Back to Journals » Journal of Pain Research » Volume 10
Bone-anchored annular closure following lumbar discectomy reduces risk of complications and reoperations within 90 days of discharge
Authors Klassen PD, Bernstein DT, Köhler HP, Arts MP, Weiner B, Miller LE , Thomé C
Received 21 June 2017
Accepted for publication 1 August 2017
Published 26 August 2017 Volume 2017:10 Pages 2047—2055
DOI https://doi.org/10.2147/JPR.S144500
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Michael Schatman
Peter Douglas Klassen,1 Derek Thomas Bernstein,2 Hans-Peter Köhler,3 Mark P Arts,4 Bradley Weiner,2 Larry E Miller,5 Claudius Thomé6
On behalf of the Annular Closure RCT Study Group
1Department of Neurosurgery, St. Bonifatius Hospital, Lingen, Germany; 2Department of Orthopaedic Surgery, Methodist Hospital, Houston, TX, USA; 3Department of Neurosurgery, Asklepios Westklinikum Hamburg, Hamburg, Germany; 4Department of Neurosurgery, Haaglanden Medical Center, The Hague, The Netherlands; 5Miller Scientific Consulting, Inc., Asheville, NC, USA; 6Department of Neurosurgery, Medical University Innsbruck, Innsbruck, Austria
Purpose: The purpose of this study was to evaluate perioperative complications of lumbar discectomy with or without bone-anchored annular closure device (ACD) implant in patients at high risk of recurrent disc herniation.
Methods: This was a post hoc analysis of a randomized controlled trial that compared outcomes of lumbar discectomy with or without additional placement of an ACD. Patients presented with imaging evidence of lumbar disc herniation and radicular pain that was unresponsive to conservative care. Randomization occurred intraoperatively following discectomy completion and confirmation of annular defect width ≥6 mm. Main outcomes included serious adverse events (SAEs) from any cause, device- or procedure-related SAEs, and reoperations at the index level. The perioperative period included all outcomes occurring between the day of surgery and 90 days following hospital discharge.
Results: Analyses were performed on a modified intention-to-treat population consisting of 272 patients treated with ACD and 278 patients treated with lumbar discectomy only (controls). Mean patient age was 44 years, 59% were men, and mean body mass index was 26 kg/m2. Baseline patient characteristics and operative outcomes were comparable between groups. The risks of all-cause SAE (9.7% vs 16.3%, p=0.056), device- or procedure-related SAE (4.5% vs 10.2%, p=0.02), and index-level reoperation (1.9% vs 5.4%, p=0.03) were lower with ACD vs controls. In multivariable logistic regression, control group assignment and female gender were independently associated with higher risk of device- or procedure-related SAE and index-level reoperation, respectively.
Conclusion: In patients undergoing lumbar discectomy to treat symptomatic intervertebral disc herniation, adjunctive placement of an ACD reduces the risk for perioperative complications occurring through 90 days following hospital discharge.
Keywords: annular closure, complications, herniation, lumbar discectomy, randomized controlled trial, reoperation
Corrigendum for this paper has been published
Introduction
Lumbar discectomy for intervertebral disc herniation is one of the most commonly performed spine procedures.1 While lumbar discectomy is generally considered safe and provides initial symptomatic relief in most patients, the risk of perioperative complications ranges from 13% to 15%.2 As patients with large annular defects following lumbar discectomy have higher rates of recurrent disc herniation over long-term follow-up,3 it is plausible that these patients may experience greater risk of complications during the perioperative period. Perioperative complications place a large financial burden on patients, providers, hospitals, commercial payers, and federal health care agencies.4 Hospitals are highly incentivized to reduce complication rates, both in-hospital and following discharge.5 Treatment paths that reduce perioperative complication risks following lumbar discectomy have potential to improve patient outcomes and lower health care costs. We report here a post hoc analysis from a randomized controlled trial of a bone-anchored annular closure device (ACD) in patients at high risk of recurrent disc herniation after lumbar discectomy. We hypothesized that ACD implant following lumbar discectomy would reduce the risk for perioperative complications and associated reoperations occurring through 90 days following hospital discharge.
Methods
This prospective multicenter randomized controlled trial compared outcomes after lumbar discectomy with or without additional placement of an ACD. The primary objective of the study was to determine safety and effectiveness of adjunctive ACD placement through 2-year follow-up in patients at high risk of herniation recurrence.6 We report here a post hoc analysis of perioperative complication data from this study. The study was approved by the local ethics committee at each site and all patients provided written informed consent. The trial was prospectively registered at ClinicalTrials.gov (NCT01283438).
Baseline assessments included physical examination, neurologic examination with straight leg lift test, and anteroposterior, lateral, and flexion–extension x-rays. Disc herniation was confirmed with magnetic resonance imaging with T1- and T2-weighted axial and sagittal images and low-dose multiplanar computed tomography. Eligible patients were adults aged 21–75 years with single-level posterior or posterolateral disc herniation between L1 and S1, confirmation of neural compression on magnetic resonance imaging, positive straight leg raise or femoral stretch test, and radicular pain (visual analog scale ≥40) and back dysfunction (Oswestry Disability Index ≥40) that was unresponsive to at least 6 weeks of conservative treatment. Main exclusion criteria included disc height <5 mm at the index level, grade II or higher spondylolisthesis, or prior surgery at the index level. Complete inclusion and exclusion criteria in this study have been described elsewhere.6
All patients underwent single-level limited lumbar discectomy.7 Nuclear material removed from within or outside the disc was placed dry in a syringe and the volume was measured and recorded. Following the discectomy, intraoperative verification of annular defect between 4 and 6 mm in height and 6 and 10 mm in width was required; the latter requirement has been reported to increase recurrence risk.3,8 Eligible patients were then randomized (1:1) to additional ACD implant or discectomy only (controls). Randomization assignments were obtained intraoperatively through a web-based platform. Patients randomized to the control group underwent a standard wound closure procedure with no treatment of the annulus. Patients randomized to ACD underwent device implantation under fluoroscopic guidance as per the manufacturer’s surgical technique and instructions for use. Neither patients nor surgeons were blinded to treatment assignment, except for patients in the Netherlands (comprising 15% of the sample) who were blinded because of regional regulatory requirements.
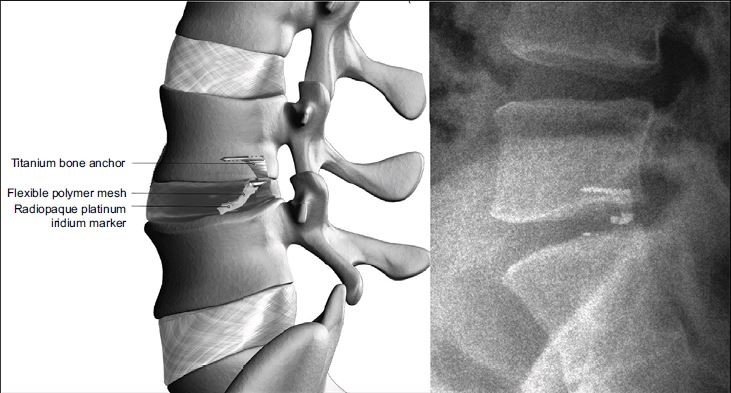
The ACD (Barricaid, Intrinsic Therapeutics, Inc., Woburn, MA, USA) is a permanent implant with two components – an occlusion component and an anchor component (Figure 1). The occlusion component consists of a flexible polymer mesh that is designed to prevent reherniation by physically blocking the annulus at the postsurgery defect and a platinum–iridium radiopaque marker to enable radiographic visualization. The anchor component consists of titanium alloy that is placed into either the caudal-adjacent or cranial-adjacent vertebral body to resist migration. The device is preassembled onto a single-use delivery tool.
Anteroposterior and neutral lateral radiographs were obtained prior to discharge. Immediate postoperative care, including discharge instructions, ambulation restrictions, and physical therapy recommendations, was provided at investigator discretion. Patients returned for planned in-clinic visits at 6 weeks and 3 months post-treatment. Complications and reoperations that occurred in hospital and through 90 days following hospital discharge were recorded and independently monitored for accuracy. An independent data safety monitoring board reviewed and adjudicated all adverse events, monitored study stopping rules, and had the authority to stop the study at any point.
A Bayesian adaptive sample size procedure to test for superiority of two co-primary endpoints at 2-year follow-up has been described elsewhere.6 Analyses were performed using a modified intention-to-treat population, which included all randomized control patients and all randomized ACD patients where the delivery tool was inserted through the skin. Continuous data were reported as mean and standard deviation unless otherwise noted. Categorical data were presented as counts and percentages. Group comparisons of procedural data were performed using independent-samples t-test or Wilcoxon–Mann–Whitney test for continuous data and Fisher’s exact test for categorical data. Time-to-event data through 90 days following hospital discharge were analyzed using Kaplan–Meier methods; group comparisons were performed with a log-rank test. Univariate logistic regression was performed to determine the association of baseline patient characteristics with risk of perioperative complications. Independent variables included treatment group, age, gender, body mass index, smoking status, and index level. Variables that entered the univariate model at p<0.2 were considered for inclusion in a multivariate model. The multivariate model utilized a forward–backward stepwise elimination variable selection process that optimized the Akaike information criterion by assessing model fit penalized for the number of estimated parameters.9 Statistical analyses were performed using SAS v9.4 (SAS Institute, Cary, NC, USA) and R v3.3.2 (R Foundation for Statistical Computing, Vienna, Austria ).
Results
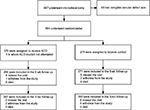
A total of 647 patients met the initial study entry criteria and underwent lumbar discectomy. After exclusion of 93 patients because of ineligible annular defect dimensions, 554 patients were randomly allocated to ACD (n=276) or control (n=278) at 21 centers in six European countries between December 2010 and October 2014. A list of participating centers and investigators is provided in Table S1. Four patients randomized to ACD did not undergo device implantation because of anatomical considerations; therefore, the modified intention-to-treat population consisted of 272 patients treated with ACD and 278 patients treated with limited discectomy only. Follow-up compliance through the 3-month visit was 98% with ACD and 95% with control (Figure 2).
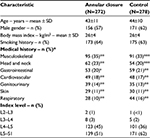
Baseline patient characteristics were comparable between groups (Table 1). Mean patient age was 44 years, 59% were men, and mean body mass index was 26 kg/m2. Surgery was most frequently performed at L5–S1 (56%) or L4–L5 (41%). Intraoperative findings were similar between groups including mean volume of nucleus removed (1.3 mL) and mean annular defect area (39 mm2). Surgery time (skin-to-skin) was longer in the ACD group owing to the additional time required for implant placement (70 vs 52 minutes, p<0.001). Median blood loss (50 mL) and hospital stay (3 days) were identical between groups.
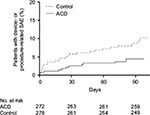
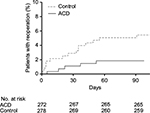
Through 90 days following hospital discharge, the cumulative probability of all-cause serious adverse event (SAE) was lower with ACD vs control (9.7% vs 16.3%, p=0.056). The cumulative probability of a device- or procedure-related SAE through 90 days following hospital discharge was 4.5% with ACD and 10.2% with control (p=0.02) (Figure 3). The most common of these SAEs was herniation at the index level, reported in six (2.2%) ACD patients and 19 (6.8%) control patients (p=0.01) (Table 2).
The risk of reoperation at the index level over this period was also lower with ACD (1.9% vs 5.4%, p=0.03) (Figure 4). In the control group, 18 index-level reoperations were performed in 15 patients. These included discectomy (n=8), discectomy with ACD implant (n=2), hematoma evacuation (n=3), wound revision (n=1), and multiple (four) wound revisions (n=1). In the ACD group, six index-level reoperations were performed in five patients including discectomy (n=3), decompression with subsequent fusion (n=1), and implant removal (n=1). The risk of reoperation for recurrent herniation was lower in the ACD group vs controls (0.7% vs 4.0%, p=0.02).
In univariate logistic regression, treatment group was the only variable that was associated with occurrence of a device- or procedure-related SAE (control vs ACD: odds ratio [OR]=2.2, p=0.03). Control group assignment (OR=3.1, p=0.03) and female gender (OR=2.8, p=0.03) were associated with greater risk of index-level reoperation in the univariate model (Table 3). In each multivariable model, control group assignment and female gender were independently associated with greater complication risks (Table 4). Comparing women to men in the control group, the probabilities were 13.1% vs 7.0% for a device- or procedure-related SAE and 8.4% vs 3.5% for index-level reoperation. In the ACD group, the probabilities were 6.0% vs 3.2% for a device- or procedure-related SAE and 3.4% vs 0.6% for index-level reoperation.
Discussion
The results of this post hoc analysis from a randomized controlled trial demonstrated that reherniation was the most common perioperative complication following lumbar discectomy for disc herniation. Further, adjunctive use of an ACD following lumbar discectomy reduced the risk for perioperative complications and associated reoperations compared to lumbar discectomy alone. To the authors’ knowledge, this is the first study to characterize perioperative complications in patients with large annular defects following lumbar discectomy.
In the current economic climate with heightened scrutiny on health care resource utilization, hospitals continually face a delicate balance between limiting unnecessarily long hospitalizations and reducing the risk of complications and readmissions following discharge. With Diagnosis-Related Group-based flat payment schedules10 and financial penalties for higher-than-average readmission rates set forth by the Hospital Readmission Reduction Program,11 adoption of therapies that reduce in-hospital and postdischarge complications may improve patient outcomes and potentially increase hospital margins. Given that 480,000 discectomy procedures are performed annually in the USA12 and that adjunctive ACD implant reduced perioperative complication risk by over 50%, it is plausible that significant cost savings may be realized with routine ACD placement in patients undergoing lumbar discectomy who are at high risk for reherniation based on annular defect size.
We found that in patients with large annular defects following lumbar discectomy for disc herniation, perioperative complication risk was higher in women than men. This is in agreement with other studies that have reported female gender as an independent risk factor for inferior outcomes following lumbar disc surgery.13 However, we are unaware of other studies that have examined the influence of gender on perioperative complications following lumbar discectomy. It is plausible that the greater complication risk in women was confounded by preoperative status. In the Swedish Spine Register of over 15,000 patients, women scheduled for lumbar disc surgery reported inferior clinical status compared to men including greater pain severity, inferior walking ability, higher consumption of analgesics, and greater disability.14 In the current study, no other preoperative variable was independently associated with perioperative complication risk. Still, the possible influence of unmeasured preoperative status variables on the elevated complication risk in women remains a possibility. Despite the higher risk of perioperative complications in women following lumbar discectomy, the risk of device- or procedure-related SAE and index-level reoperation in women remained lower with ACD vs controls.
Strengths of this study included a randomized design, rigorous study entry criteria, and adjudicated complication reporting. There were also several limitations of the study that warrant consideration. First, as investigators and most patients were aware of treatment allocation, the potential for expectation bias must be acknowledged. Second, while SAEs were reported and reviewed in a standardized fashion, the decision to perform surgery was based on patient willingness and surgeon recommendations. Third, the results of this study are applicable to patients with large annular defects following lumbar discectomy. Perioperative complication risk in patients with small vs large annular defects has not been reported to date.
Conclusion
In patients undergoing lumbar discectomy to treat symptomatic intervertebral disc herniation, adjunctive placement of an ACD reduces the risk for perioperative complications occurring through 90 days following hospital discharge.
Disclosure
Intrinsic Therapeutics provided support for the conduct of the study, analysis of the data, and preparation of this manuscript. PDK, CT, and LEM are consultants to Intrinsic Therapeutics. The authors report no other conflicts of interest in this work.
References
Weinstein JN, Lurie JD, Olson PR, Bronner KK, Fisher ES. United States’ trends and regional variations in lumbar spine surgery: 1992–2003. Spine (Phila Pa 1976). 2006;31(23):2707–2714. | ||
Sherman J, Cauthen J, Schoenberg D, Burns M, Reaven NL, Griffith SL. Economic impact of improving outcomes of lumbar discectomy. Spine J. 2010;10(2):108–116. | ||
Carragee EJ, Han MY, Suen PW, Kim D. Clinical outcomes after lumbar discectomy for sciatica: the effects of fragment type and anular competence. J Bone Joint Surg Am. 2003;85-A(1):102–108. | ||
Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360(14):1418–1428. | ||
Centers for Medicare & Medicaid Services. Hospital-Wide (All-Condition) 30-Day Risk-Standardized Readmission Measure; 2011. Available from: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/MMS/downloads/MMSHospital-WideAll-ConditionReadmissionRate.pdf. Accessed April 15, 2017. | ||
Klassen PD, Hes R, Bouma GJ, et al. A multicenter, prospective, randomized study protocol to demonstrate the superiority of a bone-anchored prosthesis for anular closure used in conjunction with limited discectomy to limited discectomy alone for primary lumbar disc herniation. Int J Clin Trials. 2016;3(3):120–131. | ||
Spengler DM. Lumbar discectomy. Results with limited disc excision and selective foraminotomy. Spine (Phila Pa 1976). 1982;7(6):604–607. | ||
Kim KT, Lee DH, Cho DC, Sung JK, Kim YB. Preoperative risk factors for recurrent lumbar disk herniation in L5-S1. J Spinal Disord Tech. 2015;28(10):E571–E577. | ||
Zhang Z. Variable selection with stepwise and best subset approaches. Ann Transl Med. 2016;4(7):136. | ||
Fourie C, Biller-Andorno N, Wild V. Systematically evaluating the impact of diagnosis-related groups (DRGs) on health care delivery: a matrix of ethical implications. Health Policy. 2014;115(2–3):157–164. | ||
McIlvennan CK, Eapen ZJ, Allen LA. Hospital readmissions reduction program. Circulation. 2015;131(20):1796–1803. | ||
Gray DT, Deyo RA, Kreuter W, et al. Population-based trends in volumes and rates of ambulatory lumbar spine surgery. Spine (Phila Pa 1976). 2006;31(17):1957–1963. discussion 1964. | ||
Stromqvist F, Ahmad M, Hildingsson C, Jonsson B, Stromqvist B. Gender differences in lumbar disc herniation surgery. Acta Orthop. 2008;79(5):643–649. | ||
Stromqvist F, Stromqvist B, Jonsson B, Karlsson MK. Gender differences in patients scheduled for lumbar disc herniation surgery: a National Register Study including 15,631 operations. Eur Spine J. 2016;25(1):162–167. |
Supplementary materials
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.