Back to Journals » ClinicoEconomics and Outcomes Research » Volume 14
Burden and Cost of Anterior Cruciate Ligament Reconstruction and Reimbursement of Its Treatment in a Developing Country: An Observational Study in Indonesia
Authors Deviandri R , van der Veen HC, Lubis AMT, Utoyo GA, van den Akker-Scheek I, Postma MJ
Received 5 April 2022
Accepted for publication 11 July 2022
Published 17 July 2022 Volume 2022:14 Pages 479—486
DOI https://doi.org/10.2147/CEOR.S368840
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Xing Lin Feng
Romy Deviandri,1– 3 Hugo C van der Veen,1 Andri MT Lubis,4 Ghuna A Utoyo,5 Inge van den Akker-Scheek,1 Maarten J Postma6– 9
1Department of Orthopedic Surgery, University of Groningen/ University Medical Center Groningen, Groningen, the Netherlands; 2Department of Physiology-Faculty of Medicine, Universitas Riau, Pekanbaru, Indonesia; 3Department of Orthopedics-Sports Injury, Arifin Achmad Hospital, Pekanbaru, Indonesia; 4Department of Orthopedics-Faculty of Medicine, Universitas Indonesia/Cipto Mangunkusumo Hospital, Jakarta, Indonesia; 5Department of Orthopedics-Faculty of Medicine, Universitas Padjadjaran/ Hasan Sadikin Hospital, Bandung, Indonesia; 6Department of Health Sciences, University of Groningen/ University Medical Center Groningen, Groningen, the Netherlands; 7Department of Economics-Faculty of Economics & Business, University of Groningen, Groningen, the Netherlands; 8Department of Pharmacology & Therapy, Universitas Airlangga, Surabaya, Indonesia; 9Department Center of Excellence in Higher Education for Pharmaceutical Care Innovation, Universitas Padjadjaran, Bandung, Indonesia
Correspondence: Romy Deviandri, Department of Orthopedic Surgery, University of Groningen/ University Medical Center Groningen, Hanzeplein 1, Groningen, 9713 GZ, the Netherlands, Email [email protected]; [email protected]
Objective: The number of anterior cruciate ligament reconstruction (ACLR) procedures is increasing. However, ACLR procedures are likely to be underbudgeted in a developing country like Indonesia. This study aimed to analyze costs for ACLR procedures in Indonesia’s resource-limited context, determine the burden of ACLR, and suggest national prices for ACLR reimbursement.
Methods: A retrospective observational study was conducted between 1 January and 31 December 2019 on the cost of ACLR from a payer perspective using inpatient billing records in four hospitals. The national burden of ACLR was calculated, and projected national prices for reimbursement were determined.
Results: Of 80 ACLRs, 53 (66%) were isolated ACLRs and 27 (34%) ACLRs were combined with meniscus treatment. Mean hospital costs incurred per ACLR procedure were US$ 2853, with the dominant cost relating to orthopedic implant prices (US$ 1,387.80). The costs of ACLR with combined meniscus treatment were estimated as being 35% higher than isolated ACLR. The national burden of ACLR showed a total budget of US$ 367.4 million per 100,000 patients (0.03% of GDP) for ACLR with additional meniscus treatment and US$ 271.3 million per 100,000 patients (0.02% of GDP) for isolated ACLR.
Conclusion: ACLR procedures in Indonesia are likely underbudgeted. Adjustments of reimbursement prices for ACLR are needed to facilitate adequate access of Indonesians to the procedures. This study demonstrated varying costs determined for ACLR in Indonesia, which entails that a new reimbursement system with improvement of national prices should become the core of transformation.
Keywords: ACL tear, meniscus injury, cost, developing countries, BPJS
Introduction
Anterior cruciate ligament (ACL) rupture is a common sports injury. The estimated overall age- and sex-adjusted annual incidence of ACL rupture is between 0.03% and 0.04%.1 Anterior cruciate ligament reconstruction (ACLR) surgery is an operation frequently performed by orthopedic surgeons worldwide. An estimated 400,000–500,000 ACLR procedures are performed each year in the United States based on implant usage.2 These numbers have also risen in developing countries, including Indonesia. ACLR implant usage in Indonesia increased by 42% in 2019 compared to 2018 (1575 implants in 2018 vs 2236 in 2019), and are expected to climb further as a result of increased participation in sports activities by adolescents and young adults.3 Although exact data is lacking about the annual incidence of ACL rupture in Indonesia, it is estimated that the number reaches almost one million people per year entire Indonesian population of 270 million people.1,4
In conjunction with the rising prevalence of ACLR, the cost of this procedure is also on the rise. In the United States, where US$ 1 billion is spent on ACLR procedures each year,5 the mean direct price of an ACLR increased from $7634 in 2005 to $10,780 in 2013, and this cost is expected to keep rising gradually.6 ACLR costs are influenced by many aspects, such as use of general anesthesia; time spent in the operating room; patient factors including older age, male sex, ethnicity, and number of chronic medical conditions; insurance type; and annual income.6 There are significant differences in costs between ACLRs with and without concomitant meniscal treatment (repair or meniscectomy).5,7
There is a lack of data on the burden of the cost of ACLR procedures in developing countries. In 2014 Indonesia – the most populous country in Southeast Asia and the fourth globally – introduced a new national health insurance system administered by the healthcare and social security agency BPJS Kesehatan (BPJS-K).8 In 2018, universal health coverage (UHC) provided by BPJS-K was introduced for 203 million people.9 In 2019–2020 coverage was extended to the entire Indonesian population (270 million).4,10 Accordingly, a national reimbursement price for each disease and procedure will need to be accounted for within the reimbursement system.9,10
The Indonesian Ministry of Health has implemented a standard rate for ACLR procedures in the IDR 9,586,400 to 31,379,700 range (US$ 677 to 2215, exchange index year 2019), depending on region, room class, and type of hospital.11 These prices do not take into account any concomitant procedures like meniscal surgery. This rate seems like a very low estimate of the costs compared with the data from the US. While understanding the difficulty of comparing budgeting rates between a developed country and Indonesia, there might still be a need to adjust this budgeting cost more rationally depending on the actual situation. The international budgetary guidelines for particular practices apply mainly to developed countries and therefore may require cost adjustments of service bundles relating to ACLR procedures in resource-limited settings.12
The possibility of underbudgeted ACLR procedures in Indonesia is presumed, therefore a re-evaluation of these costs has become urgent. This study analyzed costs for ACLRs in natural settings for each region of Indonesia. In the same manner, it determined rational national prices for reimbursement under UHC, based on the calculated burden and costs of an ACLR.
Methods
Study Design
The study was approved by the Institutional Review Board (KET- 894/UN2.F1/ETIK/PPM.00.02/2020) of the Faculty of Medicine of Universitas Indonesia- Cipto Mangunkusumo Hospital in Jakarta, Indonesia, and patient consent to review their medical records was not required because of a database study. Subsequently, for covering patient data confidentiality, all of data were kept anonymized. This study has been performed in accordance with the principles stated in the Declaration of Helsinki. A retrospective database study was conducted on medical records of patients with an ACLR in four Indonesian medical centers: (1) Dr. Cipto Mangunkusumo Hospital (RSCM) in Jakarta, a national healthcare referral center with 1181 beds; (2) Dr. Hasan Sadikin Hospital (RSHS) in Bandung, a national referral center with 928 beds; (3) Dr. M. Djamil Hospital (RSMJ) in Padang, a national referral center with 800 beds, serving western Indonesia; and (4) Arifin Achmad Hospital (RSAA) in Pekanbaru with 673 beds, serving western Indonesia.13 Inpatient registries and hospital discharge data were obtained from the Department of Medical Records from 1 January to 31 December 2019. The dataset covered patient demographics, diagnoses, additional meniscal procedures, costs of surgery, inpatient costs, laboratory tests, radiology, and medications.
Criteria for Selecting Patients
All patients with arthroscopic ACLR procedures were included. Data extraction was done from an electronic system of the hospital by code S.83.5 of Indonesian Case Base Groups (INA-CBGs). ACL revision procedures and multi-ligament reconstructions were excluded.
Cost Calculation
The costs were calculated from a payer perspective using billing records that included the costs of beds, pharmacy, implants, surgical procedures, other expenses, and total costs. Bed costs comprised hospital administration fees, daily room services, nursing, and medical staff care. Physiotherapists’ and rehabilitation specialists’ costs were calculated under patients’ bed service costs. Pharmacy prices were derived from the pharmacy department’s budget covering costs relating to drugs, fluids, disposable devices, oxygen, and pharmacy services either in the ward or in the operating room. Implant usage for both ACL reconstruction surgery and the concomitant procedure such as meniscus repair were analyzed separately. The surgical procedure included medical services fees for the reconstruction procedure and orthopedic, anesthesiological, and operating room services, plus costs for laboratory work, radiology, and other supporting investigation procedures if needed. The 2019 currency exchange rate (US$ 1 = 14,147,671 IDR) was used, as applied by the Organization for Economic Cooperation and Development (OECD), to convert Indonesian Rupiahs (IDR) into US Dollars (US$).14 The economic burden of an ACL reconstruction procedure was determined by distribution of disease incidence and mean cost of each procedure using a denominator of 100,000 patients.
Extrapolation of the Cost to the National Level
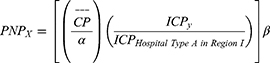
The national costs for ACLR procedures were calculated based on the rates described by the Indonesian Ministry of Health for Indonesia Case Base Groups (INA-CBGs). INA-CBGs’ rates were used as national estimation for projecting ACLR costs – accomplished from patients’ billing records – into Proposed National Prices (PNPs) for ACLR reimbursements by taking four aspects into account.11 The first aspect considered three room classes at the hospital. Class I accommodates up to two patients and has more privacy within one room; Class II accommodates three or four patients; Class III service accommodates five or six patients in a room. This study determined the PNP in Class III as the reference. It estimated the actual costs from Classes I, II, and III [Class Price (CP)] – obtained from patients’ billing records – and divided them by the specific factor (α) in accordance with the INA-CBGs at 1.0, 1.2, and 1.4, respectively. The second aspect considered the private or public sector ownership of the hospital. In the INA-CBG system, reimbursement provided by the government through subsidies was 1.03 (β) times higher for private than for public healthcare services.11 Both α and β factors were associated with the difference of CP between each room class and between the private or public sector ownership of the hospital in BPJS-K system.11 The third and fourth aspects considered the hospital’s type and region, corresponding with the particular INA-CBG prices (ICPy) published by the Indonesian Ministry of Health in 2016. Based on the medical specialist services, hospitals in Indonesia were classified into types A, B, C, and D. Five INA-CBG regions covered a total of 34 provinces, with region 1 consisting of the Banten, Jakarta, West Java, Central Java, Yogyakarta, and East Java provinces as a reflection of the center of activity in Indonesia (Figure 1).10,11 The ICP for Hospital Type A in Region 1 was used as the denominator reference for ICP in calculating a PNP since the actual costs were obtained from the hospitals with type A located in INA-CBG Region 1. For an inpatient ACL tear following ACLR, in a specific class of room, type of hospital and particular region under the private or the public sectors, a PNP was defined with the following formula:
 |
Figure 1 The five regions covered in the Indonesia Case Base Group (INA-CBG) system. Region 1 (green): Banten, Jakarta, West Java, Central Java, Yogyakarta, and East Java. Region 2 (blue): West Sumatra, Riau, South Sumatra, Lampung, Bali, and West Nusa Tenggara. Region 3 (red): Aceh Darussalam, North Sumatra, Jambi, Bengkulu, Bangka Belitung, Riau Islands, West Kalimantan, North Sulawesi, Central Sulawesi, Southeast Sulawesi, West Sulawesi, South Sulawesi, and Gorontalo. Region 4 (yellow): South Kalimantan, East Kalimantan, North Kalimantan, and Central Kalimantan. Region 5 (purple): East Nusa Tenggara, Maluku, North Maluku, Papua, and West Papua. Adapted from Khairul A, Purba R, Mariana N, Aliska G, Hadi S. The burden and costs of sepsis and reimbursement of its treatment in a developing country: An observational study on focal infections in Indonesia. Int J Infect Dis. 2020;96:211–218. © 2020 The Author(s). Published by Elsevier Ltd on behalf of International Society for Infectious Diseases. This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/).10 |
Formula 1. PNP reflecting the mean actual costs estimated from four aspects: single mean class price (CP), specific factor (α) of each class, exact INA-CBG prices (ICPy), and government subsidy factor (β).10,11
Statistical Analyses
Data were analyzed using IBM SPSS statistics version 26.0 (IBM), providing descriptive data on baseline characteristics in percentages. To determine the statistical cost difference, an independent sample t-test was performed. Statistical significance was defined as a p-value <0.05.
Results
Of the 80 patients, 68 were male (85%) and 12 female (15%). More than half of the patients had isolated ACL injuries on the right side (55%). Most of the patients were non-professional athletes with a mean age of 26.3±8.5 years (Table 1).
 |
Table 1 Demographic Patient Characteristics (N=80) |
Hospitalization Costs
The mean cost per ACLR procedure was US$ 2853. The highest cost was found in RSCM Jakarta – the capital city of Indonesia (Table 2). The dominant cost was from orthopedic implant prices (US$ 1387.80). Table 3 shows all costs divided into unit cost for beds, pharmacy, implants, surgery, and other costs.
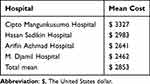 |
Table 2 Mean Cost of ACLR at Each Hospital (US$) |
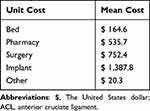 |
Table 3 Unit Cost of ACL Reconstruction Procedure in the Hospital (US$) |
The cost analyses of an ACLR procedure indicated that the cost was higher with the concomitant meniscal repair procedure than an isolated ACLR itself. There was also a significant difference in cost between ACLR with additional meniscal treatment procedure (US$ 3674) and ACLR without additional meniscal treatment procedure (US$ 2713; difference US $961, p<0.05).
National Burden of ACLR and Prospective National Prices
Analysis of the treatment costs of ACLR procedures showed that the lowest price within the INA-CBG system (ICP) was for an isolated ACLR in a type D public hospital in region I with an estimated PNP of US$ 1267. The highest PNP was for ACLR including meniscus treatment in a type A private hospital in region 5 (US$ 4011). The national burden of ACLR thus revealed a total budget of US$ 367.4 million per 100,000 patients (0.03% of Indonesian GDP) for isolated ACLR with concomitant meniscal procedure and a total budget of US$ 271.3 million per 100,000 patients (0.02% of Indonesian GDP) for isolated ACLR. The complete rates specified for the ICPs for an ACLR procedure in all five regions of Indonesia are reported in the Appendices (supplementary Data Table A.1).
Discussion
In this study, the economic burden of ACLR procedures was comprehensively determined in the resource-limited setting of Indonesia. The main finding is that ACLR procedures in Indonesia are underbudgeted. ACLR procedures are shown to have a high impact on the national burden (US$ 271.3 million to 367.4 million). In addition, this study proposes the national price for ACLRs in all regions of Indonesia. From the results we found that the mean cost of an ACLR in Indonesia was $2853 – lower than the actual costs of ACLR in others countries, such as the United States (US$24,707),5 the Netherlands (US$ 7129),15 Sweden (US$ 5760),16 Switzerland (US$ 7391),17 Malaysia (US$ 4354),18 or Thailand (US$ 5710).18 The low operating costs of ACLR in Indonesia showed it to be a competitive country in medical care for ACLR procedures.
However, the results of this study showed that the actual costs of an ACLR procedure were higher than the reimbursement level of the Indonesian national health insurance system (US$ 2853 vs 1451). There seems an underbudgeting of reimbursement prices for ACLRs, with a gap of US$ 1402. BPJS-K determined the same reimbursement prices for ALCR with additional meniscal treatment – such as meniscus repair or meniscectomy – as for isolated ACLR. This study showed a significant difference between those procedures, with a gap of US$ 961, which is in line with other studies.5,19 This discrepancy is likely caused by the use of additional meniscal repair implants, increased operating time, and accordingly additional anesthetics use.6,20,21 Determination of the substantial costs is necessary for the healthcare system to properly facilitate accessible medical care. We therefore propose a new national price for ACLR procedures and adjustment of ACLR costs with concomitant meniscal procedure. The INA-CBG prices from the Indonesian Ministry of Health published in 2016 introduced the top-up payment system for any special factor – special drugs, special procedure, special prosthesis, special investigation, sub-acute cases, and chronic cases – as additional payment to cover the fees for those procedures.11 This is known as special Casemix Main Groups (CMG) in the INA-CBG system. In the orthopedic field, this top-up payment has been applied for particular procedures as an adjustment-cost system, such as total knee replacements and total hip replacements. We propose including both the ACLR procedure and the meniscal treatment procedures in this adjustment-cost system to make these interventions more accessible.
A growing body of evidence shows that the deficit in the cost reimbursement system could create a surgical culture whereby surgical decisions are influenced by insurance reimbursement.22,23 In a reimbursement structure that does not consider the patient or surgical complexity, surgeons might be rewarded for performing cost-saving surgeries that neglect coexisting repairable meniscal pathology. There is convincing evidence of the meniscal repair procedure as a cost-effective strategy in the setting of ACLR surgery.5,19
Efforts to adjust ACLR costs – as well as the meniscal treatment cost as a concomitant injury in ACL cases – in Indonesia’s national health insurance system with reasonable prices are essential to facilitate access of Indonesians to ACLR procedures. ACLR surgery is an effective treatment for ACL injury patients, especially for those with high activity levels. A growing body of evidence shows that ACLR is a cost-effective strategy for treating ACL injury.17,24–27 It is described that delayed treatment for ACL injury patients would cause higher societal impact and higher burden of disease for the national economy.24 Plus, many studies show that meniscus repair is a more cost-effective strategy than meniscectomy or conservative treatment.6,28,29
This study has some limitations. Data from only four hospitals in Indonesia was used. More data from other hospitals in Indonesia would provide a more complete overview of the costs of an ACLR procedure. Still, these four hospitals can be considered a good representation of the hospitals from regions 1 and 2 of Indonesia in terms of the country’s national health insurance system. The ICP for the hospitals in this study can be used as the denominator reference for calculating reimbursement costs for all types of hospitals located in all regions of Indonesia’s national health insurance system. Next, we analyzed merely isolated ACL cases and concomitant meniscal injuries. We did not consider other potential additional procedures related to ACLR, such as cartilage procedures or multi-ligament reconstructions that could increase ACLR costs. Further research is needed to analyze the costs of ACLR with other possible concomitant procedures than meniscal treatment alone.
Conclusion
The reimbursement prices for an ACLR procedure are lower than the actual prices in the Indonesian national healthcare system. Hence an adjustment of reimbursement prices for ACLR procedures with or without concomitant meniscal surgery is warranted to facilitate access for Indonesians. We likewise determined reasonable costs for ACLR procedures in all regions of Indonesia and proposed that they be the same as BPJS-K’s reimbursement amounts.
Acknowledgements
We extend our gratitude to Abdul Khairul RP, MD, Hidayat, MD, and Dea Payes, MD, for facilitating this research.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or non-for-profit sectors.
Disclosure
The authors declare no conflict of interest.
References
1. Moses B, Orchard J, Orchard J. Systematic review: annual incidence of ACL injury and surgery in various populations. Res Sports Med. 2012;20(3–4):157–179. doi:10.1080/15438627.2012.680633
2. Wright RW, Bogunovic L. Revision anterior cruciate ligament reconstruction-the multicenter anterior cruciate ligament revision study. In: The Anterior Cruciate Ligament: Reconstruction and Basic Science.
3. Deviandri R, van der Veen HC, Lubis AMT, Postma MJ, van den Akker-Scheek I. Translation, cross-cultural adaptation, validity, and reliability of the Indonesian version of the IKDC subjective knee form. Orthop J Sports Med. 2021;9(9):23259671211038372. doi:10.1177/23259671211038372
4. Central Bureau of Statistics of Indonesia. Portrait of the 2020 population census towards one Indonesian population data (Potret Sensus Penduduk 2020 Menuju Satu Data Kependudukan Indonesia); 2021. Available from: https://www.bps.go.id/publication.html.
5. Lester JD, Gorbaty JD, Odum SM, Rogers ME, Fleischli JE. The cost-effectiveness of meniscal repair versus partial meniscectomy in the setting of anterior cruciate ligament reconstruction. Arthroscopy. 2018;34(9):2614–2620. doi:10.1016/j.arthro.2018.06.046
6. Bokshan SL, Mehta S, DeFroda SF, Owens BD. What are the primary cost drivers of anterior cruciate ligament reconstruction in the United States? A cost-minimization analysis of 14,713 patients. Arthroscopy. 2019;35(5):1576–1581. doi:10.1016/j.arthro.2018.12.013
7. Sayampanathan AA, Koh B, Howe T, et al. Orthopedic Surgery Epidemiology of surgically managed anterior cruciate ligament ruptures in a sports surgery practice. J Orthop Surg. 2017;25(1):1–6. DOI:10.1177/2309499016684289
8. Health Ministry of the Republic of Indonesia. A guideline for performing the national healthcare insurance system No. 28, 2014 /PMK No. 28; 26 December 2020.
9. Agustina R, Dartanto T, Sitompul R, et al. Universal health coverage in Indonesia: concept, progress, and challenges. Lancet. 2019;393(10166):75–102. doi:10.1016/S0140-6736(18)31647-7
10. Khairul A, Purba R, Mariana N, Aliska G, Hadi S. The burden and costs of sepsis and reimbursement of its treatment in a developing country: an observational study on focal infections in Indonesia. Int J Infect Dis. 2020;96:211–218. doi:10.1016/j.ijid.2020.04.075
11. The Health Ministry Republic of Indonesia. Health Ministry, Republic of Indonesia No. 64, The standard tariff for healthcare service in the implementation of universal health coverage. (Standar tarif kesehatan dalam penyelenggaraan program jaminan; 2016.
12. Wolfe PR, Moran DW. Global budgeting in the OECD countries. Health Care Financ Rev. 1993;14(3):55–76.
13. The Health Ministry Republic of Indonesia. Direktorat jenderal pelayanan kesehatan- daftar rumah sakit. Available from: http://sirs.yankes.kemkes.go.id/integrasi/.
14. Organization for Economic Cooperation and Development. Exchange rates. Available from: https://data.oecd.org/conversion/exchangerates.htm. 2016.
15. Eggerding V, Reijman M, Meuffels DE, et al. ACL reconstruction for all is not cost- effective after acute ACL rupture. Br J Sports Med. 2021:1–5. doi:10.1136/bjsports-2020-102564
16. Kiadaliri AA, Englund M, Stefan Lohmander L, Carlsson KS, Frobell RB. No economic benefit of early knee reconstruction over optional delayed reconstruction for ACL tears: registry enriched randomized controlled trial data. Br J Sports Med. 2016;50(9):558–563. doi:10.1136/bjsports-2015-095308
17. Farshad M, Gerber C, Meyer DC, et al. Reconstruction versus conservative treatment after rupture of the anterior cruciate ligament: cost-effectiveness analysis. BMC Health Serv Res. 2011;11(1):317. doi:10.1186/1472-6963-11-317
18. Orbit Lab Aarhus University. How much is acl surgery in Malaysia. Available from: https://orbitlab.au.dk/assets/nyizvo/how-much-is-acl-surgery-in-malaysia.
19. Proietti L, Ciolli G, Corona K, Cerciello S. Regarding “What are the primary cost drivers of anterior cruciate ligament reconstruction in the United States? A cost-minimization analysis of 14,713 patients”. Arthroscopy. 2021;37(5):1369–1371. doi:10.1016/j.arthro.2021.03.021
20. Feeley BT, Liu S, Garner AM, Zhang AL, Pietzsch JB. The cost-effectiveness of meniscal repair versus partial meniscectomy: a model-based projection for the United States. Knee. 2016;23(4):674–680. doi:10.1016/j.knee.2016.03.006
21. Sochacki KR, Varshneya K, Calcei JG, et al. Comparing meniscectomy and meniscal repair: a matched cohort analysis utilizing a national insurance database. Am J Sports Med. 2020;48(10):2353–2359. doi:10.1177/0363546520935453
22. Johnson TR, Nguyen A, Shah K, Hogue GD. Impact of insurance status on time to evaluation and treatment of meniscal tears in children, adolescents, and college-aged patients in the United States. Orthop J Sports Med. 2019;7(10):2325967119875079. doi:10.1177/2325967119875079
23. Schairer WW, Nwachukwu BU, Lyman S, Allen AA. Race and insurance status are associated with surgical management of isolated meniscus tears. Arthroscopy. 2018;34(9):2677–2682. doi:10.1016/j.arthro.2018.04.020
24. Mather RC, Koenig L, Kocher MS, et al. Societal and economic impact of anterior cruciate ligament tears. J Bone Jt Surg Am. 2013;95(19):1751–1759. doi:10.2106/JBJS.L.01705
25. Mather RC, Hettrich CM, Dunn WR, et al. Cost-effectiveness analysis of early reconstruction versus rehabilitation and delayed reconstruction for anterior cruciate ligament tears. Am J Sports Med. 2014;42(7):1583–1591. doi:10.1177/0363546514530866
26. Gottlob CA, Baker CL, Pellissier JM, Colvin L. Cost-effectiveness of anterior cruciate ligament reconstruction in young adults. Clin Orthop Relat Res. 1999;367:272–282. doi:10.1097/00003086-199910000-00034
27. Stewart BA, Momaya AM, Silverstein MD, Lintner D. The cost-effectiveness of anterior cruciate ligament reconstruction in competitive athletes. Am J Sports Med. 2017;45(1):23–33. doi:10.1177/0363546516664719
28. Faucett SC, Geisler BP, Chahla J, et al. Meniscus root repair vs meniscectomy or nonoperative management to prevent knee osteoarthritis after medial meniscus root tears: clinical and economic effectiveness. Am J Sports Med. 2019;47(3):762–769. doi:10.1177/0363546518755754
29. Rogers M, Dart S, Odum S, Fleischli J. A cost-effectiveness analysis of isolated meniscal repair versus partial meniscectomy for red-red zone, vertical meniscal tears in the young adult. Arthroscopy. 2019;35(12):3280–3286. doi:10.1016/j.arthro.2019.06.026
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.