Back to Journals » Clinical Ophthalmology » Volume 16
Canaloplasty and Trabeculotomy Ab Interno Combined with Cataract Surgery: 12-Month Outcomes in Hispanic Patients with Open-Angle Glaucoma
Authors Gallardo MJ , Dhamdhere K, Dickerson JE Jr
Received 18 January 2022
Accepted for publication 15 March 2022
Published 24 March 2022 Volume 2022:16 Pages 905—908
DOI https://doi.org/10.2147/OPTH.S358878
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Mark J Gallardo,1 Kavita Dhamdhere,2,3 Jaime E Dickerson Jr2,4
1El Paso Eye Surgeons, PA, El Paso, TX, USA; 2Sight Sciences Inc., Menlo Park, CA, USA; 3Mahatma Gandhi Medical College and Research Center, Wardha, India; 4North Texas Eye Research Institute, University of North Texas Health Science Center, Fort Worth, TX, USA
Correspondence: Jaime E Dickerson Jr, Email [email protected]
Introduction
Between 2010 and 2019, the Hispanic demographic increased in the US from 16% to 18%. Hispanic ethnicity accounted for 52% of US population growth over this period.1 By 2035, Hispanic males will be the largest primary open-angle glaucoma (POAG) demographic; by 2050, Hispanics will account for 50% of POAG.2 Glaucoma in the Hispanic population is more prevalent than for non-Hispanic Whites with a higher proportion undiagnosed.3 While the Hispanic demographic is growing there remains much to be learned regarding specific risk factors for OAG in this population and how they may differ between the Hispanic and non-Hispanic White demographics.4 Population differences may have an effect on response to medical or surgical therapeutics therefore it is important to understand effectiveness and safety of glaucoma therapeutics within this significant demographic. Published data regarding the performance of various minimally invasive glaucoma surgeries in the Hispanic population remains relatively sparse. This study reports 12-month outcomes for canaloplasty followed by trabeculotomy (OMNI Surgical System, Sight Sciences, Menlo Park, CA) in conjunction with cataract surgery in a Hispanic (Northern Mexico/mestizo) open-angle glaucoma (OAG) population from El Paso, Texas.
Methods
Patients were enrolled at a tertiary referral glaucoma center as part of the multicenter 12-month GEMINI study (NCT03861169). The study was reviewed and approved by the IRB (Aspire). All patients provided written informed consent. The study followed the tenets of the Declaration of Helsinki. Study design and eligibility criteria have been previously described.5 In brief, key inclusion and exclusion criteria were: Hispanic ethnicity, adults aged 22 years or older, visually significant cataract, and mild to moderate open-angle glaucoma (ICD-10 guidelines), medicated IOP <33 mmHg on 1–4 topical IOP-lowering medications and unmedicated mean diurnal IOP (after washout) 21–36 mmHg and at least 3 mmHg higher than screening IOP, Schaffer grade ≥3 in all four quadrants by gonioscopy, no laser trabeculoplasty within 3 months of enrollment, or any prior glaucoma surgery (trabeculectomy, tube-shunt, or any MIGS procedure). Race/ethnicity information was self-reported. Eligible patients underwent medication washout preoperatively and at month 12. Diurnal IOP (DIOP; 9 AM, 12 PM, 4 PM) was measured preoperatively and 12 months. All IOP measurements were with Goldmann tonometer. Following phacoemulsification cataract surgery through a clear corneal incision (CCI, ≤ 2 mm), canaloplasty and trabeculotomy (360/180 degree) was performed using the same CCI for access. No IOP-lowering medications were administered to patients after the surgery (0 meds on postop day 1) unless medically warranted. If during the follow-up period medication was required to manage IOP, the same medication class (es) as used preoperatively were re-introduced with no more than one ocular hypotensive agent added at a single visit or within a 2-week period. Effectiveness outcomes included mean IOP and medications. Safety included adverse events (AE), and secondary surgical interventions (SSI). Analysis includes descriptive statistics and Mann–Whitney tests evaluating change from baseline.
Results
Thirty-nine subjects were treated and followed 12 months (March 2019 - April 2021). Demographics aside from ethnicity were similar to those for the GEMINI study as a whole; mean age and percentage female were 68.3 years, 60% in GEMINI and 69.2 years, 51% in this subset. Average [SD} Visual Field Mean Deviation and Pattern Standard Deviation were −3.9 [3.5] dB and 3.2 [2.1] dB compared to −3.7 [3.6] dB and 3.7 [2.6] dB for the GEMINI study as a whole. Note that nearly all (39/41, 95%) of subjects self-reporting as Hispanic in the GEMINI study are included in the present single-center analysis. Prior to washout, mean IOP was 16.5 (2.8) mmHg on average 2.0 (1.1) medications. Unmedicated mean (SD) DIOP was 22.8 mmHg (2.5) preoperatively and 14.9 (3.6) at 12 months, (−7.9 mmHg, −35%, P<0.001). Most (38/39, 97%) had an IOP reduction, and 85% had ≥20% reduction (Figure 1). Medications were reduced to 0.15 (0.43, - 93%, P<0.001). The majority (87%) of patients required no medications (Figure 2). Mean IOP and medication use for all follow-up visits are shown in Figure 3. There were no SSI. Adverse events were mild, self-limiting and typical of MIGS combined with cataract surgery; IOP increase ≥ 10 mmHg at ≥ 1 month (2, 5.1%), mild inflammation (3, 7.6%), and hyphema ≥ 1 mm (1, 2.6%).
 |
Figure 2 Ocular hypotensive medication usage before preoperative and month 12 washout. |
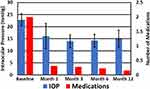 |
Figure 3 Mean intraocular pressure and medication usage by visit. N = 39, error bars are ± 1 standard deviation. |
Discussion
OMNI surgery reduced IOP and medication burden when combined with cataract surgery in a Hispanic population with OAG. The magnitude of these reductions closely mirrors those for the GEMINI study where IOP was reduced 8.2 mmHg (−35%) and medication use by 1.4 (−80%).5 While the current study suggests generalizability of the multicenter GEMINI results, congruence of the effectiveness results was not necessarily a given. Okeke found that outcomes with Trabectome were somewhat better for Hispanic than for non-Hispanic White, African-American, or Asian patients.6 Gallardo et al reported medicated IOP reductions of 5.7 to 6.5 mmHg and medication reductions of 0.6 to 1.4 for the first generation iStent in Hispanic patients with baseline medicated IOP ~19 mmHg.7 Interestingly, these data are slightly better than for those reported for a similar study based in South Dakota where medicated IOP went from 19.1 to 15.6 mmHg and medications went from 1.2 to 0.6 at 12 months.8
The Hispanic population is the second fastest growing ethnicity/race demographic in the US and the second largest.1 The Hispanic population has been underserved medically as evidenced by the large estimated proportion of undiagnosed glaucoma.3 The prevalence of OAG in Hispanics is greater than for non-Hispanic Whites.3 The size and potentially unique characteristics of this population4 underscore the importance of differentiated interventions and focused studies of effectiveness and safety in this ethnic group.
This was a single-center, single surgeon data set. Data from other centers and confirming studies are needed. Longer term data to establish effect durability would be desirable. However, within the 12 months of follow-up, no SSI were required and medication reintroduction was limited to 5 of 39 patients. This suggests that the therapeutic effect was not diminishing.
The present study was a case series of patients undergoing the OMNI procedure in conjunction with cataract surgery. It is therefore not possible with the current data set to know the relative contributions of the OMNI procedure and of cataract surgery to the observed IOP lowering. However, a recent systematic review and meta-analysis of 32 studies including 1826 patients found that cataract surgery alone could provide a 14% reduction in IOP at 12 months post-surgery in contrast to the 35% reduction observed in the present study.9
The OMNI device is a safe, implant-free MIGS combining trabeculotomy and canaloplasty. The present analysis indicates that the favorable safety and effectiveness for OMNI reported in the broader population5 is also observed in Hispanic patients.
Data Sharing Statement
The authors do not intend to share participant level data. Other queries or requests should be directed to the corresponding author (JED Jr).
Disclosure
MJG is a consultant, speaker, and clinical investigator for Sight Sciences and Nova Eye. KD and JED Jr are employees of Sight Sciences, Inc. The authors report no other conflicts of interest in this work.
References
1. Luis Noe-Bustamante MHL, Krogstad JM. US Hispanic population surpassed 60 million in 2019, but growth has slowed. Pew Research Center [Internet]; 2020 [October 12, 2021]. Available from: https://www.pewresearch.org/fact-tank/2020/07/07/u-s-hispanic-population-surpassed-60-million-in-2019-but-growth-has-slowed/.
2. Vajaranant TS, Wu S, Torres M, Varma R. The changing face of primary open-angle glaucoma in the United States: demographic and geographic changes from 2011 to 2050. Am J Ophthalmol. 2012;154(2):303–14.e3. doi:10.1016/j.ajo.2012.02.024
3. Varma R, Ying-Lai M, Francis BA, et al. Prevalence of open-angle glaucoma and ocular hypertension in Latinos: the Los Angeles Latino Eye Study. Ophthalmology. 2004;111(8):1439–1448. doi:10.1016/j.ophtha.2004.01.025
4. Wurster P, Harris A, Gonzalez AC, et al. Risk factors for open-angle glaucoma in persons of Latin American descent. J Glaucoma. 2020;29(3):217–225. doi:10.1097/IJG.0000000000001429
5. Gallardo MJ, Sarkisian SR
6. Okeke CO, Miller-Ellis E, Rojas M. Trabectome success factors. Medicine. 2017;96(24):e7061. doi:10.1097/MD.0000000000007061
7. Gallardo MJ, Supnet RA, Giamporcaro JE, Hornbeak DM. Outcomes of combined trabecular micro-bypass and phacoemulsification in a predominantly Hispanic patient population. Clin Ophthalmol. 2016;10:1931–1937. doi:10.2147/OPTH.S117403
8. Ferguson TJ, Berdahl JP, Schweitzer JA, Sudhagoni RG. Clinical evaluation of a trabecular microbypass stent with phacoemulsification in patients with open-angle glaucoma and cataract. Clin Ophthalmol. 2016;10:1767–1773. doi:10.2147/OPTH.S114306
9. Armstrong JJ, Wasiuta T, Kiatos E, Malvankar-Mehta M, Hutnik CML. The effects of phacoemulsification on intraocular pressure and topical medication use in patients with glaucoma: a systematic review and meta-analysis of 3-year data. J Glaucoma. 2017;26:511–522. doi:10.1097/IJG.0000000000000643
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

