Back to Journals » Vascular Health and Risk Management » Volume 10
Cardiac angiosarcoma: utility of [18F]fluorodeoxyglucose positron emission tomography–computed tomography in evaluation of residue, metastases, and treatment response
Authors Tokmak H, Demir N, Demirkol MO
Received 18 March 2014
Accepted for publication 14 April 2014
Published 27 June 2014 Volume 2014:10 Pages 399—401
DOI https://doi.org/10.2147/VHRM.S64286
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Handan Tokmak,1 Nurhan Demir,2 Mehmet Onur Demirkol3
1Department of Nuclear Medicine and Molecular Imaging, American Hospital, Nisantasi, Istanbul, 2Internal Medicine Department, Cerrahpasa Medical Faculty, Istanbul University, Istanbul, 3Department of Nuclear Medicine and Molecular Imaging, Koç University, Istanbul, Turkey
Abstract: Cardiac angiosarcomas are a rare form of malignancy. The majority of cases arise from the right atrium as mural masses. These tumors have extremely aggressive behavior, with early clinical symptoms that vary depending on location, size, and extent of the tumor. Most of these patients have a very short survival time. Surgical therapy is considered the best choice of therapy approach in cardiac angiosarcoma patients with nonmetastatic disease, even though the disease is rarely cured. Advanced diagnostic techniques facilitate accurate, noninvasive assessments of cardiac sarcomas. We report a case of a 62-year-old man with cardiac angiosarcoma who had multiple distant metastases that were revealed by [18F]fluorodeoxyglucose positron emission tomography–computed tomography imaging.
Keywords: primary cardiac angiosarcoma, FDG PET/CT imaging, noninvasive assessment of cardiac sarcomas
Introduction
Sarcoma is the most common primary malignancy of the heart and pericardium. Primary cardiac sarcomas are rare entities,1–3 with an autopsy prevalence of 0.001%–0.28%.3 Pathologic subtypes of primary cardiac sarcoma are angiosarcoma fibrosarcoma, rhabdomyosarcoma, malignant schwannoma, and mesothelioma. Frequency rate decreases in adults.
Angiosarcoma frequency is less than 1% among sarcomas. Of all angiosarcomas, a primary angiosarcoma of the heart and the great vessels accounts for only 3%.4 Most of cardiac angiosarcomas (80%) originate from right atrium as mural masses. Extension to the pericardium and encasement of the heart may be seen, and usually fills the entire cardiac chamber. The aggressive behavior of cardiac angiosarcomas causes early symptoms and a very short survival rate. Clinical presentation of sarcomas varies depending on the location, size, and extent of the tumor. Advanced diagnostic techniques facilitate accurate, noninvasive assessment of cardiac sarcomas.5
Diagnostic workup usually includes standard echo contrast-enhanced computed tomography (CT), magnetic resonance imaging, and angiography. In the literature, a few case reports have demonstrated the diagnostic contribution of [18F]fluorodeoxyglucose (FDG) positron emission tomography (PET)-CT in the evaluation of the malignant nature of disease and staging before deciding on the therapy aproach.6,7
Even though cardiac angiosarcoma is rarely cured, surgical therapy is considered the best choice of therapy in nonmetastatic disease.8 Complete or partial surgical resection of primary or metastatic cardiac sarcoma can provide significant hemodynamic improvement, successful palliation, and prolonged survival.9,10 Chemotherapy and postsurgical adjuvant radiotherapy have not proven consistently beneficial. However, all treatment choices after surgical resection can ameliorate symptoms with a varied response.11
Case report
Herein, we report the case of a 62-year-old man who had previously undergone tumor resection for primary high-grade cardiac angiosarcoma (Figure 1) at a university hospital 4 months previously. The patient was referred to the Nuclear Medicine Department for 18F-FDG PET-CT imaging to assess residual and/or metastatic disease.
  | Figure 1 Histopathology findings. |
The tumor was surgically approached by medial sternotomy, but complete tumor resection was not possible because of the extensive tumor infiltration. Palliative intervention consisting of partial excision of the tumor mass was aimed at releasing the right ventricular outflow tract.
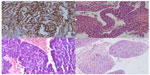
PET-CT scans revealed a residual or relapsed mass in the right atrium, with significantly increased uptake of 18F-FDG (maximum standardized uptake value of 12). The mass extended to the mitral valve, septum, and left ventricle and infiltrated to the pericardium and adjacent mediastinum (Figure 2). The mass encased and almost completely replaced the atrial wall and nearly filled the entire cardiac chamber. Increased activity in the sternum was concomitant with sternotomy. PET-CT images also revealed multiple distant metastasis in the lung, liver, and bones (Figure 3). Despite receiving subsequent aggressive therapy, including radiotherapy, the patient died 8 months later.
  | Figure 2 18F-FDG PET-CT image showing the tumor mass in the right atrium. |
Conclusion
Angiosarcoma is a very aggressive malignant neoplasm with a short fatal clinical process, despite new, cutting edge, treatment modalities, such as extensive surgery, radiotherapy, and chemotherapy.12 Nowadays, through advanced diagnostic technology, such as high-resolution CT, dynamic magnetic resonance imaging, and PET-CT, clinicians are able to diagnose in a shorter time, which allows for more effective radical surgical resection. 18F-FDG PET-CT seems to be an effective and feasible imaging modality to evaluate primary or postsurgical residue and/or relapse and metastases of the tumor.
Disclosure
The authors report no conflicts of interest in this work.
References
Reynen K. Frequency of primary tumors of the heart. Am J Cardiol. 1996;77:107. | |
Silverman NA. Primary cardiac tumors. Ann Surg. 1980;191:127–138. | |
Barreiro M, Renilla A, Jimenez JM, et al. Primary cardiac tumors: 32 years of experience from a Spanish tertiary surgical center. Cardiovasc Pathol. 2013;22;424–427. | |
Lantz DA, Dougherty TH, Lucca MJ. Primary angiosarcoma of the heart causing cardiac rupture. Am Heart J. 1989;118:186–188. | |
Yuan SM, Shinfeld A, Lavee J, Kuperstein R, Haizler R, Raanani E. Imaging morphology of cardiac tumours. Cardiol J. 2009;16:26–35. | |
Hori Y, Funabashi N, Miyauchi H, et al. Angiosarcoma in the right atria demonstrated by fusion images of multislice computed tomography and positron emission tomography using F-18 fluoro-deoxyglucose. Int J Cardiol. 2007;123:e15–e17. | |
Higashiyama S, Kawabe J, Hayashi T, et al. Effectiveness of preoperative PET examination of huge angiosarcoma of the heart. Clin Nucl Med. 2009;34:99–102. | |
Truong PT, Jones SO, Martens B, et al. Treatment and outcomes in adult patients with primary cardiac sarcoma: the British Columbia Cancer Agency experience. Ann Surg Oncol. 2009;16:3358–3365. | |
Reardon MJ, Walkes JC, Benjamin R. Therapy insight: malignant primary cardiac tumors. Nat Clin Pract Cardiovasc Med. 2006;3:548–553. | |
Furukawa N, Gummert J, Börgermann J. Complete resection of undifferentiated cardiac sarcoma and reconstruction of the atria and the superior vena cava: case report. J Cardiothorac Surg. 2012;7:96. | |
Kakizaki S, Takagi H, Hosaka Y. Cardiac angiosarcoma responding to multidisciplinary treatment. Int J Cardiol. 1997;62:273–275. | |
Look Hong NJ, Pandalai PK, Hornick JL, et al. Cardiac angiosarcoma management and outcomes: 20-year single-institution experience. Ann Surg Oncol. 2012;19(8):2707–2715. |
 © 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.