Back to Journals » Clinical and Experimental Gastroenterology » Volume 16
Body Mass Index Profile of Adult Patients with Inflammatory Bowel Disease in a Multicenter Study in Northeastern Brazil
Authors Lima JS , Brito CAAD , Celani LMS , Araújo MVTD, Lucena MTD, Vasconcelos GBS, Lima GAS, Nóbrega FJF, Diniz GTN , Lucena-Silva N, Maio R , Martinelli VF
Received 23 August 2023
Accepted for publication 7 November 2023
Published 14 November 2023 Volume 2023:16 Pages 213—224
DOI https://doi.org/10.2147/CEG.S436699
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Santosh Shenoy
Jones Silva Lima,1 Carlos Alexandre Antunes de Brito,1– 4 Lívia Medeiros Soares Celani,2,5 Marcelo Vicente Toledo de Araújo,2,6 Maurilio Toscano de Lucena,7 Graciana Bandeira Salgado Vasconcelos,1,2,8 Gustavo André Silva Lima,1,2,4 Fernando Jorge Firmino Nóbrega,6 George Tadeu Nunes Diniz,9 Norma Lucena-Silva,9 Regiane Maio,10 Valéria Ferreira Martinelli1,2,4
1Department of Gastroenterology, Hospital das Clínicas, Federal University of Pernambuco, Recife, Pernambuco, Brazil; 2Department of Gastroenterology, Member of Organização Brasileira de Doença de Crohn e Retocolite – GEDIIB, São Paulo, Brazil; 3Department of Internal Medicine, Center of Medical Sciences of Federal University of Pernambuco, Pernambuco, Brazil; 4Department of Immunology, Autoimune Research Institute, Recife, Pernambuco, Brazil; 5Department of Gastroenterology, Onofre Lopes Hospital, Federal University of Rio Grande do Norte, Natal, Rio Grande do Norte, Brazil; 6Department of Gastroenterology, Lauro Wanderley Hospital, Federal University of Paraíba, João Pessoa, Paraíba, Brazil; 7Department of Coloproctology, Barão de Lucena Hospital, Recife, Pernambuco, Brazil; 8Department of Gastroenterology, University of Pernambuco, Recife, Pernambuco, Brazil; 9Aggeu Magalhães Institute, Oswaldo Cruz Foundation, Recife, Brazil; 10Department of Nutrition, Federal University of Pernambuco, Recife, Pernambuco, Brazil
Correspondence: Carlos Alexandre Antunes de Brito, Division of Immunology, Autoimune Research Institute, 715 Rui Barbosa Avenue, Recife, Pernambuco, 52011-040, Brazil, Tel + 55 81 31480101, Email [email protected]
Purpose: Inflammatory bowel disease (IBD) is a disease of increasing prevalence in developing countries. Obesity has emerged as a potential risk for IBD; however, the data in the literature are conflicting, and relevant studies in Brazil are limited. Here, we report body mass index profile (BMI) of patients with IBD treated at reference centers in three states of northeastern Brazil.
Patients and Methods: Observational descriptive study conducted from January 2021 through December 2021 in patient with IBD.
Results: Of 470 patients with IBD, 194 (41%) were classified as normal weight, 42 (9%) as underweight, 155 (33%) as overweight, and 79 (17%) as obese; CD patients were significantly more likely to be underweight than UC patients (p=0.031)Overweight patients were older (median age: 47 years) than normal-weight and underweight patients at diagnosis (38.5 and 35.5 years, respectively [p< 0.0001]). IBD onset and diagnosis among overweight and obese individuals were associated with older age. More extensive disease behavior patterns predominated in UC, while forms associated with complications were prevalent in CD, irrespective of nutritional status. There was a higher frequency of compatible symptoms with axial joint inflammation among obese patients (p=0.005) and a lower frequency of compatible symptoms with peripheral joint inflammation in underweight patients (p=0.044) than in patients of normal weight. No significant difference in the frequency of different drug or surgical treatments was observed among the groups.
Conclusion: Despite the predominance of overweight and obesity in patients with IBD, no differences in the patterns of disease were seen between the overweight and normal-weight groups; however, obesity was associated with IBD onset in older adults and a higher frequency compatible symptom with axial joint inflammation. These data reinforce the importance of monitoring the nutritional status of IBD patients and the need for a multidisciplinary approach, as recommended in the current guidelines.
Keywords: Crohn’s disease, ulcerative colitis, obesity, overweight
Introduction
Inflammatory bowel disease (IBD) is a term encompassing Crohn’s disease (CD) and ulcerative colitis (UC), immunologically mediated diseases of multifactorial etiology characterized by chronic inflammation of the gastrointestinal tract.1,2 Although highest in North America and Europe, the prevalence of IBD has seen a progressive increase in Asia and Latin America over recent years.2,3 Based on data from a public service database, the prevalence of the disease in Brazil has increased progressively, rising from 30 to 100 cases per 100,000 population between 2012 and 2023.3 This increase may be related to the progressive increase in industrialization/urbanization, which has led to changes in lifestyle, including changes in diet, smoking, and physical inactivity.4–7
Obesity has been associated with increased IBD prevalence and severity; however, its epidemiological and pathophysiological relationship with IBD remains to be established.8–12 The prevalence of excess weight and obesity among patients with IBD has increased greatly over recent decades.13,14 The prevalence of obesity among patients with IBD has been estimated at 15% to 40%, with an additional 20% to 40% being classified as overweight.11,14
The accumulation of adipose tissue, especially visceral fat, can increase the release of proinflammatory cytokines, which can negatively affect clinical and surgical outcomes. In addition, changes in the microbiota and the reduced bioavailability of drugs for the treatment of IBD in these patients contribute to unfavorable outcomes.5,10–12,15–21 However, the results in the literature are controversial about the presentation of worse outcomes in obese patients with CD and UC with higher body mass index (BMI), with some even suggesting a protective effect of obesity.6,7,22–28
Obesity may also not be a risk factor for IBD but rather a consequence of dietary changes in patients diagnosed with the condition, such as reduced anorexia and increased food intake with improved control of inflammation or side effects of drugs such as corticosteroids, as well as decreased physical activity in symptomatic patients with uncontrolled disease.15,29
At the other extreme, low weight in patients with IBD may be a risk factor for worse prognosis, and clinical and surgical complications and may be related to malabsorption, inflammatory activity, and decreased intake secondary to anorexia or gastrointestinal losses, among other factors. The frequency of low weight reported for patients with IBD varies, with estimates of up to 7% among patients with UC and up to 14% among those with CD; however, low weight is not always associated with an unfavorable outcome.14,18,27,29,30
Relatively few studies have assessed the prevalence of overweight and obesity among Brazilian patients with IBD.17,29,30 Accordingly, the objective of this study was to describe the BMI of patients with IBD treated at reference centers in three states in northeastern Brazil.
Patients and Methods
Study Design, Participants, and Ethics Approval
This was an observational descriptive study of patients with IBD followed up at specialized outpatient clinics at referral hospitals for the condition—Hospital das Clínicas da Federal University of Pernambuco, Hospital Universitário Oswaldo Cruz, and Hospital Barão de Lucena, in Recife/PE; Hospital Universitário Lauro Wanderley in João Pessoa/PB; and Hospital Universitário Onofre Lopes in Natal/RN. The study involved patients with IBD seen between January 2021 and December 2021.
IBD diagnosis was based on clinical, endoscopic, radiological, and histopathological criteria. BMI, based on the criteria of the World Health Organization, was used for nutritional classification. Patients for whom BMI information was not available were excluded from the analysis.
The study complied with the Declaration of Helsinki and was approved by the Federal University of Pernambuco Research Ethics Committee (CAAE 66718823.0.0000.8807). All patients were informed about the study and, after signing the informed consent form, were included in the study, without prejudice to their treatment if they refused to participate in the study.
Study Variables
The following demographic variables were analyzed: age, sex, race, smoking status, past appendectomy, and family history of IBD. The Montreal classification was used to describe the IBD phenotype, including age at diagnosis, location/extent of the disease, and disease behavior.31 The interval between the onset of symptoms and definitive diagnosis was also evaluated, as was the presence of extraintestinal manifestations (EIMs), such as musculoskeletal, cutaneous, ocular, hepatic, and vascular manifestations. The drug and surgical therapies instituted for IBD were included among the variables. World Health Organization criteria were used to define the BMI ranges—underweight: below 18.5, normal weight: between 18.5 and 24.9, overweight: between 25 and 29.9, and obese: above 30.
Additionally, we introduced an assessment of suspected cases of spondyloarthritis using the questionnaire by Queiroz et al. This questionnaire was designed to be applied by gastroenterologists, aiming to increase the suspicion and identification of spondyloarthritides. After a detailed evaluation by rheumatologists and analysis of imaging tests, it was found that the questionnaire has a sensitivity of 87.5% and 82.2% and a specificity of 89.8% and 87.4% for identifying cases of peripheral and axial spondyloarthritis, respectively.32 Axial spondyloarthritis was suspected when at least two of the following symptoms were present for more than 3 months: a history of lower back pain, morning lumbar stiffness for more than 30 minutes, and night awakening due to pain. Peripheral spondylitis was suspected when at least two of the following symptoms were present for more than 3 months: a history of peripheral joint pain, morning stiffness for more than 30 minutes, and joint swelling.32
Statistical Analysis
Absolute and relative frequencies of the variables were expressed as percentages. Continuous data were posteriorly tested for assumptions of normality using the Shapiro‒Wilk test. For normally distributed data, means were evaluated with the Student’s t-test. For non-normally distributed data, medians were evaluated using the Mann‒Whitney test.
To assess the significance of the results for the qualitative data, the chi-square test with Yates’ correction was used, when indicated. Fisher’s exact test was used. A p-value <0.05 was considered significant.
Results
Classification of IBD, Demographic Characteristics, and Antecedents Based on Nutritional Status
A total of 470 patients were enrolled between January 2020 and December 2021 from centers in the state of Pernambuco (n: 244, 52%), Rio Grande do Norte (n: 137, 29%), and Paraíba (n: 89, 19%). Of these patients, 178 were diagnosed with CD and 292 with UC. The mean age was 43 ± 15.87 years (mean ± standard deviation) and the median age was 42 years. Females comprised 63.8% of the cohort. There was a predominance of non-white patients, who represented 63.4% of the total (Table 1).
 |
Table 1 Demographic Profile of 470 Patients with Inflammatory Bowel Disease, Grouped by Body Mass Index Profile, at Reference Centers in Three States in Northeastern Brazil |
Among the 470 patients with IBD, 194 (41%) were normal weight, 42 (9%) were underweight, 155 (33%) were overweight, and 79 (17%) were obese (Figure 1). Among the CD patients, 71 (39.9%) were normal weight, 23 (12.9%) were underweight, 50 (28.1%) were overweight, and 34 (19.1%) were obese. Among the patients with UC, 123 (42.1%) were normal weight, 19 (6.5%) were underweight, 105 (36%) were overweight, and 45 (15.4%) were obese (Figure 1). There were significantly more underweight patients in the CD group than in the UC group (p=0.031).
Regarding demographic variables, most of the patients were female and mostly non-white, with no difference seen between the two groups. A family history of IBD was more common among patients with obesity, present in 20% of the patients; however, the difference between the groups was not significant (p=0.071). The time between the onset of symptoms and disease diagnosis was similar between the CD and UC groups (Table 1).
For age at diagnosis of IBD, overweight and obese patients were older (median: 47 years of age) than normal-weight and underweight patients (38.5 and 35.5 years of age, respectively) (p<0.001) (Table 1).
Clinical Profile
For age at diagnosis, the data showed that overweight and obese patients were diagnosed at an older age. As shown in Table 2, there was a higher frequency of overweight and obese patients in groups A2 (17–40 years of age) and A3 (>40 years of age) when compared with normal-weight patients, with the differences reaching significance (A2 Overweight, p=0.008; A2 Obese, p= 0.006; A3 Overweight, p= 0.001; A3 Obese, p= 0.009). Based on the multivariate analysis, we found that overweight individuals have a higher likelihood of being diagnosed with IBD in age groups A2 and A3. Specifically, this probability is 3.3 and 4.5 times higher, respectively, compared to individuals of normal weight (p=0.005 and p=0.001). Within the obese group, the chance of being diagnosed with IBD in the same age groups was 5.0 times higher than those of regular weight (p=0.012 and p=0.016).
 |
Table 2 Montreal Classification of 470 Patients with Inflammatory Bowel Disease, Grouped by Body Mass Index Profile, at Reference Centers in Three States in Northeastern Brazil |
The median times between the onset of symptoms and diagnosis were 8, 9, 11, and 12.5 months for normal-weight, underweight, overweight, and obese individuals, respectively; the differences among the groups were not significant. Meanwhile, most patients with UC had pancolitis as the disease presentation (120, 41.1%), also predominating between groups according to nutritional status (Table 2).
Most patients with CD had ileocolonic localization (66, 37.1%) and stenosing behavior (80, 44.9%), irrespective of nutritional status; however, the difference among the groups was not significant. Although there was a slightly higher frequency of colonic involvement (18.4%) than ileocolonic involvement (16.3%) in the overweight group, this difference was again not significant (Table 2).
Seventy-one patients (39.9%) with CD had perianal disease. In the analysis by group, perianal disease was present in 33.8%, 34.8%, 46%, and 47.1% of normal weight, underweight, overweight, and obese individuals, respectively; and although the frequency of perianal disease was higher among overweight and obese patients, the differences were not significant (p=0.196 and p=0.257, respectively) relative to normal-weight patients (Table 2).
The most common EIM was arthralgia, as an isolated symptom, which was present in 101 (21.5%) patients. According to BMI grouping, arthralgia was found in 46 (23.7%), 6 (14.3%), 35 (29.2%), and 14 (17.7%) normal weight, underweight, overweight, and obese patients, respectively; however, no difference was found between the normal-weight and the other groups (Table 3).
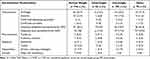 |
Table 3 Extraintestinal Manifestations in 470 Patients with Inflammatory Bowel Disease, Grouped by Body Mass Index Profile, at Reference Centers in Three States in Northeastern Brazil |
Regarding symptoms suggestive of axial inflammatory disease, there was a significantly higher prevalence of suspicion of axial spondyloarthritis in patients with obesity, with 27 (34.2%) of these patients meeting the criteria for suspicion, compared with 35 (18%) in the normal-weight group (p=0.005). When the data underwent multivariate analysis, the difference persisted, suggesting that obese patients are 2.2 times more likely to meet the suspicion criteria for axial spondyloarthritis than those of normal weight (p=0.029).
In the assessment of symptoms suggesting peripheral spondyloarthritis, we noted a lower occurrence in underweight patients compared to those of normal weight (4 [9.5%] vs 47 [24.2%], respectively), with this difference being statistically significant (p=0.044). Furthermore, there was a trend of higher suspicion of this type of spondyloarthritis in obese patients (28 [35.4%]), although this difference did not reach statistical significance (p=0.061). In the multivariate analysis, it was found that underweight individuals have a 76% reduced chance of presenting suspicion criteria for peripheral spondyloarthritis when compared to the normal weight group (p=0.036).
The occurrence of mucocutaneous, ocular, hepatobiliary, and vascular manifestations was 4.9%, 6.4%, 4.5%, and 2.1% in normal-weight, underweight, overweight, and obese patients with IBD, respectively, and did not differ among groups by nutritional status (Table 3).
Pharmacological and Surgical Treatment
Regarding drug therapies instituted, immunobiologicals were the most prescribed drugs, used by 88 (45.4%), 20 (47.6%), 67 (43.5%), and 38 (48.1%) normal-weight, underweight, overweight, and obese patients, respectively; however, no significant differences in the prescription of immunobiologicals were seen among the groups (p < 0.05). Similarly, no differences were observed in the frequency of use of immunosuppressants (azathioprine or methotrexate) and aminosalicylates among the groups. The use of biologicals associated with immunosuppressants, despite being more frequent among the overweight (36.7%) and obese (17, 51.5%) groups when compared to eutrophic (38, 48.1%) and thin (7, 38.9%) was not statistically significant (Table 4).
 |
Table 4 Treatments Instituted in 470 Patients with Inflammatory Bowel Disease, Grouped by Body Mass Index Profile, at Reference Centers in Three States of Northeastern Brazil |
The frequency of surgical treatment for normal-weight, underweight, overweight, and obese patients was 23.7%, 31%, 21.3%, and 25.3%, respectively; these intergroup differences were not significant (Table 4).
Discussion
In this study, we observed a predominance of BMI-related abnormalities in patients with IBD (59% of our cohort), with high BMI being more frequent (33% were overweight and 17% were obese). These results are consistent with those reported by Steed et al,33 who analyzed 480 followed-up patients in Scotland and reported that 38% of them were overweight while 18% were obese. A North American study involving 581 patients found higher frequencies than those observed in our study, with 32.7% presenting with obesity.27 In contrast, a study conducted in Italy found a prevalence of obesity of only 6.9% among 807 patients with IBD,23 while in France, Blain et al reported an obesity rate of 3% in a cohort of 62 patients.16
In the present study, overweight and obese patients were older than normal-weight patients at the time of diagnosis, as previously reported in several studies.14,16,18,23,24,27 In a cohort of 334 patients with CD patients in the United States, Johnson et al14 reported mean ages at diagnosis for patients who were overweight and obese of 42.3 and 44.3 years, respectively, higher than those for patients with low or normal weight (31.6 and 35.8 years, respectively). However, although our findings were consistent with those previously reported, the reason for the late onset of the disease in obese individuals remains unclear. A delay in diagnosis of this subgroup could explain the differences; however, this seems unlikely given that we did not find significant differences in the time between the onset of symptoms and diagnosis of the disease among the different BMI groups.
One explanation may be related to the pathophysiology of weight gain in older individuals. The onset of insulin resistance and adipokine dysregulation is associated with increasing age, with a consequent accumulation and redistribution of fat mass and a higher prevalence of obesity; this, combined with more sedentary practices, results in a positive energy balance. This increased frequency of obesity may trigger the activation of proinflammatory cytokines and may promote the development of IBD.10,11,21,34 In addition, the physiopathogenic mechanisms proposed for the association between obesity and IBD could necessitate a longer chronic inflammatory stimulus for the onset of the disease, resulting in delayed disease onset. These data may reinforce the hypothesis that obesity is not a consequence of IBD and that its high prevalence represents a risk factor for the condition, especially among older age groups.
It has been proposed that obesity may not be a risk factor for IBD but rather a consequence of the disease. Evidence for this is multifactorial and includes recovery of appetite with increased food intake due to better inflammation control after therapeutic response or the side effects of drugs such as corticosteroids, as well as a decrease in physical activity in symptomatic patients with uncontrolled disease.15,23,29
The current study only considered the therapies used at the time of evaluation and recruitment of patients, not having assessed the previous use of corticosteroids which could be a contributing factor to weight gain. However, it is essential to mention that corticosteroids are not part of the maintenance therapy for these patients, generally being prescribed to induce remission or treat relapses. For this reason, many studies do not consider their use in their analyses.17,21,29,33 Yet, the studies that took into account the history of corticosteroid use throughout the disease showed varied results. Most did not find a significant association between corticosteroid use and increased obesity in IBD patients.16,18,23,24,27
The study by Hass et al, which assessed the history of corticosteroid use in 148 patients with CD, showed that the frequency of use was higher in patients with a normal BMI (<25) compared to those with a high BMI (>25). However, this difference was not statistically significant (90% x 95%, p=0.41).18 Similarly, Blain et al, when comparing 62 cases of obese patients and 124 without obesity with CD, found no significant differences in corticosteroid use between the groups.16 Another study, by Kim et al, when evaluating 136 cases of UC, found a higher frequency of medical history of corticosteroid use among patients with BMI < 30 than those with BMI > 30, but without statistical significance (45.4% vs 29.6%; p=0.13).24 Interestingly, Flores et al reported a significantly higher frequency of corticosteroid use in the group of patients with CD with normal weight and underweight compared to cases of obese and overweight CD (p=0.01), but no difference for UC (p=0.51).27 Lastly, in a meta-analysis conducted by Hu et al, which included three additional studies not previously mentioned, it was observed that 50.7% of the 814 obese patients and 60.2% of the 2227 non-obese patients had used corticosteroids (p=0.85).28 On the other hand, the study by Losurto et al showed that obese patients with IBD consumed corticosteroids more frequently than non-obese IBD patients (66.6% vs 12.5%; p=0.02).23 This result deviates from the trend observed in most of the other mentioned studies.
Although the use of corticosteroids may have implications for the patient’s weight, current studies do not show a clear correlation between the consumption of these drugs and the increase in obesity in IBD patients. It is likely that other factors, beyond corticosteroid use, play a decisive role in these patients’ obesity.
On the other hand, it is essential to note that the high frequency of obesity reported among IBD patients in various studies may, in fact, reflect the obesity frequency of the population in the region in question. These analyses could be more accurate in case-control studies. In their research, Losurdo et al indicated a lower prevalence of obesity (6.9%) among IBD patients, a number very close to the control group (7.9%) and slightly lower than the prevalence observed in the European population (10.8%).23 Our study, like other observational studies on BMI in IBD patients, faces limitations due to not having a matched comparison group to analyze BMI frequency.16–18,21–24,27,29,33 Analyzing official data from the population in our region, we noticed an increased regional prevalence of overweight. In Brazil, statistics show that obesity prevalence grows with age, reaching 38.0% among women and 30.0% among men aged 40 to 59. Moreover, in the last two decades, there has been a significant increase in the number of individuals with excess weight (BMI ≥25 kg/m2) in the region, reaching a prevalence of 60.3%.35
In this study, we found more extensive disease patterns in patients with UC, with a predominance of pancolitis and greater ileocolonic involvement; for CD, there was a predominance of stenosing and/or penetrating behavior. However, there was no significant difference between the overweight and normal-weight groups, similar to the results of other studies.14,24,27 A cohort study recruiting 344 patients with CD, 46.7% of whom were overweight or obese, did not find any effect of excess weight on clinical presentation patterns or outcomes. Obesity did not influence the risk of corticosteroid use, hospitalization, intestinal resection, or penetrating complications and strictures.14
Multiple studies have reported an association between obesity/overweight and more severe inflammatory disease or unfavorable outcomes.16–18,20,21,36 In 2002, Blain et al, in the USA, reported an increased risk of perianal disease among 62 obese patients compared with that in matched non-obese controls with IBD, which was mainly characterized by a greater likelihood of abscess and fistula formation.16 Again, no differences in the pattern and behavior of the disease were observed between obese and normal-weight individuals. These findings were similar to those of a Brazilian study by Nascimento et al17 involving 64 patients with CD, in which an association was found between the presence of abscesses and obesity. The authors suggested that increased friction and sweating between the anoperineal skinfolds may stimulate maceration and secondary bacterial infections, thus favoring the formation of abscesses.16 In our sample, despite higher percentages of perineal disease and fistulectomy among overweight and obese individuals, no statistically significant differences were observed between these groups and the normal-weight group, similar to that reported in other studies.14,19,24,26,27 However, the study by Flores et al obtained conflicting results, and despite not finding differences between obese and normal weight individuals in the clinical classification and behavior of IBD based on the Montreal classification, it reported that obese patients with IBD had a significantly lower probability of receiving anti-TNF treatment, tolerated surgery, and hospitalized (55.8% vs 72.1%, p<0.001) than non-obese IBD patients.27
Among the EIMs, articular manifestations were the most frequent, occurring in one-fifth of the patients independently of the BMI. When we included patients with suspected spondyloarthritis, as determined using the standardized questionnaire of Queiro et al, we found a higher frequency of the criteria of axial spondyloarthritis in obese patients (p= 0.005) and a lower occurrence of the criteria of peripheral spondyloarthritis in underweight patients (p= 0.044).32 Studies analyzing these EIMs are rare. Singla et al found that arthralgia was the main joint manifestation among 209 patients with CD and that these joint manifestations were associated with excess weight.19
An association between obesity and immune-mediated inflammatory rheumatological diseases has been reported, especially ankylosing spondylitis, and may be related to the pro-inflammatory mechanisms induced by visceral fat through the synthesis of cytokines that act on the joint, similar to the hypothesis described for IBD. Obese patients with rheumatologic disease may present with higher rates of inflammatory activity and poor therapeutic responses, leading to less favorable outcomes.37–39 This potential inflammatory effect of obesity on joints could amplify the known immune-mediated association of IBD with spondyloarthritis, thereby explaining the higher frequency of axial disease observed in our study. The potential protective effect of being underweight on disease risk through a peripheral inflammatory component that we found in our study may reinforce these possibilities. Although this study identified differences in the frequencies of symptoms consistent with axial joint inflammation in obese individuals, using questionnaires with high sensitivity to identify spondyloarthritis, it has the limitation of not having used imaging tests or consultations with rheumatologists to confirm the diagnosis. Therefore, we cannot assert with certainty that all identified cases are of an inflammatory nature.
The frequency of underweight in this study was 8.9% and was higher among patients with CD (12.9%) than among those with UC. These results differ from those reported in other studies.14,19,33 Steed et al identified a frequency of underweight of 2% among a sample of 480 patients with IBD and a frequency of 3% among patients with CD.33 Two Brazilian studies reported a frequency similar to that found in our study. Back et al, in São Paulo, southeastern Brazil, reported a frequency of underweight of 8.5% among 141 patients with IBD and 11.1% and 6.9% among those with CD and UC, respectively.29 Rocha et al,30 in Northeastern Brazil, reported a frequency of underweight of 9.8% in a sample of 101 patients with IBD and 14% among patients with CD. In the official data of an anthropometric evaluation of the Brazilian population, the frequency of low weight (BMI <18.5 kg/m2) corresponds to only 1.6% among patients aged over 18 years.35
The effects of IBD-associated malnutrition are multifactorial and involve an inflammatory process in the mucosa that leads to diarrhea, protein loss, nutrient malabsorption, anorexia, and increased catabolism, especially in patients with CD and with active disease, and these effects can be aggravated by surgical procedures.
Regarding the therapies instituted, we did not find differences in the frequency of use of the different drug therapies between patients with CD and those with UC. Studies have suggested that the response to anti-TNF and immunosuppressive drugs such as azathioprine and 6-mercaptopurine may be reduced in patients with a higher BMI.12,40 Biological drugs were the most prescribed drugs, used by 45% of patients, and with similar frequency in all nutritional status groups.
Pharmacokinetic studies have suggested that the effectiveness of biological therapy is reduced in patients with obesity due to increased drug clearance, a reduced drug half-life, and low trough drug concentrations, which may be higher in users of anti-TNF agents as a result of rapid proteolysis and a phenomenon known as the “TNF sinker”, whereby increased levels of TNF secreted in adipose tissue sequester anti-TNF drugs, thus reducing their effectiveness in serum.9 Kurnool suggested that for every 1 kg/m2 increase in BMI, there is a 4% increase in the risk of treatment failure and an 8% increase in the risk of surgery and hospitalization in patients with UC.41
Although anti-TNF agents were the most prescribed therapeutic class of biologics (87.7%), we did not assess whether there were differences in the frequency of dose optimization and changes in therapy based on nutritional status.
The high frequency of the use of biologics reported in this study may be related to a more severe disease pattern, as has also been described for patients in other Brazilian studies.42,43
In our study, as in many others published in the literature, the assessment was based solely on the nutritional status determined by BMI. However, other indicators, such as arm muscle area (AMA) and triceps and subscapular skinfolds (TST+SST), which are useful for identifying total, muscle, and fat mass, were not considered. These parameters have the potential to enrich future studies by providing a more comprehensive nutritional analysis of patients.
The frequent findings of BMI abnormalities in this study reinforce the importance of identifying these patients and facilitating their nutritional recovery. Obesity is associated with cardiovascular risks and diabetes mellitus, among other diseases, regardless of the absence of unfavorable outcomes for many of the variables analyzed. These risks can be aggravated when associated with underlying IBD, in addition to being associated with depression, fatigue, and reduced social interaction, which negatively affects quality of life. Malnutrition is associated with a higher risk of infections in patients who are often immunosuppressed, as well as an increased risk of complications in patients undergoing surgical procedures, especially those with CD.
Conclusions
The results of this multicenter study showed a predominance of excess weight among patients with IBD, with onset and diagnosis of the condition associated with older age, findings that are in agreement with those reported in the literature. Although we found more extensive disease patterns for IBD, which are often associated with complications and difficult-to-control disease, no difference in clinical profiles or the frequency of surgical procedures were found between the overweight and normal-weight groups. Compatible symptoms with axial joint dysfunction were more frequent among obese individuals, indicating the need for more studies to evaluate this association. The dissemination of these results may increase awareness of the importance of monitoring the nutritional status of patients with IBD and the need for a multidisciplinary approach, in accordance with current guidelines.
Data Sharing Statement
All data generated or analyzed during this study are included in the published article.
Ethics Approval and Consent to Participate
Written informed consent for publication was obtained from the patients before information was collected. The patients also provided written consent for the inclusion of personal and clinical details in this study. The study was approved by the Research Ethics Committee of the Centre of Medical Sciences, Federal University of Pernambuco (CAAE [certificate of presentation of ethical appreciation]: 31047320.7.0000.5208).
Consent for Publication
The patients provided written, informed consent for the inclusion of personal and clinical details in this study.
Acknowledgments
We thank the Autoimmune Institute for Research and Continuing Education for its support in the development of this project.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was funded by Takeda Pharmaceuticals, Brazil, under a specific grant (IISR-2020-102789). The sponsors did not participate in the design of the study, the analysis of the results, or the content of the publication.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Weimers P, Munkholm P. The Natural History of IBD: lessons Learned. Curr Treat Options Gastroenterol. 2018;16(1):101–111. doi:10.1007/s11938-018-0173-3
2. Ng SC, Shi HY, Hamidi N, et al. Worldwide incidence and prevalence of inflammatory bowel disease in the 21st century: a systematic review of population-based studies. Lancet. 2017;390(10114):2769–2778. doi:10.1016/S0140-6736(17)32448-0
3. Quaresma AB, Damiao AOMC, Coy CSR, et al. Temporal trends in the epidemiology of inflammatory bowel diseases in the public healthcare system in Brazil: a large population-based study. Lancet Reg Health Am. 2022;9(13):100298. doi:10.1016/j.lana.2022.100298
4. Jiang K, Chen B, Lou D, et al. Systematic review and meta-analysis: association between obesity/overweight and surgical complications in IBD. Int J Colorectal Dis. 2022;37(7):1485–1496. doi:10.1007/s00384-022-04190-y
5. Jain A, Nguyen NH, Proudfoot JA, et al. Impact of obesity on disease activity and patient-reported outcomes measurement information system (PROMIS) in inflammatory bowel diseases. Am J Gastroenterol. 2019;114(4):630–639. doi:10.14309/ajg.0000000000000197
6. Seminerio JL, Koutroubakis IE, Ramos-Rivers C, et al. Impact of obesity on the management and clinical course of patients with inflammatory bowel disease. impact of obesity on the management and clinical course of patients with inflammatory bowel disease. Inflamm Bowel Dis. 2015;21(12):2857–2863. doi:10.1097/MIB.0000000000000560
7. Pringle PL, Stewart KO, Peloquin JM, et al. Body mass index, genetic susceptibility, and risk of complications among individuals with Crohn’s disease. Inflamm Bowel Dis. 2015;21(10):2304–2310. doi:10.1097/MIB.0000000000000498
8. Singh S, Dulai PS, Zarrinpar A, Ramamoorthy S, Sandborn WJ. Obesity in IBD: epidemiology, pathogenesis, disease course and treatment outcomes. Nat Rev Gastroenterol Hepatol. 2017;14(2):110–121. doi:10.1038/nrgastro.2016.181
9. Khakoo NS, Ioannou S, Khakoo NS, Vedantam S, Pearlman M. Impact of obesity on inflammatory bowel disease. Curr Gastroenterol Rep. 2022;24(1):26–36. doi:10.1007/s11894-022-00840-x
10. Rajabnia M, Hajimirzaei SM, Hatamnejad MR, et al. Obesity, a challenge in the management of inflammatory bowel diseases. Immunol Res. 2022;70(6):742–751. doi:10.1007/s12026-022-09315-7
11. Michalak A, Kasztelan-Szczerbińska B, Cichoż-Lach H. Impact of obesity on the course of management of inflammatory bowel disease-a review. Nutrients. 2022;14(19):3983. doi:10.3390/nu14193983
12. Swanson SM, Harper J, Zisman TL. Obesity and inflammatory bowel disease: diagnostic and therapeutic implications. Curr Opin Gastroenterol. 2018;34(2):112–119. doi:10.1097/MOG.0000000000000422
13. Lipcsey M, Stein DJ, DeVore ZG, Feuerstein JD. Rising rate of obesity in patients admitted for crohn’s disease increases costs but not mortality. J Clin Gastroenterol. 2021;55(8):716–720. doi:10.1097/MCG.0000000000001421
14. Johnson AM, Harmsen WS, Aniwan S, et al. Prevalence and impact of obesity in a population-based cohort of patients with crohn’s disease. J Clin Gastroenterol. 2022;30:10–1097. doi:10.1097/MCG.0000000000001821
15. Jarmakiewicz-Czaja S, Sokal A, Filip R. What was first, obesity or inflammatory bowel disease? What does the gut microbiota have to do with it? Nutrients. 2020;12(10):3073. doi:10.3390/nu12103073
16. Blain A, Cattan S, Beaugerie L, Carbonnel F, Gendre JP, Cosnes J. Crohn’s disease clinical course and severity in obese patients. Clin Nutr. 2002;21(1):51–57. doi:10.1054/clnu.2001.0503
17. Nascimento AT, Rocha R, Coqueiro FG, Santana GO, Lyra AC. Does obesity complicate inflammatory bowel diseases? J Crohns Colitis. 2012;6(10):1041. doi:10.1016/j.crohns.2012.06.008
18. Hass DJ, Brensinger CM, Lewis JD, Lichtenstein GR. The impact of increased body mass index on the clinical course of Crohn’s disease. Clin Gastroenterol Hepatol. 2006;4(4):482–488. doi:10.1016/j.cgh.2005.12.015
19. Singla MB, Eickhoff C, Betteridge J. Extraintestinal manifestations are common in obese patients with Crohn’s disease. Inflamm Bowel Dis. 2017;23(9):1637–1642. doi:10.1097/MIB.0000000000001187
20. Nguyen NH, Ohno-Machado L, Sandborn WJ, Singh S. Obesity is independently associated with higher annual burden and costs of hospitalization in patients with inflammatory bowel diseases. Clin Gastroenterol Hepatol. 2019;17(4):709–718.e7. doi:10.1016/j.cgh.2018.07.00
21. Dahiya DS, Kichloo A, Wani F, Singh J, Solanki D, Shaka H. A nationwide analysis on the influence of obesity in inflammatory bowel disease hospitalizations. Intest Res. 2022;20(3):342–349. doi:10.5217/ir.2021.00046
22. Guardado J, Carchman E, Danicic AE, et al. Obesity does not impact perioperative or postoperative outcomes in patients with inflammatory bowel disease. J Gastrointest Surg. 2016;20(4):725–733. doi:10.1007/s11605-015-3060-4
23. Losurdo G, La Fortezza RF, Iannone A, et al. Prevalence and associated factors of obesity in inflammatory bowel disease: a case-control study. World J Gastroenterol. 2020;26(47):7528–7537. doi:10.3748/wjg.v26.i47.7528
24. Kim SK, Lee HS, Kim BJ, et al. The clinical features of inflammatory bowel disease in patients with obesity. Can J Gastroenterol Hepatol. 2021;2021:9981482. doi:10.1155/2021/9981482
25. Gu P, Luo J, Kim J, et al. Effect of obesity on risk of hospitalization, surgery, and serious infection in biologic-treated patients with inflammatory bowel diseases: a CA-IBD cohort study. Am J Gastroenterol. 2022;117(10):1639–1647. doi:10.14309/ajg.0000000000001855
26. Nic Suibhne T, Raftery TC, McMahon O, Walsh C, O’Morain C, O’Sullivan M. High prevalence of overweight and obesity in adults with Crohn’s disease: associations with disease and lifestyle factors. J Crohns Colitis. 2013;7(7):e241–8. doi:10.1016/j.crohns.2012.09.009
27. Flores A, Burstein E, Cipher DJ, Feagins LA. Obesity in inflammatory bowel disease: a marker of less severe disease. Dig Dis Sci. 2015;60(8):2436–2445. doi:10.1007/s10620-015-3629-5
28. Hu Q, Ren J, Li G, Wu X, Li J. The impact of obesity on the clinical course of inflammatory bowel disease: a meta-analysis. Med Sci Monit. 2017;23:2599–2606. doi:10.12659/msm.901969
29. Back IR, Marcon SS, Gaino NM, Vulcano DSB, Dorna MS, Sassaki LY. Body composition in patients with crohn’s disease and ulcerative colitis. Arq Gastroenterol. 2017;54(2):109–114. doi:10.1590/S0004-2803.201700000-02
30. Rocha R, Santana GO, Almeida N, Lyra AC. Analysis of fat and muscle mass in patients with inflammatory bowel disease during remission and active phase. Br J Nutr. 2009;101(5):676–679. doi:10.1017/S0007114508032224
31. Silverberg MS, Satsangi J, Ahmad T, et al. Toward an integrated clinical, molecular and serological classification of inflammatory bowel disease: report of a working party of the 2005 Montreal world congress of gastroenterology. Can J Gastroenterol. 2005;19(Suppl A):5A–36A. doi:10.1155/2005/269076
32. Queiro R, Rodríguez-Caminero S, Riestra S, de Francisco R, Pérez-Martínez I, Ballina J. Performance of two screening questionnaires for inflammatory arthritis in patients with inflammatory bowel disease. Biomed Res Int. 2018;2018:8618703. doi:10.1155/2018/8618703
33. Steed H, Walsh S, Reynolds N. A brief report of the epidemiology of obesity in the inflammatory bowel disease population of Tayside, Scotland. Obes Facts. 2009;2(6):370–372. doi:10.1159/000262276
34. Jura M, Kozak LP. Obesity and related consequences to ageing. Age (Dordr). 2016;38(1):23. doi:10.1007/s11357-016-9884-3
35. Brasil. Instituto Brasileiro de Geografia e Estatística - IBG. Pesquisa nacional de saúde: 2019: Atenção primária à saúde e informações antropométricas [Brazilian Institute of Geography and Statistics - IBG. National health survey: 2019: Primary health care and anthropometric information]. Rio de Janeiro: IBGE; 2020. https://abeso.org.br/wp-content/uploads/2021/07/Pesquisa-Nacional-de-Saude-2019.pdf.
36. Yerushalmy-Feler A, Galai T, Moran-Lev H, et al. BMI in the lower and upper quartiles at diagnosis and at 1-year follow-up is significantly associated with higher risk of disease exacerbation in pediatric inflammatory bowel disease. Eur J Pediatr. 2021;180(1):21–29. doi:10.1007/s00431-020-03697-2
37. Lee YX, Kwan YH, Lim KK, et al. A systematic review of the association of obesity with the outcomes of inflammatory rheumatic diseases. Singapore Med J. 2019;60(6):270–280. doi:10.11622/smedj.2019057
38. Chen CH, Chen HA, Liu CH, Liao HT, Chou CT, Chen CH. Association of obesity with inflammation, disease severity and cardiovascular risk factors among patients with ankylosing spondylitis. Int J Rheum Dis. 2020;23(9):1165–1174. doi:10.1111/1756-185X.13912
39. Liew JW, Huang IJ, Louden DN, Singh N, Gensler LS. Association of body mass index on disease activity in axial spondyloarthritis: systematic review and meta-analysis. RMD Open. 2020;6(1):e001225. doi:10.1136/rmdopen-2020-001225
40. Harper JW, Sinanan MN, Zisman TL. Increased body mass index is associated with earlier time to loss of response to infliximab in patients with inflammatory bowel disease. Inflamm Bowel Dis. 2013;19(10):2118–2124. doi:10.1097/MIB.0b013e31829cf401
41. Kurnool S, Nguyen NH, Proudfoot J, et al. High body mass index is associated with increased risk of treatment failure and surgery in biologic-treated patients with ulcerative colitis. Aliment Pharmacol Ther. 2018;47(11):1472–1479. doi:10.1111/apt.14665
42. Gomes TNF, de Azevedo FS, Argollo M, Miszputen SJ, Ambrogini O. Clinical and demographic profile of inflammatory bowel disease patients in a reference center of São Paulo. Brazil Clin Exp Gastroenterol. 2021;14:91–102. doi:10.2147/CEG.S288688
43. Cury DB, Oliveira R, Cury MS. Inflammatory bowel diseases: time of diagnosis, environmental factors, clinical course, and management - A follow-up study in a private inflammatory bowel disease center (2003–2017) . J Inflamm Res. 2019;12:127–135. doi:10.2147/JIR.S190929
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

