Back to Journals » Clinical Interventions in Aging » Volume 18
C-Reactive Protein and Albumin Levels as Useful Tools for Predicting In-Hospital Outcomes in Polish Nonagenarians
Authors Mazurkiewicz M , Lizurej W, Mazurkiewicz L , Majewski A, Tobis S , Cymerys M
Received 14 June 2023
Accepted for publication 18 August 2023
Published 14 September 2023 Volume 2023:18 Pages 1547—1554
DOI https://doi.org/10.2147/CIA.S422895
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Nandu Goswami
Michal Mazurkiewicz,1,* Wojciech Lizurej,1,* Lukasz Mazurkiewicz,1,* Arkadiusz Majewski,2 Slawomir Tobis,3 Maciej Cymerys1
1Department of Internal Medicine, Poznan University of Medical Sciences, Poznan, Poland; 2Department of Computer Science and Statistics, Poznan University of Medical Sciences, Poznan, Poland; 3Department of Occupational Therapy, Poznan University of Medical Sciences, Poznan, Poland
*These authors contributed equally to this work
Correspondence: Slawomir Tobis, Department of Occupational Therapy, Poznan University of Medical Sciences, Poznan, Poland, Tel +48 61 8546573, Email [email protected]
Purpose: The admissions of nonagenarians to internal medicine wards are rising. The aim of this study was to analyse the causes of ward admission and blood and renal parameters as potential mortality predictors in this age group.
Patients and Methods: Out of 1140 patients, 111 nonagenarians aged 90+ admitted to the Internal Medicine Ward in one general hospital in Poznan in 2019 were studied. Medical records of these patients were analysed to find factors attributable to the hospitalisation.
Results: The leading causes of admission were infections and cardiovascular diseases, and the main causes of death were cardiovascular diseases. Elevated C-reactive protein (CRP) level was a statistically significant death predictor. Equally, decreased albumin level was found to be a mortality predictor. No such relationships were obtained for haematological or renal parameters.
Conclusion: Our study uniquely analysed a relatively large group of hospitalised nonagenarians and identified those who need particular attention in the ward by identifying those with the highest risk of death. CRP and albumin levels may serve as useful indicators of in-hospital mortality in this age group.
Keywords: nonagenarians, CRP, albumin level, mortality predictor
Introduction
During the 20th century, in Western Europe, the US, Canada, New Zealand, and Australia, average life expectancy increased by 30 years. Data obtained from more than 30 developed countries revealed that the chance of surviving from 80 to 90 years of age increased from 15–16% in 1950 to 37% in 2002 for women and from 12% in 1950 to 25% in 2002 for men.1 According to United Nations estimations, in 2050, there will be more than 400 million people over the age of 80 years in the world.2 Every third person in Europe will be over 60. As for patients admitted to internal medicine departments, Barba et al noticed that around 6% of them were at the age of 90 years or over and that the proportion of the oldest old was increasing rapidly.3 Nonagenarians are also the fastest-growing group in the population worldwide.4 It is estimated that the group of patients above 90 will constitute as many as 27% of all admissions to internal medicine departments in 2050.3 Many of the health systems will be challenged by insufficient availability of geriatricians.5 Since older patients are often frail and suffer from comorbidities, they may require rehabilitation services, which are aimed at restoring or maintaining their functional independence and should be tailored to their medical conditions.6 Furthermore, polypharmacy, which may lead to adverse drug effects, is much more prevalent in older patients. Therefore, the safety and appropriate use of pharmacotherapy are very important in this group of patients7 and proper use of tools from Comprehensive Geriatric Assessment is essential for the treatment of 90+ patients. Furthermore, since internal medicine wards are increasingly becoming a stop on the way to geriatric wards,8 cooperation between internists and geriatricians is of great importance,9 potentially leading to lower morbidity. Moreover, population ageing is a challenge for care systems’ budgets, as Polder et al observed that expenses for patients in the last year of life were 13.5 times higher than those of patients who did not die in the same year.10
Health-related evidence for the oldest old (90+) is scarce in the literature, particularly so when it comes to predicting survival and mortality. Our goal was thus to identify easily obtainable markers which could serve as predictors of adverse outcomes.
Patients and Methods
Study Participants
We analysed medical records of patients hospitalised in 2019 at the Internal Medicine Ward of Heliodor Swiecicki Clinical Hospital in Poznan. From the total group of 1140 patients, we selected those aged 90 years or more (n=111; 9.74%). Blood pressure and biochemical parameters were analysed at admission. Three kinds of calculations were performed: a general one, divided by gender (women/men), and according to the mortality status during hospitalisation. The group characteristics are presented in Table 1.
 |
Table 1 Mean Values of Analysed Parameters |
The study was approved by the Bioethics Committee of Poznan University of Medical Sciences, protocol number KB-877/22. The analysed data were collected retrospectively, based on patients’ medical history.
Statistical Analysis
Statistical analysis was done with Statistica 13.1 (Tibco Software, Poland). The Shapiro–Wilk test was used to check if the studied variables had a normal distribution. Student’s t-distribution was used to compare the variables which did have a normal distribution, variances were equal, and groups were not related (uric acid, haemoglobin and RBC in sex-related groups, and uric acid and RBC in groups according to mortality status). The Fisher-Snedecor test was used to check the variances in comparison with every variable with normal distribution. The Cochrane-Cox test was used when variances were not equal (sodium at admission and MCV in sex-related groups). The Mann–Whitney U-test was used when at least one of the variables did not have normal distribution and variables were not correlated. Pearson’s correlation coefficient was used for variables with normal distribution to analyse the correlation between particular parameters. Otherwise, we used Spearman’s rank correlation coefficient. If parameters were measured on a nominal scale, the C Pearson’s coefficient was used. The Chi-squared test was used to check if there was a significant relationship between death and sex, rehospitalisation, transfer from another hospital and the presence of bedsores.
p<0.05 was considered statistically significant.
Results
The most common reasons for hospitalisation in our study were: infections (38.2% - mainly pneumonia with various aetiology), cardiovascular diseases (30.0% - especially: congestive heart failure, atrial fibrillation), genitourinary system diseases (10.0% - renal failures). Less often, admissions were due to haematological and autoimmune diseases; only one patient was hospitalised due to cancer (1.0%).
The main reasons for admitting females to the ward were infections (36.8%), cardiovascular diseases (26.0%), blood and autoimmune diseases (13.0%), and genitourinary system diseases (10.9%). The most common reasons for hospitalisation of males were infections (41.1%); a similar frequency was observed for cardiovascular diseases (38.0%).
Out of the 120 deaths during hospitalisation in the department in 2019, twenty-eight were found in our study group, which accounted for 23.34% of nonagenarians admitted to the ward. No relationship was found between death and sex, rehospitalisation or transfer from another hospital; the only one we observed was between death and bedsores – they increased the risk of death (p<0.001). The leading direct causes of death in our group of nonagenarians were cardiovascular diseases (82%), particularly heart failure and atherosclerosis in various locations. Less frequent reasons for death were pneumonia, renal failure and digestive diseases. Cardiovascular diseases accounted for all direct causes of death in the men’s group. In the group of women, cardiovascular conditions accounted for 77% of all deaths. Furthermore, the ratio of deaths per admission did not differ significantly between genders (p=0.05): for men, 10 deaths per 34 admissions, and for women, 18 deaths per 77 admissions were observed.
The average systolic blood pressure was 121.89±20.29 mmHg. There were no significant differences in average systolic blood pressure in groups of survivors and non-survivors. The mean diastolic blood pressure was 71.27±12.36 mmHg. There were no significant differences in average diastolic blood pressure in the studied subgroups. We observed a moderate positive correlation between systolic and diastolic blood pressure (p<0.001; R=0.37) and a weak correlation between systolic blood pressure and the level of potassium at admission (p<0.05; R=0.25). Also, weak correlations between diastolic blood pressure and the level of haemoglobin (p<0.05; R=0.25), RBC (p<0.05; R=0.27) and PLT (p<0.05; R=0.26) were found. The average sodium level was 136.73±7.00 mmol/L. No significant differences between the level of sodium in the group of survivors and non-survivors were observed. There were moderate correlations between sodium and urea (p<0.001; R=0.33) and sodium and creatinine (p<0.001; R=0.31). The mean level of potassium during the stay was 4.51±0.92 mmol/L. No significant differences in potassium levels were measured between the studied subgroups. The potassium level correlated moderately with the urea level (p<0.001; R=0.36).
Several blood parameters were examined in our study. The global mean haemoglobin (Hb) level was 11.35±2.6 g/dl. The mean Hb level tended to be lower in the group of patients who died during hospitalisation. Table 2 presents the laboratory findings.
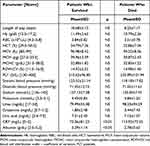 |
Table 2 Laboratory Findings |
The mean value of CRP was 81.31±80.89 mg/l. Patients who died had statistically higher CRP values than those who survived. As for the renal parameters, urea level was increased in all studied subgroups (global average at 83.70±64.75 mg/dL); there were no significant differences in mean values of urea in the subgroups. The correlation between creatinine and the uric acid level was strong (p<0.001; R=0.59). No significant differences were observed for average uric acid levels in survivors and non-survivors (global mean at 7.20±2.29 mg/dL). Total protein level correlated moderately with albumin level (p<0.001; R=0.66) and weakly with red blood cell distribution width – coefficient of variation (RDW-CV, p<0.05; R=0.25). The mean albumin level was 3.19±1.08 g/dL. There were significant differences between the groups of men and women (3.32±0.49 g/dL vs 3.13±1.25 g/dL, p<0.05) and also between survivors and non-survivors (3.29±1.14 g/dL vs 2.78±0.65 g/dL, p<0.05). Albumin levels were moderately correlated with CRP (p<0.001; R=0.39) and weakly with haemoglobin (p<0.05; R=0.24). Low albumin levels can be considered a predictor of mortality: patients with lower albumin levels were more likely to decrease.
No other statistically significant differences were observed between men and women in haematological and biochemical parameters.
Discussion
Nonagenarians represent a large and understudied group of patients admitted to hospitals. Studies on the relationships between biochemical markers and mortality in nonagenarians are extremely sparse in the literature. We analysed values of easily obtainable markers (among them, albumin and CRP levels) as potential predictors of in-hospital mortality. We were able to identify three papers that analysed these factors in groups aged 90 years and more.11–13
Our studied group accounted for 9.74% of total admissions to the ward, visibly more than in internal medicine wards in Spain between the years 2005 and 2007, where admissions of patients older than 90 years of age constituted 5.80%.3 The mean age of nonagenarians at admission was comparable across different countries: Israel 93.1±2.9, Spain 93.3±2.9, Poland 92.8±2.3.8,14
Studies involving patients aged 90 years or more revealed that women were more often hospitalised than men, similar to our study.14,15 Proportions of women and men admitted to the wards were comparable in many healthcare institutions, but proportions between nonagenarians and younger patients differed.3
The mean length of hospital stay was comparable in various studies, at around 9–11 days: 9.6±9.2,3 10.6±7.2;14 our result was similar with 10.1±5.8 days. The length of hospitalisation is known to be influenced by such factors as malnutrition, cognitive impairment and infectious diseases. Also, frailty syndrome has been found to be strongly associated with in-hospital mortality and length of stay.16 Furthermore, loss of functional capacity at discharge was assessed by many researchers as the most significant cause of mortality in 90+ patients.15 A study conducted by Chao et al involving hospitalised older patients (76–103 years of age) revealed that the occurrence of cognitive impairment, particularly dementia, among these patients was generally high and was associated with both longer stay and readmission within 30 days. Moreover, patients with cognitive impairment had more geriatric syndromes: frailty, gait disturbance and falls, incontinence, delirium and malnutrition.17
In the literature, both the reasons for admission to the hospital and the methods of categorising diagnoses by a medical unit are widely considered to have an effect on the results.18 In our study, the largest group constituted infections such as pneumonia, urinary tract inflammation, or sepsis; the second largest one was cardiovascular diseases (as presented in Figure 1). In the abovementioned Spanish study, pneumonia and urinary tract infections were the most common (27.9%), followed by heart failure (23.3%), chronic obstructive pulmonary disease (13.1%) and strokes (10.8%).14 In our sample, only one patient was hospitalised due to a transient ischemic attack (in Poland, particularly in cities, stroke patients are admitted directly to neurological stroke units). Another internal department in Spain reported acute respiratory failure (35.7%) and congestive heart failure (14.8%) as the most common.3 In an Israeli study, the leading diagnoses were acute infections (57%), in which urinary tract diseases were the most common and constituted 31% of total admissions. Acute coronary syndromes were less frequent and accounted for 17% of hospitalisations. Additionally, renal failure and permanent urinary catheters were demonstrated to predict post-discharge mortality.8 Hospitalisations due to cancer are rare in the group of nonagenarians - probably due to the fact that cancer patients have, on average, shorter life expectancy. In our study, only one patient was admitted due to cancer.
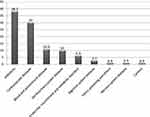 |
Figure 1 The main reasons for admission to hospital among 90+ patients. |
Over the course of the year, 28 nonagenarians died during their stay at the unit, resulting in a mortality rate of 25.2%. In other studies, the in-hospital mortality of nonagenarians reached 21.8%3 and 22.0%.8 In a Spanish study involving an acute geriatric unit, 13.3% of nonagenarians died during hospitalisation.15 Based on our data, the main reasons for death in the group of 90+ patients were cardiovascular diseases (82%), particularly heart failure. The remaining causes of death were related to incapacity of the digestive, genitourinary and respiratory systems. In 42.8% of analysed cases, the direct cause of death was the same as the diagnosis on admission.
According to Statistics Poland (GUS), in 2019, Polish people died the most often due to cardiovascular conditions (39.4%) and neoplasms (26.5%).19 The highest number of deaths in 2019 was recorded in the group of citizens over 85 years of age. In 2019, 53% of them died due to cardiovascular disorders. The second dominant group were reasons described as “symptoms, signs and abnormal clinical and laboratory findings, not elsewhere classified” according to ICD-10, which constituted the reason for 17% of deaths in this group. Cancer was the cause of death of 12% of people over 85 years of age.
As for CRP, there are differing opinions on the usefulness of this parameter in older adults.20,21 Our patients were hospitalised due to severe conditions, like respiratory tract infections. CRP is a protein commonly used not only to diagnose infections but also to predict outcomes and evaluate treatment options.20 This makes the CRP a crucial inflammatory marker. Karasahin et al described the monitoring of changes in CRP level as a prognostic tool in older patients, in contrast to the initial CRP level, which does not have a prognostic value when considering infectious diseases.20 Serino et al evaluated patients with a mean age of 66 years and found that elevated CRP level was the only independent risk factor for in-hospital mortality in influenza patients.22 On the contrary, a study on nonagenarians revealed no statistical significance of CRP level as a mortality predictor, recommending the use of Interleukin-1 receptor antagonist instead.13 The results of a recent study carried out on patients aged 65 and above suggest using more sophisticated parameters – neutrophil to lymphocyte ratio and C-reactive protein/albumin ratio, which are considered a better choice in predicting in-hospital mortality in older subjects.23 Nevertheless, in our study, CRP was a statistically significant mortality predictor: elevated CRP values were associated with fatal in-hospital outcomes. This also suggests the need for periodical CRP measurements in the treatment of nonagenarians.
The level of albumin, as a negative serum phase protein, descends during sepsis or other inflammations. Ranzani et al noticed that albumin level could be a hospital survival predictor. Hypoalbuminemia can also be associated with malnutrition.24 Brown et al investigated patients aged ≥ 75 years admitted to an acute-care geriatric ward and observed that not only hypoalbuminemia but also other biochemical markers such as low total cholesterol level, hyperglycaemia, high C-reactive protein level and renal impairment markers predicted the in-hospital mortality.25 Aronen et al also stressed that albumin level on admission appeared to be a predictor of potential patient recovery in treating respiratory infections in older adults.26 Dagmura et al studied octogenarians and nonagenarians undergoing colorectal cancer surgery and also identified albumin level as a prognostic marker for survival.11 Similarly, Huang et al observed that serum albumin predicted mortality in a group of nonagenarians with acute infections.12 Based on our results, high C-reactive protein levels can serve as a predictor of in-hospital mortality in the general population of nonagenarians; we also observed a reverse proportionality between albumin level and mortality during hospitalisation. Patients with lower albumin levels were more likely to decrease during hospitalisation. Apart from that, hypoalbuminemia may result from inflammation, which, in turn, may have serious consequences.
The prevalence of chronic kidney diseases increases with age. According to Hamrahian et al, hypertension can be both a reason and an effect of chronic kidney disease.27 We observed no correlation between blood pressure and the parameters of renal function. As our results showed, urea level was increased in both groups, which is in agreement with the results obtained by Musch et al, stating that urea level is directly proportional with age28 - according to this study, there was no correlation between creatinine level and age. Despite that, creatinine level was raised in our nonagenarians.
Our study has some limitations. The impact of medications on the patients’ clinical state and therapy was not analysed, nor was their previous health status. No assessment of functional independence was conducted among the patients during admissions and hospitalisation. Still, our paper confirms the significance of the oldest old for the health care system and identifies challenges for health services. The group of nonagenarians is rarely studied in the literature despite its dynamically growing clinical importance. The high number of included subjects enabled a credible analysis of factors that are characteristic of the hospitalisation of patients aged 90+.
Future Directions
The relation between parameters and causes of admission may be an interesting path for future research to ascertain that changes are not related to specific causes. Furthermore, the relevant results may benefit from a dedicated risk study.
Conclusion
The main reasons for hospitalisations in our study sample were infections and cardiovascular diseases. The majority of patients died for reasons other than those for which they were admitted. Cancer incidence was observed rarely. The group of the oldest old requires particular attention during hospitalisation, among others, by identifying those with the highest risk of death. CRP and albumin levels may be useful as indicators of in-hospital mortality, which was, for the first time, demonstrated for the general population of nonagenarians.
Abbreviations
BMI, Body Mass Index; Hb, haemoglobin; RBC, red blood cells; HCT, haematocrit; MCV, mean corpuscular volume; MCH, mean corpuscular haemoglobin; MCHC, mean corpuscular haemoglobin concentration; RDW-CW, red blood cell distribution width, coefficient of variation; PLT, platelets; CRP, C reactive protein.
Data Sharing Statement
The data was collected retrospectively based on patients’ medical history. The datasets used during the current study are available from the corresponding author on reasonable request.
Ethics Approval
The study was approved by the Bioethics Committee of Poznan University of Medical Sciences, 70 Bukowska Street, 60-812 Poznan.
Consent for Publication
Since it was based on an analysis of existing medical records and did not constitute a medical experiment, considering the retrospective nature of the study informed consent was waived by the Bioethics Committee of Poznan University of Medical Sciences (protocol number KB-877/22). Our research was performed in accordance with the Declaration of Helsinki.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
There is no funding to report.
Disclosure
The authors declare no conflicts of interest.
References
1. Christensen K, Doblhammer G, Rau R, Vaupel JW. Ageing populations: the challenges ahead. Lancet Lond Engl. 2009;374:1196–1208. doi:10.1016/S0140-6736(09)61460-4
2. World Population Prospects. Population Division - United Nations. Available from: https://population.un.org/wpp/Graphs/Probabilistic/POP/80plus/900.
3. Barba R, Martínez JM, Zapatero A, et al. Mortality and complications in very old patients (90+) admitted to departments of internal medicine in Spain. Eur J Intern Med. 2011;22:49–52. doi:10.1016/j.ejim.2010.11.001
4. Kawas CH. The oldest old and the 90+ Study. Alzheimers Dement J Alzheimers Assoc. 2008;4:S56–59.
5. Borrie M, Cooper T, Basu M, Kay K, Prorok JC, Seitz D. Ontario geriatric specialist physician resources 2018. Can Geriatr J CGJ. 2020;23:219–227. doi:10.5770/cgj.23.448
6. Weber DC, Fleming KC, Evans JM. Rehabilitation of geriatric patients. Mayo Clin Proc. 1995;70:1198–1204. doi:10.4065/70.12.1198
7. Delgado-Silveira E, Bermejo-Vicedo T. The role of pharmacists in geriatric teams: the time is now. Eur Geriatr Med. 2021;12:1119–1121. doi:10.1007/s41999-021-00501-8
8. Zafrir B, Laor A, Bitterman H. Nonagenarians in internal medicine: characteristics, outcomes and predictors for in-hospital and post-discharge mortality. Israel Med Assoc J. 2010;12(1):10–15.
9. Mannucci PM, Nobili A. Internal and geriatric medicine: an alliance for the challenges of the elderly. Eur J Intern Med. 2012;23:479–482. doi:10.1016/j.ejim.2012.06.008
10. Polder JJ, Barendregt JJ, van Oers H. Health care costs in the last year of life--the Dutch experience. Soc Sci Med. 2006;63:1720–1731.
11. Dagmura H, Daldal E, Okan I. The efficacy of hemoglobin, albumin, lymphocytes, and platelets as a prognostic marker for survival in octogenarians and nonagenarians undergoing colorectal cancer surgery. Cancer Biother Radiopharm. 2022;37:955–962. doi:10.1089/cbr.2020.4725
12. Huang W, Sun Y, Xing Y, Wang C. Functional impairment and serum albumin predict in-hospital mortality in nonagenarians with acute infection: a retrospective cohort study. BMC Geriatr. 2019;19:269. doi:10.1186/s12877-019-1301-1
13. Jylhä M, Paavilainen P, Lehtimäki T, et al. Interleukin-1 receptor antagonist, interleukin-6, and C-reactive protein as predictors of mortality in nonagenarians: the vitality 90+ study. J Gerontol a Biol Sci Med Sci. 2007;62:1016–1021. doi:10.1093/gerona/62.9.1016
14. Socorro García A, de la Puente M, Perdomo B, López Pardo P, Baztán JJ. Functional status and mortality at month and year in nonagenarians hospitalized due to acute medical illness. Eur J Intern Med. 2015;26:705–708. doi:10.1016/j.ejim.2015.08.007
15. Formiga F, Ferrer A, Mascaró J, Ruiz D, Olmedo C, Pujol R. Predictive items of one-year mortality in nonagenarians. The NonaSantfeliu Study. Aging Clin Exp Res. 2007;19:265–268. doi:10.1007/BF03324700
16. Chong E, Ho E, Baldevarona-Llego J, et al. Frailty in hospitalized older adults: comparing different frailty measures in predicting short- and long-term patient outcomes. J Am Med Dir Assoc. 2018;19:450–457.e3. doi:10.1016/j.jamda.2017.10.006
17. Chao Y-T, Kuo F-H, Lee Y-S, et al. Characteristics and outcome determinants of hospitalized older patients with cognitive dysfunction. Int J Environ Res Public Health. 2022;19:584. doi:10.3390/ijerph19010584
18. Ramos JM, Sánchez-Martínez R, Nieto F, et al. Characteristics and outcome in nonagenarians admitted in general internal medicine and other specialties. Eur J Intern Med. 2013;24:740–744. doi:10.1016/j.ejim.2013.07.003
19. Statistics Poland. Rocznik Demograficzny 2021. stat.gov.pl. Available from: https://stat.gov.pl/obszary-tematyczne/roczniki-statystyczne/roczniki-statystyczne/rocznik-demograficzny-2021,3,15.html.
20. Karasahin O, Tasar PT, Timur O, Yıldırım F, Binici DN, Sahin S. The value of C-reactive protein in infection diagnosis and prognosis in elderly patients. Aging Clin Exp Res. 2018;30:555–562. doi:10.1007/s40520-017-0821-9
21. Ticinesi A, Lauretani F, Nouvenne A, et al. C-reactive protein (CRP) measurement in geriatric patients hospitalized for acute infection. Eur J Intern Med. 2017;37:7–12. doi:10.1016/j.ejim.2016.08.026
22. Serino M, Melo N, Caldas JP, Ferreira A, Garcia D, Lourenço P. Predictors of severity and in-hospital mortality in patients with influenza. Monaldi Arch Chest Dis Arch Monaldi Mal Torace. 2021;92. doi:10.4081/monaldi.2021.1876
23. Ayrancı MK, Küçükceran K, Dundar ZD. NLR and CRP to albumin ratio as a predictor of in-hospital mortality in the geriatric ED patients. Am J Emerg Med. 2021;44:50–55. doi:10.1016/j.ajem.2021.01.053
24. Ranzani OT, Zampieri FG, Forte DN, Azevedo LCP, Park M. C-reactive protein/albumin ratio predicts 90-day mortality of septic patients. PLoS One. 2013;8:e59321. doi:10.1371/journal.pone.0059321
25. Brown SH, Flint K, Storey A, Abdelhafiz AH. Routinely assessed biochemical markers tested on admission as predictors of adverse outcomes in hospitalized elderly patients. Hosp Pract. 2012;40:193–201. doi:10.3810/hp.2012.02.960
26. Aronen M, Viikari L, Langen H, et al. The long-term prognostic value of serum 25(OH)D, albumin, and LL-37 levels in acute respiratory diseases among older adults. BMC Geriatr. 2022;22:146. doi:10.1186/s12877-022-02836-8
27. Hamrahian SM, Falkner B. Hypertension in Chronic Kidney Disease. Adv Exp Med Biol. 2017;956:307–325.
28. Musch W, Verfaillie L, Decaux G. Age-related increase in plasma urea level and decrease in fractional urea excretion: clinical application in the syndrome of inappropriate secretion of antidiuretic hormone. Clin J Am Soc Nephrol. 2006;1:909–914. doi:10.2215/CJN.00320106
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
