Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 11 » Issue 1
Bronchodilator efficacy of 18 µg once-daily tiotropium inhalation via Discair® versus HandiHaler® in adults with chronic obstructive pulmonary disease: randomized, active-controlled, parallel-group, open-label, Phase IV trial
Authors Yildiz P , Bayraktaroglu M, Gorgun D , Secik F
Received 5 August 2016
Accepted for publication 10 October 2016
Published 22 November 2016 Volume 2016:11(1) Pages 2859—2867
DOI https://doi.org/10.2147/COPD.S119114
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Richard Russell
Pinar Yildiz, Mesut Bayraktaroglu, Didem Gorgun, Funda Secik
Clinics of Chest Diseases, Yedikule Chest Diseases and Thoracic Surgery Training and Research Hospital, Istanbul, Turkey
Purpose: To compare the bronchodilator efficacy of 18 µg once-daily tiotropium inhalation administered via Discair® versus HandiHaler® in adults with moderate-to-severe chronic obstructive pulmonary disease (COPD).
Patients and methods: Fifty-eight patients with moderate-to-severe COPD were enrolled in this randomized, active-controlled, parallel-group, open-label, Phase IV non-inferiority trial. Patients were randomly assigned to a test group (n=29, inhalation with Discair) or a reference group (n=29, inhalation with HandiHaler). The primary efficacy parameter was the average maximum change in forced expiratory volume in 1 second (FEV1, in L). Change in forced vital capacity (FVC, in L), %FEV1 and %FVC, the standardized area under the response–time curve (AUC) for the absolute change in FEV1 and FVC, time to onset and peak of response, and safety data were also evaluated.
Results: The test inhaler was non-inferior to the reference inhaler in terms of maximum change in FEV1 at 24 h (unadjusted change: 0.0017 L [95% confidence interval [CI]: –0.0777, 0.0812]; change adjusted for time to reach maximum change in FEV1 and smoking in pack-years: 0.0116 L [95% CI: –0.0699, 0.0931]), based on a non-inferiority margin of 0.100 L. There were also no significant differences between the two groups in maximum change in FVC value from baseline (0.3417 L vs 0.4438 L, P=0.113), percent change from baseline (22.235 vs 20.783 for FEV1, P=0.662; 16.719 vs 20.337 for FVC, P=0.257), and AUC0–24 h (2.949 vs 2.833 L for FEV1, P=0.891; 2.897 vs 4.729 L for FVC, P=0.178). There were no adverse events, serious adverse events, or deaths.
Conclusion: Our findings show that the Discair was non-inferior to the HandiHaler. More specifically, these devices had similar clinical efficacy in terms of time-dependent response over 24 h for patients with moderate-to-severe COPD.
Keywords: non-inferiority, tiotropium, Discair®, HandiHaler®, bronchodilator efficacy, spirometry
Introduction
Chronic obstructive pulmonary disease (COPD) is characterized by persistent and progressive airflow limitation and reduced lung function,1,2 and is estimated to become the third leading cause of mortality and the seventh leading cause of morbidity worldwide by 2030. COPD also has a substantial impact on health-related quality of life (HRQoL) and requires significant health care expenditures.3–6
Tiotropium bromide is an inhaled long-acting anticholinergic bronchodilator, and a single dose per day is effective for treatment for moderate-to-severe COPD. Its therapeutic benefits include sustained bronchodilation over 24 h, improved efficacy of lung function, better HRQoL, and reduced acute exacerbations and hospitalization.7–14 Previous studies have consistently reported that this drug has favorable tolerability and the potential to improve treatment adherence and compliance of patients with moderate-to-severe COPD.7,8,12
Tiotropium bromide has been available as a single-dose (18 μg) dry-powder capsule delivered via a HandiHaler® (Boehringer Ingelheim Pharma GmbH & Co, KG, Biberach, Germany) since 200215 and as an aqueous solution (5 μg once daily) delivered via the propellant-free multidose Soft Mist™ inhaler (SMI) (Boehringer Ingelheim Pharma GmbH & Co, KG, Biberach, Germany) since 2007.16 Physicians worldwide have prescribed this drug, and there are >25 million patient-years of use.7,8,11 HandiHaler is the most prescribed COPD maintenance treatment inhaler worldwide, and has >31 million patient-years of use.17 Adherence to COPD treatments, particularly long-acting bronchodilators, is considered critical for the management of stable COPD.13,18 The therapeutic success of inhaled medications relies on the efficacy of the drug, the characteristics of the inhaler (such as ease of use), the complexity of the regimen, the frequency of dosing, and patient preference for a particular inhalation device.12,18–27
Operational complexity and a need for the patient to generate an inspiratory effort to overcome the internal resistance are the main limitations of several single-dose dry-powder inhalers (DPIs), which were introduced over the last few years.28–30 Development of new inhalers with features that make it easier for patients to deliver the same dose of tiotropium may provide substantial cost benefits for treatment of COPD.31 A previous study compared patient preference and ease of use between Diskus® and HandiHaler® among 60 COPD patients who were naive to these inhalers but experienced with others. The results indicated that there were similar numbers of instruction steps for these inhalers, but that more patients preferred Diskus (43 patients) than HandiHaler (16 patients).32
Another study assessed inhaler technique and patient preferences in adults with asthma (n=194) or COPD (n=107) who were undergoing treatment with Aerolizer®, Autohaler®, Breezhaler®, Diskus, HandiHaler, MDI without Spacer®, Miat-haler®, Novolizer®, Respimat®, and/or Turbohaler®. The HandiHaler and Diskus were the most commonly used inhalers among COPD patients (26% and 21%, respectively). The patients reported that the Diskus was the second easiest to use (after Turbohaler) and the second favorite-for-daily-use (after Novolizer). HandiHaler use was associated with increased likelihood of performing errors in inhalation technique (odds ratio: 3.71, 95% confidence interval [CI]: 1.38, 10.2) and it also had poorer performance than the Diskus.33
COPD occurs most often in the elderly, who are also more prone to the adverse effects of diseases in general.34 Given the rise of error rates in use of inhalation devices with increasing age,35 easy-to-use multidose DPIs are considered as especially beneficial for elderly COPD patients because they can improve patient adherence to treatment and thereby improve long-term outcome.19,36
Thus, Neutec Ar-Ge San & Tic A.S. Istanbul, Turkey developed Discair® to provide a patient-friendly and easy-to-use alternative for tiotropium therapy. Discair is a true multidose DPI device that contains 60 doses in an indexed foil–foil aluminum strip. The dose blister is only opened just prior to patient inspiration and there is no need for cleaning or reloading. Discair is an easy-to-use DPI that requires only 3 steps, and the inhalation flow rate has minimal effect on dose emission.37
The present study compared the bronchodilator efficacy of 18 μg once-daily tiotropium inhalation administered via Discair and HandiHaler (reference inhaler) in patients with moderate-to-severe and stable COPD.
Methods
Study population
Fifty-eight of 67 initially recruited patients with moderate-to-severe COPD fulfilled the eligibility criteria and were included in this randomized, active-controlled, parallel-group, open-label, Phase IV non-inferiority trial (ClinicalTrials.gov Identifier: NCT02541006). This study was conducted at 2 consecutive visits (screening visit at study enrollment and treatment visit up to 24 h after inhalation therapy) between November 2014 and April 2015.
All patients were aged 40 years and older and had clinically confirmed moderate-to-severe COPD. COPD severity was defined as a post-bronchodilator forced expiratory volume in 1 second (FEV1)/forced vital capacity (FVC) ratio of ≤0.70 and an FEV1 of ≤80% of predicted normal value at the screening. The enrolled patients also had no exacerbations within last 4 weeks, were current/former smokers with at least a 10 pack-year history of cigaret smoking, able to communicate with the investigator, accepted the procedures of study protocol, and provided signed and dated informed consent documents for participation. Additional inclusion criteria for female patients of childbearing age were negative pregnancy test results and use of acceptable contraceptive methods. The exclusion criteria were history of hypersensitivity to anticholinergics, diagnosis of asthma, history of allergic rhinitis and atopy, current or past history of lung cancer, known symptomatic prostatic hypertrophy or narrow-angle glaucoma requiring drug therapy, exacerbation of COPD or lower respiratory inflammatory disease requiring use of antibiotics, use of oral or parenteral corticosteroids within 4 weeks prior to the screening visit and/or during the run-in period, attenuated virus vaccination within 2 weeks prior to the screening visit and/or during the run-in period, recent history of myocardial infarction, acute ischemic cardiac disease or severe cardiac arrhythmia requiring drug therapy, and being pregnant or lactating or planning on becoming pregnant during the study period.
The study protocol was approved by the Ethics Committee of Istanbul University, Istanbul Faculty of Medicine (date of approval: February 21, 2014; reference number: 04) and the Turkish Medicines and Medical Devices Agency (April 16, 2014). All participants provided written informed consent following a detailed explanation of the objectives and protocol of the study. This study was conducted in accordance with the ethical principles stated in the Good Clinical Practice Guidelines and the Declaration of Helsinki.
Study procedures
Patients were evaluated at 4 consecutive visits: baseline (enrollment), screening, treatment, and 24 h after treatment. After confirmation of patient eligibility, data on socio-demographic characteristics (age, sex, and smoking status), body mass index (BMI), characteristics of COPD (newly diagnosed, formerly diagnosed, disease category, treatments, and exacerbations), and modified Medical Research Council (mMRC) scale dyspnea scores were recorded at the screening visit. For newly diagnosed and formerly diagnosed patients who were not on COPD medication, the screening visit was performed on the day of enrollment. For formerly diagnosed patients receiving COPD treatment, the day of the screening visit was based on the completion of a wash-out period, with the length determined by the specific medication. During the wash-out period, salbutamol (100 μg inhaler) was prescribed as a rescue medication.
The 58 eligible patients were randomly assigned to receive the standard dose of tiotropium (18 μg) with proven efficacy and safety for COPD indication, as dry powder for inhalation (Tiofix®) by Discair (test inhaler, n=29), or as dry-powder capsule for inhalation (Spiriva®) by HandiHaler (reference inhaler, n=29). Vital signs, physical examination findings, complete blood count (CBC), and blood biochemistry panels were recorded at the screening and treatment visits.
Patients in both groups were trained for the correct use of the inhalers. We considered all patients to have received the medication properly unless indicated otherwise in the case report form.
A single dose of the study drug was administered via the test or reference inhaler at 8:00 am on the day of the treatment visit. Spirometric measurements (FEV1 and FVC) were performed via spirometer (MIR SpiroLab III, Italy) for a period of 24 h at 11 different times: pretreatment (0 min, prior to the first dose) and posttreatment (15, 30 min and 1, 2, 3, 4, 6, 8, 12, and 24 h).
Study measures
The primary efficacy measures were the maximum changes in FEV1 and FVC (absolute change in L and %) from baseline and standardized area under the response–time curve (AUC) for both measures at 24 h after a single dose of tiotropium. The secondary efficacy measures were time to onset of response and peak response, and safety. Safety evaluation was based on adverse events reported by the patients and determined by physical examination and laboratory tests.
The AUC was calculated for the absolute change in FEV1 and FVC from baseline over the 24-h study period using the trapezoidal rule. The “time to onset of response” was defined as the time after drug administration when a 100 mL increase in FEV1 and a 150 mL increase in FVC first occurred. The “time to maximum response” over the 24-h study period was also recorded.
Statistical analysis
The sample size calculation was based on the primary efficacy measure of mean maximum change in FEV1 within 24 h after bronchodilator use. We estimated a sample size of 58 patients (29 per group) based on the non-inferiority hypothesis of maximum change (mL) in FEV1 from baseline in reference versus test groups with a non-inferiority margin of 0.100 L (H0: μr-μt ≥0.100; HA: μr-μt <0.100) and a standard deviation (SD) of 0.150 L. All statistical analyses were performed using SAS 9.3 TS Level 1M2 software (SAS Institute Inc., Cary, NC, USA). Data are expressed as mean (SD), count (%), and minimum–maximum where appropriate.
The non-inferiority of the test group relative to the reference group (primary efficacy variable: mean maximum change in FEV1 with in 24 h) was analyzed by analysis of covariance (covariates: time to maximum FEV1 response and smoking as pack-years) and calculation of 95% CI. For the comparison of other variables, superiority analyses were performed using a two-way Student t-test for numeric data and a chi-square and Fisher’s exact test for categorical data. A P-value <0.05 was considered statistically significant.
Results
Baseline characteristics
Table 1 shows the baseline characteristics of patients in the test and reference groups. The two groups were similar in terms of demographic characteristics, BMI, vital signs, CBC findings, and COPD characteristics. Most patients in the reference group (82.8%) and test group (62.1%) were ex-smokers, and 86.2% in each group were diagnosed with COPD category B based on the criteria of the Global Initiative for Obstructive Lung Disease (GOLD). Most patients in the test group (62.1%) and reference group (58.6%) did not experience exacerbations during the previous year, and 82.8% in each group were receiving COPD treatment. The distribution of mMRC scores were similar in the reference group (1: 27.6%, 2: 69.0%, 3: 3.4%) and the test group (1: 17.2%, 2: 72.4%, 3: 10.3%). All patients were compliant with their COPD therapies, and there were no records of poor inhalation technique during training.
Efficacy parameters
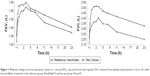
Table 2 shows the spirometry results for the reference and test groups. These results show no significant difference between the groups in FEV1 and FVC at the screening visit. Figure 1 shows the spirometric measurements during the 24 h after bronchodilator use. Analysis of these results indicated that the FEV1 and FVC values in the reference and test groups were not significantly different at 2, 4, 8, and 24 h (Table 3).
Additional comparisons of treatment efficacy (Table 3) indicated similar mean maximum change in FEV1 (reference: 0.2766 L, test: 0.2783 L). The difference of the mean maximum change in FEV1 between the study groups (unadjusted difference: 0.0017 L [95% CI: −0.0777, 0.0812]; difference adjusted for time to maximum change in FEV1 and pack-years of smoking: 0.0116 L [95% CI: −0.0699, 0.0931]) indicated that the test inhaler was non-inferior to the reference inhaler, based on a non-inferiority margin of 0.100 L. The test and reference groups were also similar in maximum change in FVC in L, percent maximum change in FEV1 and FVC, AUC of the response–time curves for FEV1 and FVC, and time to onset of response and maximum response (Table 3).
Safety parameters
There were no adverse events, serious adverse events, or deaths during the study. Vital signs, which were recorded at the pretreatment visit (0 h) and during the 24 h posttreatment follow-up, indicated no significant differences between the study groups. Biochemical and hematological findings were within normal limits in all patients, and there were no abnormal laboratory findings.
Discussion
This randomized, active-controlled, parallel-group, open-label, Phase IV non-inferiority trial showed that Discair was non-inferior (based on maximum change from baseline FEV1) to HandiHaler in the delivery of a single dose of 18 μg tiotropium to patients with moderate-to-severe COPD. Importantly, patients in the test and reference groups had similar baseline characteristics. The two treatments also produced similar time-dependent responses in absolute maximum change of FVC, percent change of FEV1 and FVC, and area under the response–time curve for FEV1 and FVC during the 24-h follow-up period. The two treatments also had similar times for onset of response and peak response, and favorable safety profiles.
FEV1 obtained during forced spirometry is the main parameter used to evaluate progression and extent of airflow obstruction, and to select optimal treatment strategies for COPD patients.1,2,38 Thus, we used maximum change in FEV1-related bronchodilator efficacy as the basis of a non-inferiority hypothesis in this study. The results indicated that the experimental product (Discair) was non-inferior to the active comparator product (HandiHaler). Moreover, Discair seemed to provide comparable clinical efficacy as HandiHaler in terms of time-dependent bronchodilator response associated with improvement in FEV1 and FVC, the most reliable and objective parameters available to measure airflow limitation.39
The mean improvement from baseline FEV1 was 0.04 L in the reference group and 0.05 L in the test group. The time to onset of response was 0.25 h in most patients and was similar in both groups. The maximum response was at 4.7 h (reference group) and 4.2 h (test group). This is a clinically significant bronchodilator response for patients with moderate-to-severe COPD, and further reinforces the benefit provided by tiotropium in management of COPD.38
Dyspnea is the most frequent reason that COPD patients seek medical advice, is the symptom that mostly limits the activities of daily living, and has the greatest negative impact on HRQoL in patients with COPD.40,41 Thus, evaluation of the success of a treatment for COPD is generally based on the presence of exacerbations and symptoms such as dyspnea.41
COPD is a complex heterogeneous disease and many studies have assessed the extent of airflow limitation by spirometric indices such as FEV1. However, FEV1 and other indices may be poor surrogate markers for symptoms.38 Accordingly, some studies have suggested use of multidimensional evaluation of COPD by inclusion of patient reported outcomes (PROs).38,42,43 The emphasis on use of FEV1, other markers of lung function, and other clinical variables (eg, chronic symptoms and exacerbations) may be valuable because of their potential modulatory effects.
The mMRC scale was developed to assess dyspnea, and it is currently the most widely used one-dimensional scale to evaluate PROs for COPD. Thus, current guidelines recommend its use for evaluation of COPD patients.43,44 Our findings indicated comparable efficacy of Discair and HandiHaler in terms of change of FEV1 and FVC from baseline for patients with mMRC scores of 1, and for patients with mMRC scores of ≥2. Hence, our findings indicate that both devices can generate the flow rates needed for currently available DPIs over a wide range of inspiratory flow rates39,45 for patients with stable COPD and varying severities of airflow limitation and dyspnea. Indeed, previous research reported that tiotropium markedly reduced the development of breathlessness and physical limitations by reducing progressive airflow obstruction and lung hyperinflation due to progressive destruction of supporting tissues and elastin fibers of the lungs.39,46,47 This translates into significant amelioration of clinical symptoms. Hence, some researchers have emphasized the importance of considering static lung volume in the multidimensional evaluation of COPD patients, because this can help to assess the full impact of COPD on a patient’s life.39,46,48
The baseline characteristics of patients in the Discair and HandiHaler groups were similar. In particular, all patients in both groups were males, their mean ages were similar (reference: 61.7 years old, test: 62.5 years old), most were ex-smokers, most had diagnoses of GOLD B disease, most were on COPD medications, and none had exacerbations in the previous year.
Age can influence the pharmacokinetics and pharmacodynamics of inhaled therapies and the mainstay of treatment for COPD.49 Analysis of patients who discontinued treatment in the UPLIFT trial of COPD patients indicated a higher likelihood of premature discontinuation in those who were older, female, and current smokers, and in those with poorer health status, more exacerbations, and more pack-years of smoking.50 Thus, the demographic and clinical similarities of our Discair and HandiHaler groups and our observation that all patients were compliant with therapy (with no records of poor inhalation technique during training) are major strengths of our study.
The Discair was designed for easier handling and minimal complexity. In fact, none of our patients reported difficulties in using the Discair during and following the training period, and there was no need to repeat respiratory function tests in any patients. A recent multinational real-world study of COPD patients identified a direct link between improved inhaler satisfaction (mainly durability, ergonomics, and ease-of-use) and increased treatment adherence.51 Hence, improved patient satisfaction with an inhaler may improve clinical and economic outcomes in patients with COPD.31,51 Notably, a recent study on the potential societal costs and benefits of improving treatment satisfaction, by use of a new tiotropium inhaler that was comparable to HandiHaler, estimated that 59% of patients preferred the new inhaler.31 Moreover, patients who switched to the new inhaler reported a ~32% improvement in satisfaction with treatment and a 9% increase in adherence.31
The HandiHaler is a complex single-dose DPI that requires 6 distinct steps for drug delivery and, like other unit-dose DPIs, cannot be considered a patient-friendly and easy-to-use device. Some of the disadvantages of the HandiHaler are: a) the need to place an individual capsule into the device immediately before each use, b) the need to discard the spent capsule and to clean the device and remove remnants of the hard gelatin capsule after each use, c) potential hygiene problems from the need to repeat the loading and cleaning steps, and d) difficulty of using the device by patients with impaired dexterity.19,28 Another disadvantage is that a patient’s inspiratory effort affects powder dispersion, and the operational complexity of the device can make it challenging to generate sufficient fine particles to ensure proper drug deposition in the lower airway in the elderly and patients with more severe airway obstruction.28,30 Also, the inhalation process sometimes needs to be repeated to ensure that the capsule is empty, and this increases the likelihood of dose variability and adds to the complexity of use.28,30
These problems with the HandiHaler motivated the development of a more patient-friendly and easier-to-use alternative for tiotropium therapy – Discair. Tiofix Discair is a multidose DPI device that contains 60 doses in an indexed foil–foil aluminum strip. The dose blister is only opened just prior to patient inspiration, and there is no need for cleaning or reloading. Discair is an easy-to-use DPI that requires only 3 steps for dose delivery. During dose delivery with Discair, there is no risk of direct contact with the drug, no need to open the cap (because this occurs automatically inside the device), no special inhalation maneuvers are needed, and there is no need to close the device. Moreover, inhalation flow rate characteristically has minimal effect on dose emission.37 All of our patients were able to use this device without any problems.
Our safety data indicated that 18 μg tiotropium dry-powder formulation delivered by Discair was well tolerated, as was the dry-powder capsule delivered by HandiHaler. This is consistent with previous trials, and confirms that tiotropium bromide inhalation powder is well tolerated in patients with COPD.10,52–54
Limitations
Major limitation of the present study seems to be the lack of the data from the female patients. Female patients were not included in the study since majority of moderate-to-severe COPD patients admitted to the study center were composed of males in accordance with predominance of COPD among males than females in Turkey, and also none of the female patients met the inclusion criteria. Nonetheless, this precludes the generalization and interpretation of the study findings for the general population.
Conclusion
Based on our measurements of FEV1, the bronchodilation efficacy of 18 μg tiotropium dry-powder formulation delivered by Discair was non-inferior to the dry-powder capsule delivered by the reference device (HandiHaler). These products also had similar clinical efficacy in terms of time-dependent bronchodilator response, and both had favorable safety profiles for patients with moderate-to-severe COPD. Importantly, patients in the test and reference groups had similar baseline characteristics. Thus, Discair is a safe and effective inhaler that is more patient-friendly for delivery of the active ingredient tiotropium (18 μg), a widely used drug with well-known efficacy and safety for treatment of COPD. Further larger scale and longer duration studies are required to assess the long-term safety and efficacy of Discair, the benefits of features related to handling and ease of use, and additional outcomes such as PROs and HRQoL.
Acknowledgments
This study was funded by Neutec Ar-Ge San & Tic AS (Turkey). The authors thank Cagla Ayhan, MD and Prof Sule Oktay, MD, PhD from KAPPA Consultancy Training Research Ltd. (Istanbul, Turkey) who provided help with medical writing and Kivanc Yuksel from Ege University Center For Drug Research & Development and Pharmacokinetic Applications (Izmir, Turkey) who performed the statistical analysis and was funded by Neutec Ar-Ge San & Tic AŞ (Turkey).
Disclosure
The authors report no conflicts of interest in this work.
References
Global Strategy for the Diagnosis, Management and Prevention of COPD, Global Initiative for Chronic Obstructive Lung Disease (GOLD) 2016. Available from: http://www.goldcopd.org/. Accessed May 1, 2016. | ||
Qaseem A, Wilt TJ, Weinberger SE, et al; American College of Physicians; American College of Chest Physicians; American Thoracic Society; European Respiratory Society. Diagnosis and management of stable chronic obstructive pulmonary disease: a clinical practice guideline update from the American College of Physicians, American College of Chest Physicians, American Thoracic Society, and European Respiratory Society. Ann Intern Med. 2011;155(3):179–191. | ||
Janson C, Marks G, Buist S, et al. The impact of COPD on health status: findings from the BOLD study. Eur Respir J. 2013;42(6):1472–1483. | ||
Lopez-Campos JL, Hartl S, Pozo-Rodriguez F, Roberts CM; European COPD Audit team. Variability of hospital resources for acute care of COPD patients: the European COPD audit. Eur Respir J. 2014;43(3):754–762. | ||
World Health Organization. COPD predicted to be third leading cause of death in 2030 [webpage on the Internet]. Geneva: World Health Organization; 2008. Available from: http://www.who.int/respiratory/copd/World_Health_Statistics_2008/en/index.html. Accessed December 25, 2015. | ||
Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2007;3(11):e442. | ||
Yohannes AM, Connolly MJ, Hanania NA. Ten years of tiotropium: clinical impact and patient perspectives. Int J Chron Obstruct Pulmon Dis. 2013;8:117–125. | ||
Alvarado-Gonzalez A, Arce I. Tiotropium bromide in chronic obstructive pulmonary disease and bronchial asthma. J Clin Med Res. 2015;7(11):831–839. | ||
Tashkin DP, Celli B, Senn S, et al; for UPLIFT study investigators. A 4-year trial of tiotropium in chronic obstructive pulmonary disease. N Engl J Med. 2008;359(15):1543–1554. | ||
Halpin DM, Dahl R, Hallmann C, Mueller A, Tashkin D. Tiotropium HandiHaler® and Respimat® in COPD: a pooled safety analysis. Int J Chron Obstruct Pulmon Dis. 2015;10:239–259. | ||
Verhamme KM, Afonso A, Romio S, Stricker BC, Brusselle GG, Sturkenboom MC. Use of tiotropium respimat soft mist Inhaler versus HandiHaler and mortality in patients with COPD. Eur Respir J. 2013;42(3):606–615. | ||
Bourbeau J, Bartlett SJ. Patient adherence in COPD. Thorax. 2008; 63(9):831–838. | ||
Halpern R, Baker CL, Su J, et al. Outcomes associated with initiation of tiotropium or fluticasone/salmeterol in patients with chronic obstructive pulmonary disease. Patient Prefer Adherence. 2011;5:375–388. | ||
Koehorst-ter Huurne K, Movig K, van der Valk P, van der Palen J, Brusse-Keizer M. Differences in adherence to common inhaled medications in COPD. COPD. 2015;12(6):643–648. | ||
Boehringer Ingelheim. Spiriva 18 microgram inhalation powder, hard capsule. Summary of Product Characteristics (SPC), Electronic Medicines Compendium (EMC). Available from: http://www.medicines.org.uk/emc/medicine/10039/SPC/Spiriva+18+microgram+inhalation+powder%2c+hard+capsule/. Accessed December 19, 2015. | ||
Boehringer Ingelheim. Spiriva Respimat 2.5 microgram solution for inhalation. Summary of Product Characteristics (SPC), Electronic Medicines Compendium (EMC). Available from: http://www.medicines.org.uk/emc/medicine/20134/SPC. Accessed December 19, 2015. | ||
Boehringer Ingelheim. Boehringer Ingelheim submits application in Europe to extend the indication for the use of tiotropium Respimat® to the treatment of asthma in adults aged 18 years and over [press release archive: asthma]. Ingelheim, Germany: Boehringer Ingelheim; 2013 [November 13]. Available from: http://www.boehringer-ingelheim.com/news/news_releases/press_releases/2013/13_november_2013_tiotropium.html. Accessed December 19, 2015. | ||
George J, Kong DCM, Thoman R, Stewart K. Factors associated with medication non-adherence in patients with COPD. Chest. 2005;128(5):3198–3204. | ||
Hanada S, Wada S, Ohno T, Sawaguchi H, Muraki M, Tohda Y. Questionnaire on switching from the tiotropium HandiHaler to the Respimat inhaler in patients with chronic obstructive pulmonary disease: changes in handling and preferences immediately and several years after the switch. Int J Chron Obstruct Pulmon Dis. 2015;10:69–77. | ||
Rand CS. Patient adherence with COPD therapy. Eur Respir Rev. 2005;14:97–101. | ||
Cazzola M, Matera MG. Novel long-acting bronchodilators for COPD and asthma. Br J Pharmacol. 2008;155(3):291–299. | ||
Bateman ED. Improving inhaler use in COPD and the role of patient preference. Eur Respir Rev. 2005;14:85–88. | ||
Chapman KR, Fogarty CM, Peckitt C, et al. Delivery characteristics and patients’ handling of two single-dose dry-powder inhalers used in COPD. Int J Chron Obstruct Pulmon Dis. 2011;6:353–363. | ||
Hesselink AE, Penninx BW, Wijnhoven HA, Kriegsman DM, van Eijk JT. Determinants of an incorrect inhalation technique in patients with asthma or COPD. Scand J Prim Health Care. 2001;19(4):255–260. | ||
Vincken W, Dekhuijzen PR, Barnes P; ADMIT Group. The ADMIT series – Issues in inhalation therapy. 4) How to choose inhaler devices for the treatment of COPD. Prim Care Respir J. 2010;19(1):10–20. | ||
Fromer L, Goodwin E, Walsh J. Customizing inhaled therapy to meet the needs of COPD patients. Postgrad Med. 2010;122(2):83–93. | ||
Mäkelä MJ, Backer V, Hedegaard M, Larsson K. Adherence to inhaled therapies, health outcomes and costs in patients with asthma and COPD. Respir Med. 2013;107(10):1481–1490. | ||
Gupta S. How to ensure the correct inhaler device is selected for each patient. Clin Pharmacist. 2009;1:322–323. | ||
Dahl R, Backer V, Ollgaard B, Gerken F, Kesten S. Assessment of patient performance of the HandiHaler compared with the metered dose inhaler four weeks after instruction. Respir Med. 2003;97(10): 1126–1133. | ||
Ruchi T, Vishal S, Neetu K, Vikramjeet S. Recent trends in DPI technology. Int Res J Pharm. 2012;3(1):27–34. | ||
Nicolai JL, Torvinen S, Miles R, Greaney MH, Howard DJ, Plich A. The potential societal cost benefits of increasing patient satisfaction by using an inhaler with improved features compared to Spiriva® HandiHaler® for the management of chronic obstructive pulmonary disease (COPD) in the UK. Value Health. 2015;18:A500. | ||
Van Der Palen J, Eijsvogel MM, Kuipers BF, Schipper M, Vermue NA. Comparison of the Diskus inhaler and the HandiHaler regarding preference and ease of use. J Aerosol Med. 2007;20(1):38–44. | ||
Chorão P, Pereira AM, Fonseca JA. Inhaler devices in asthma and COPD-an assessment of inhaler technique and patient preferences. Respir Med. 2014;108(7):968–975. | ||
Hanania NA, Sharma G, Sharafkhaneh A. COPD in the elderly patient. Semin Respir Crit Care Med. 2010;31(5):596–606. | ||
Taffet GE, Donohue JF, Altman PR. Considerations for managing chronic obstructive pulmonary disease in the elderly. Clin Interv Aging. 2014;9:23–30. | ||
Hodder R, Price D. Patient preferences for inhaler devices in chronic obstructive pulmonary disease: experience with Respimat Soft Mist inhaler. Int J Chron Obstruct Pulmon Dis. 2009;4:381–390. | ||
Neutec Tiofix Discair Product information. Available from: http://www.neutec.com.tr/pdf/solunum-sistemi-ilaclari/tiofix-18-mcg-Discair-inh-icin-Toz-Kub.pdf. Accessed January 14, 2016. | ||
Lopez-Campos JL, Calero C, Lopez-Ramirez C, Asensio-Cruz MI, Márquez-Martín E, Ortega-Ruiz F. Patient-reported outcomes and considerations in the management of COPD: focus on aclidinium. Patient Prefer Adher. 2015;9:95–104. | ||
Brashier B, Dhembare P, Jantikar A, et al. Tiotropium administered by a pressurized metered dose inhaler (pMDI) and spacer produces a similar bronchodilator response as that administered by a Rotahaler in adult subjects with stable moderate-to-severe COPD. Respir Med. 2007;101(12):2464–2471. | ||
Shavro SA, Ezhilarasu P, Augustine J, Bechtel JJ, Christopher DJ. Correlation of health-related quality of life with other disease severity indices in Indian chronic obstructive pulmonary disease patients. Int J Chron Obstruct Pulmon Dis. 2012;7:291–296. | ||
Vincken W, van Noord JA, Greefhorst AP, et al. Improved health outcomes in patients with COPD during 1 yr’s treatment with tiotropium. Eur Respir J. 2002;19(2):209–216. | ||
Lopez-Campos JL, Bustamante V, Munoz X, Barreiro E. Moving towards patient-centered medicine for COPD management: multidimensional approaches versus phenotype-based medicine – a critical view. Chronic Obstr Pulm Dis. 2014;11(5):591–602. | ||
Vestbo J, Hurd SS, Agustí AG, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med. 2013;187(4): 347–365. | ||
Fletcher CM. The clinical diagnosis of pulmonary emphysema; an experimental study. Proc R Soc Med. 1952;45(9):577–584. | ||
Sarinas PS, Robinson TE, Clark AR, Canfield J Jr, Chitkara RK, Fick RB Jr. Inspiratory flow rate and dynamic lung function in cystic fibrosis and chronic obstructive lung diseases. Chest. 1998;114(4):988–992. | ||
Celli B, ZuWallack R, Wang S, Kesten S. Improvement in resting inspiratory capacity and hyperinflation with tiotropium in COPD patients with increased static lung volumes. Chest. 2003;124(5):1743–1748. | ||
O’Donnell DE, Fluge T, Gerken F, et al. Effects of tiotropium on lung hyperinflation, dyspnea and exercise tolerance in COPD. Eur Respir J. 2004;23(6):832–840. | ||
Bartolome R Celli. Chronic obstructive pulmonary disease phenotypes and their clinical relevance. Proc Am Thorac Soc. 2006;3(6):461–465. | ||
Valente S, Pasciuto G, Bernabei R, Corbo GM. Do we need different treatments for very elderly COPD patients? Respiration. 2010;80(5):357–368. | ||
Decramer M, Molenberghs G, Liu D, et al; UPLIFT investigators. Premature discontinuation during the UPLIFT study. Respir Med. 2011; 105(10):1523–1530. | ||
Chrystyn H, Small M, Milligan G, Higgins V, Gil EG, Estruch J. Impact of patients’ satisfaction with their inhalers on treatment compliance and health status in COPD. Respir Med. 2014;108(2):358–365. | ||
Ichinose M, Fujimoto T, Fukuchi Y. Tiotropium 5 microg via Respimat and 18 microg via HandiHaler; efficacy and safety in Japanese COPD patients. Respir Med. 2010;104(2):228–236. | ||
Keating GM. Tiotropium bromide inhalation powder: a review of its use in the management of chronic obstructive pulmonary disease. Drugs. 2012;72(2):273–300. | ||
Hohlfeld JM, Sharma A, van Noord JA, et al. Pharmacokinetics and pharmacodynamics of tiotropium solution and tiotropium powder in chronic obstructive pulmonary disease. J Clin Pharmacol. 2014;54(4):405–414. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.