distension of bowels and body habitus of the patient can obscure the imaging.3,7,12,16 This was the case with our patient, the abdominal ultrasound was inconclusive. The preoperative accuracy of abdominal ultrasound is around 60%. The accuracy increases when there is a palpable abdominal mass.7
The Target and doughnut signs on transverse views, and the pseudokidney sign on longitudinal views are classical findings of intussusception on abdominal ultrasound.3,7
Recently, abdominal CT has been the preferred imaging modality to diagnose adult intussusception, with its diagnosing accuracy reaching up to 58–100%.1,3,6,7,16,19 On a CT scan, an intussusception length of less than or equal to 3.5 cm is said to be self-limiting and does not require surgery.3,20 CT can demonstrate the site of intussusception and assess bowel viability well. It can provide valuable information regarding underlying pathology-like regional lymphadenopathy or a mass.7 Our patient had an abdominal CT that identified a proximal small bowel/jejunal/intussusception which was complicated with features of pneumatosis intestinalis and the estimated length of the intussusception was more than 30 cm.
Most adult intussusceptions present with intestinal obstruction.7,10 This was the case in our patient. The treatment of adult intussusception is primarily surgical, in contrast to pediatric cases. This has been recommended by many authors, including those in sub-Saharan Africa.1–3,7 Whether to do reduction or not before resection is controversial in the case of enteric intussusceptions but in colonic intussusceptions because there is a high likelihood of malignancy manipulation should be avoided as there is a high risk of venous dissemination of malignancy, peritoneal soiling, perforation and seeding in areas of ulcerated mucosa. So straightforward resection is recommended.1–3,5,8–10,12,17,19
En-bloc resection is recommended in enteroenteric intussusception with suspected malignancy as the underlying pathology or when a large segment of the small bowel is not going to be resected.2,7 Some authors recommend doing a simple reduction in cases of post-traumatic or idiopathic small bowel intussusceptions making sure that there are no signs of ischemia or perforations. Given the rarity of this form of intussusception, this experience is very low.3,18,19 In our case, there were areas of necrosis in the obstructed segment, so we did an en-bloc resection which is in accordance with the recommendations.
The morbidity of adult intussusception includes intestinal necrosis, perforation or septic shock, which is related to a diagnosis delay. In our intraoperative finding, there were areas of intestinal necrosis which is evident for a delay in the diagnosis though the patient had visited health facilities repeatedly before presenting to us. This can result in a mortality rate of 0–2%.9 Data are lacking regarding the risk of recurrence after treatment of adult intussusception.1
Conclusion
Due to its rarity and non-specific symptoms, preoperative diagnosis of small bowel intussusception in adults is extremely difficult, and a high index of suspicion is essential. Complications such as intestinal necrosis and perforation can result from a delayed diagnosis. A CT of the abdomen is crucial for making an early, definitive diagnosis. Surgery remains the treatment of choice. Due to the patient’s idiopathic type of small bowel intussusception and the inflammatory stricture that resulted in a closed-loop type of small bowel obstruction, our case is quite unique.
Data Sharing Statement
The data used to support the findings of this study will be available from the corresponding author upon reasonable request.
Ethical Review
After receiving permission from the Hawassa University Institutional Review Board (IRB), the patient provided written informed consent for the publication of this case report. The consent included case-specific information and images.
Acknowledgment
The authors would like to thank Dr Gedion Getachew, a second year surgical resident in Hawassa University Comprehensive Specialized Hospital, for the nice intraoperative pictures. And they would like to express sincere gratitude to Dr Abebe melis, a pathologist, and Dr Selamawit G/Egziabher a third year pathology resident in Hawassa University Comprehensive Specialized Hospital, who did a great job preparing the pathologic slides. Moreover, we would like to thank our patient who allowed us to undertake this case report.
Disclosure
The authors declare no conflicts of interest for this work.
References
1. Huang BY, Warshauer DM. Adult intussusception: diagnosis and clinical relevance. Radiol Clin North Am. 2003;41(6):1137–1151. doi:10.1016/S0033-8389(03)00116-7
2. Ongom PA, Opio CK, Kijjambu SC. Presentation, aetiology and treatment of adult intussusception in a tertiary sub-saharan hospital: a 10-year retrospective study. BMC Gastroenterol. 2014;14(1):1–8. doi:10.1186/1471-230X-14-86
3. Potts J, Al Samaraee A, El-Hakeem A. Small bowel intussusception in adults. Ann R Coll Surg Engl. 2014;96(1):11–14. doi:10.1308/003588414X13824511650579
4. Agha P. Review Intussusception in Adults. AJR. 1985;1985:527–531.
5. Sarma D, Prabhu R, Rodrigues G. Adult intussusception: a six-year experience at a single center. Ann Gastroenterol. 2012;25:128–132.
6. Manouras A, Lagoudianakis EE, Dardamanis D, et al. Lipoma induced jejuno-jejunal intussusception. World J Gastroenterol. 2007;13(26):3641–3644. doi:10.3748/wjg.v13.i26.3641
7. Wang N, Cui XY, Liu Y, et al. Adult intussusception: a retrospective review of 41 cases. World J Gastroenterol. 2009;15(26):3303–3308. doi:10.3748/wjg.15.3303
8. Renzulli P, Candinas D. Idiopathic small bowel intussusception in an adult. Cmaj. 2010;182(3):90457. doi:10.1503/cmaj.090457
9. Traoré D, Sissoko F, Ongoïba N, Traoré I, Traoré AK, Koumaré AK. Invagination intestinale aiguë chez l’adulte: écueils diagnostiques, morbidité et mortalité dans un pays en voie de développement. J Chir Viscerale. 2012;149(3):231–234. doi:10.1016/j.jchirv.2011.12.010
10. Siow SL, Mahendran HA. A case series of adult intussusception managed laparoscopically. Surg Laparosc Endosc Percutaneous Tech. 2014;24(4):327–331. doi:10.1097/SLE.0000000000000006
11. Dollinger M, Bäumler W, Brunner SM, et al. Role of clinical and CT findings in the identification of adult small bowel intussusception requiring surgical intervention. BJS Open. 2021;5:5. doi:10.1093/bjsopen/zrab076
12. Cakir M, Tekin A, Kucukkartallar T, Belviranli M, Gundes E, Paksoy Y. Intussusception: as the cause of mechanical bowel obstruction in adults. Korean J Gastroenterol. 2013;61(1):17–21. doi:10.4166/kjg.2013.61.1.17
13. Correia de Sá T, Ferreira AI, Barreto F, Santos M. Jejunal intussusceptions due to metastatic malignant melanoma: a case report. J Surg Case Reports. 2021;2021(1):1–3.
14. Rosa ML, Roque A, Ferreira P. Closed-loop obstruction caused by double intussusception in an adult. Gaz Médica. 2022;9:2021–2023.
15. Begos DG, Sandor A, Modlin IM. The diagnosis and management adult intussusception. Am J Surg. 1997;173(2):88–94. doi:10.1016/S0002-9610(96)00419-9
16. Aref H, Nawawi A, Altaf A, Aljiffry M. Transient small bowel intussusception in an adult: case report with intraoperative video and literature review. BMC Surg. 2015;15(1). doi:10.1186/s12893-015-0020-6
17. Eisen LK, Cunningham JD, Jr AHA. Intussusception in adults: institutional review. J Am Coll Surg. 1999;7515(98):390–395. doi:10.1016/S1072-7515(98)00331-7
18. Yalamarthi S, Smith RC. Adult intussusception: case reports and review of literature. Postgrad Med J. 2005;81:174–177. doi:10.1136/pgmj.2004.022749
19. Hong KD, Kim J, Ji W, Wexner SD. Adult intussusception: a systematic review and meta-analysis. Tech Coloproctol. 2019;23(4):315–324. doi:10.1007/s10151-019-01980-5
20. Lvoff N, Breiman RS, Coakley FV, Lu Y, Warren RS. Distinguishing features of self-limiting adult small bowel intussusception identified at CT. Radiology. 2003;227(1):68–72. doi:10.1148/radiol.2272020455
21. Simpson RL. Adult intussusception in the tropics. J Br Surg. 1983;70:1983.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


