Back to Journals » Patient Preference and Adherence » Volume 10
Body image discrepancy and subjective norm as mediators and moderators of the relationship between body mass index and quality of life
Authors Pétré B, Scheen AJ , Ziegler O, Donneau AF, Dardenne N, Husson E, Albert A, Guillaume M
Received 12 May 2016
Accepted for publication 25 July 2016
Published 4 November 2016 Volume 2016:10 Pages 2261—2270
DOI https://doi.org/10.2147/PPA.S112639
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Benoit Pétré,1 André J Scheen,2 Olivier Ziegler,3 Anne-Françoise Donneau,1 Nadia Dardenne,1 Eddy Husson,1 Adelin Albert,1 Michèle Guillaume1
1Department of Public Health, University of Liège, Liège, Belgium; 2Division of Diabetes, Nutrition and Metabolic Disorders, Department of Medicine, CHU Sart Tilman, University of Liège, Liège, Belgium; 3Department of Diabetes, Metabolic Diseases and Nutrition, Nancy University Hospital, Nancy, France
Background and objective: Despite the strength and consistency of the relationship between body mass index (BMI) and quality of life (QoL), a reduction in BMI does not necessarily lead to an improvement in QoL. Between-subject variability indicates the presence of mediators and moderators in the BMI–QoL association. This study aimed to examine the roles of body image discrepancy (BID) and subjective norm (SN) as potential mediators and moderators.
Subjects and methods: In 2012, 3,016 volunteers (aged ≥18 years) participated in a community-based survey conducted in the French-speaking region of Belgium. Participation was enhanced using a large multimedia campaign (which was supported by a large network of recruiters) that employed the nonstigmatizing slogan, “Whatever your weight, your opinion will count”. Participants were invited to complete a web-based questionnaire on their weight-related experiences. Self-reported measures were used to calculate each participant’s BMI, BID, SN, and QoL (a French obesity-specific QoL questionnaire was used to calculate the participants’ physical dimension of QoL scores [PHY-QoL], psychosocial dimension of QoL scores [PSY/SOC-QoL], and their total scores). The covariates included gender, age, subjective economic status, level of education, household size, and perceived health. The mediation/moderation tests were based on Hayes’ method.
Results: Tests showed that the relationships between BMI and PHY-QoL, PSY/SOC-QoL, and TOT-QoL were partially mediated by BID in both males and females and by SN in females. Moreover, BID was a moderator of the relationship between BMI and PSY/SOC-QoL in males and females. SN was a moderator of the relationship between BMI and PSY/SOC-QoL in males and between BMI and total scores in males (when used without BID in the models).
Conclusion: BID and SN should be considered as important factors in obesity management strategies. The study shows that targeting BMI only is not sufficient to improve the QoL of overweight and obese subjects, and that other variables, including perceptual factors, should be considered.
Keywords: obesity, quality of life, mediators and moderators, body image
Introduction
Overweight and obesity represent a major public health problem, both of which have social and economic implications.1–6 According to the World Health Organization,7 obesity is defined as “abnormal or excessive fat accumulation that may impair health”. One of the major potential consequences of obesity is worsening of quality of life (QoL).8,9 QoL represents a subjective assessment of a large spectrum of life domains.10 Obese people can experience impairments in their daily lives that are specifically linked to obesity and affect their QoL,11,12 resulting in so-called “weight-related quality of life (WR-QoL)”.13
The literature on QoL has been steadily growing over the past few decades.9 Today, it is generally agreed that as body mass index (BMI) increases, the QoL decreases.9,14 In addition, it is well known that individuals who have previously lost weight have difficulty in maintaining their weight loss on a long-term basis.15,16 In this context, researchers like Fontaine and Barofsky argue that obesity management should focus more on monitoring the patient’s health and preventing further ill health, rather than curing their obesity,14 thus supporting the view that new therapeutic targets should aim to improve the QoL of obese individuals.
Despite the strength and consistency of the relationship between BMI and QoL, several studies have shown that a decrease in BMI is not necessarily associated with an improvement in QoL.17,18 Other studies have found between-subjects variability in the relationship between BMI and QoL,19,20 which indicates the existence of mediators and moderators in the BMI–QoL relationship.
Baron and Kenny21 defined mediation as “a hypothesized causal chain in which one variable (X) affects a second variable (M) which, in turn, affects a third variable (Y)”. MacKinnon et al22 stated that “A mediating variable transmits the effect of an independent variable on a dependent variable”. A moderator variable is one that alters the nature of the strength of the relationship between an independent variable and an outcome variable.21 Specifically, when conducting an analysis of moderation, one seeks to determine whether the direction and/or the strength of a causal variable, X, on the outcome variable, Y, depends on another variable, the moderator. Thus, while a mediator variable explains the relationship between two other variables, a moderator influences the direction and/or strength of the relationship between two other variables.22 Contemporary methodologists assert that an analysis that focuses only on moderation or mediation is incomplete; combining mediation and moderation analyses is highly recommended.23,24
Identifying the mediators and moderators of the BMI–QoL relationship represents a major public health challenge, which may lead to new interventions for the management of the health of overweight and obese individuals.24 The goal is to improve their QoL without necessarily or specifically changing their BMI.
This study focused on body image (BI), a multidimensional construct that includes a self-perception component and feedback from other people’s perceptions of oneself.25 A large proportion of overweight and obese people underestimate their weight and believe themselves to be healthier than they actually are.26,27 This distortion regarding body weight perception is known as body image discrepancy (BID).28 Herman et al29 reported that objectively overweight adults who perceived themselves as overweight had poorer self-assessed health and lower general life satisfaction. As obesity levels continue to rise, it is paradoxical that weight control and thinness are regarded by the society as gold standards, which results in weight standards that are difficult to achieve or unrealistic.30,31
In this context, a subjective norm (SN) which is the perceived social pressure to engage or not with a behavior, can become salient. The effect of SN is influenced by the importance each individual places on their appearance in the eyes of others; this can increase when others stigmatize overweight and obese people, which can strengthen the discrepancy between a person’s desire and their actual body weight.32 This distortion is hypothesized to cause psychosocial stress, which can affect QoL.31 It also suggests that BID and SN, two components of BI, may mediate or moderate the relationship between BMI and QoL.
This study examines the role of BID and SN in the mediation/moderation of the relationship between BMI and QoL.
Materials and methods
Study design
A survey was conducted in Wallonia in Belgium as part of a larger project known as EDUDORA2 (which, translated from French, is the abbreviation of “therapeutic and preventive education against diabetes and obesity in adolescence and adulthood”).33 This project focused on therapeutic patient education regarding two metabolic disorders: diabetes and obesity. In particular, EDUDORA2 aimed to 1) improve the quality of diabetes and obesity prevention programs for adolescents and adults using a multidisciplinary approach focused on therapeutic patient education and 2) synergistically involve primary and secondary health care professionals.
A sustained multimedia campaign was organized to recruit participants.34 Information folders and leaflets were prepared and a large network of recruiters that promoted the survey was involved. The promotion of the survey was based on the nonstigmatizing slogan, “Whatever your weight, your opinion will count”. Volunteers were invited to complete a web-based questionnaire involving 31 items, which covered the following topics: demographic, socioeconomic, and anthropometric characteristics, QoL, obesity-related life experiences, expectations about weight management, and other psychosocial issues related to obesity.
The ethics committee of the University Hospital of Liège (Comité d’Ethique Hospitalo-Universitaire de Liège, Belgium) determined this study was exempt from review and did not oppose the undertaking of the study; and as the collected data were anonymous they did not require that written informed consent be obtained. Patient consent was assumed in view of the voluntary participation of the respondents and the lack of any pressure to participate. Methods to avoid stigmatization were taken into account as described in a previous paper.34
Sample
A community-based sample of 4,155 adults (≥18 years) was recruited, covering a wide range of BMI values, including respondents of normal weight. Of the 4,155 subjects who responded to the web-based questionnaire, 3,016 (72.6%) were eligible to be included in the study based on the completeness of their responses.
Measures
Body mass index
Height and weight were self-reported. BMI was calculated as weight/height2 expressed in kg/m2. BMI was categorized as follows: normal weight (19.5≤ BMI <25), overweight (25≤ BMI <30), obese class I (30≤ BMI <35), obese class II (35≤ BMI <40), and obese class III (BMI ≥40).
Body image discrepancy
BID assesses an individual’s visual estimation of their BMI. Participants were shown a series of nine Stunkard body figures35 (1 presenting the smallest BMI and 9 representing the largest BMI) and they were asked to select the figure that most closely resembled their body size. Data from a study by Bulik et al36 were used to link a mean BMI to each Stunkard figure. BID was then calculated using the following formula: BID = self-reported BMI – mean BMI for the selected figure.
Subjective norm
SN is the perceived social pressure to engage or not to engage with a behavior, which is influenced by the importance each individual places on their appearance in the eyes of others. SN was calculated by asking the participants to respond to four statements using a four-point Likert scale (with 1 representing total disagreement with the statement and 4 representing total agreement) regarding the following domains: 1) the importance they place on physical appearance compared with others, 2) what health professionals think of them, 3) what relatives think of them, and 4) what people, in general, think of them (eg, “I attach great importance to what others think of me”). A total score was calculated (range: 4–16 points), and the higher the score, the more importance they placed on their appearance in the “eyes of others”.
Quality of life
QoL was assessed using a simplified version of the French obesity-specific QoL questionnaire developed by Ziegler et al.37 Each participant was asked to evaluate 14 statements about their life on a 4-point Likert scale (with 1 representing total disagreement and 4 representing total agreement). The 14 statements (eg, “Because of my weight, I have trouble to dress or undress”) were equally divided between physical aspects of life and psychosocial aspects of life. A French obesity-specific QoL questionnaire was used to calculate the participants’ physical dimension of QoL scores (PHY-QoL) and psychosocial dimension of QoL scores (PSY/SOC-QoL) by summing the points for each relevant item (range: 7–28 points). The total score (ie, TOT-QoL) was also calculated (range: 14–56 points). The higher the scores, the better the QoL.
Covariates
The demographic and socioeconomic characteristics were: gender, age (years), subjective economic status (low or high), level of education (primary, secondary, or tertiary), household size (1 or >1), and perceived health (good or bad).
Analysis
The quantitative variables were summarized using medians and interquartile ranges. Nonparametric Kruskal–Wallis test was used to compare the values between subgroups. Normality was assessed using the Shapiro–Wilk test.
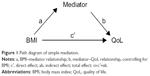
The mediation effect was tested using the product of coefficients approach.23 As shown in Figure 1, the total effect of BMI on QoL was decomposed into direct and indirect (mediated) effects. The indirect effect was calculated as the product of two estimated regression coefficients,  A bootstrapping method was used to test the hypotheses about mediation effects due to the skewness of the sampling distribution of the indirect effect.38 A statistically significant indirect effect implies the presence of mediation. There is “partial mediation” when the direct effect is statistically significantly different from zero and “complete mediation” if it is not. The completely standardized indirect effect was used to measure the effect size of mediation.39
A bootstrapping method was used to test the hypotheses about mediation effects due to the skewness of the sampling distribution of the indirect effect.38 A statistically significant indirect effect implies the presence of mediation. There is “partial mediation” when the direct effect is statistically significantly different from zero and “complete mediation” if it is not. The completely standardized indirect effect was used to measure the effect size of mediation.39
The moderation effect (Figure 2) was assessed using the following regression equation:
|
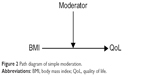  | Figure 2 Path diagram of simple moderation. |
When there was a statistically significant interaction effect, â3, the conditional effect of BMI on QoL was calculated at different values of the moderator (typically low, moderate, and high values).
All the modeling analyses were adjusted for the demographic and socioeconomic covariates. As recommended in the literature,20,32 the mediation and moderation effects were tested separately for men and women. Results were considered statistically significant at the 5% critical level (P<0.05). The statistical analyses were carried out using SAS software (version 9.4 for Windows) (SAS Institute Inc., Cary, NC, USA), and the mediation and moderation analyses were performed using the SAS PROCESS macro.23
Results
The study enrolled 3,016 eligible subjects (944 [31.3%] men and 2,072 [68.7%] women) with a mean age of 46.2±13.3 years. According to their BMIs, the subjects were classified as follows: 341 (11.3%) were of normal weight, 932 (30.9%) were overweight, 940 (31.2%) were in obese class I, 454 (15.1%) were in obese class II, and 349 (11.6%) were in obese class III.
The distribution of variables used in the model of mediation is shown in Table 1, according to demographic and socioeconomic characteristics.
QoL was generally higher for men compared to women (P<0.0001), while BMI was better estimated in women (P=0.0006). Women placed more importance on their appearance in the eyes of others than men (P<0.0001). PHY-QoL decreased with age, but PSY/SOC-QoL was better in the age group of >40 years. The emphasis on the importance of an individual’s appearance in the eyes of others decreased from 55 years of age, and the underestimation of BI was higher in the >40 years age group. Those who perceived their economic status as difficult and their health as bad had worse values regarding all of the following variables (P<0.0001): higher BMI, more importance placed on their appearance in the eyes of others, higher underestimation of BI, and worse QoL. Similar results were found for those with lower levels of education, except for the effect on SN, which was not significantly different between the different levels of education. Household size positively affected QoL (P=0.04 for PHY-QoL and P<0.0001 for both PSY/SOC-QoL and TOT-QoL).
The findings of the mediation analysis are shown in Table 2. BMI was negatively associated with PHY-QoL, PSY/SOC-QoL, and TOT-QoL in both men and women (P<0.0001). Statistically significant indirect effects were observed for SN for PHY-QoL, PSY/SOC-QoL, and TOT-QoL only in women, indicating the role of SN as a mediator in the relationship between BMI and QoL. The indirect effects of BMI on PHY-QoL, PSY/SOC-QoL, and TOT-QoL were statistically significant for both males and females. These results remained consistent when BID and SN were both used in the models. The mediation effects were found to be partial effects because the direct effect of BMI on QoL remained statistically significantly different from zero. Effect size testing showed very low values, indicating that the actual associations were weak despite being statistically significant.
  | Table 2 Mediation effects of BID and SN on BMI–QoL relationship by gender and after adjustment for covariates |
The findings of the moderation analysis are shown in Table 3. Based on the results of the interactions between the coefficients, BID and SN, when considered together or separately, were found to be moderators of the relationship between BMI and PSY/SOC-QoL, except for SN in women when considered separately. The association between BMI and QoL was higher when the values of BID or SN increased, indicating that a greater underestimation of BMI and a greater importance placed on an individual’s appearance in the eyes of others enhanced the strength of the association between higher BMI and lower PSY/SOC-QoL. When used in the model separately, SN was also a moderator of the relationship between BMI and TOT-QoL, but only in men. The R2 values varied between 0.23 and 0.45.
Discussion
This study aimed to investigate whether BID and SN are mediators and/or moderators of the BMI–QoL relationship, while taking into account the gender differences. The mediation/moderation tests based on Hayes’ method showed that the relationships between BMI and PHY-QoL, PSY/SOC-QoL, and TOT-QoL were partially mediated by BID in both males and females and by SN in females. Moreover, BID and SN played the role of moderators between BMI and PSY/SOC-QoL in males and females (except for SN in women when considered separately), and SN was also a moderator of the relationship between BMI and TOT-QoL in males (when used without BID in the models).
Next, the findings related to the demographic and socioeconomic factors are discussed and subsequently, the results of the mediation and moderation tests are discussed along with the relative prospects.
The variables studied, except for PHY-QoL, were shown to increase with age. As obese subjects get older, they become more comfortable with their BI and SN, the importance of their appearance in the eyes of others becomes smaller, and their PSY/SOC-QoL also improves. Seidell et al40 showed that the association between BMI and subjective health was much more pronounced at younger ages. In contrast, increasing age was associated with deterioration in PHY-QoL, which may be explained by the double burden on the participants’ musculoskeletal systems, namely, aging and their potentially more extensive experience living with obesity.
Women seem to be more affected by the perception of their weight than men. The tendency of women to be more concerned about weight-related issues is well known. It was confirmed in this study by the greater importance attached to their appearance in the eyes of others and their worse PSY/SOC-QoL. Moreover, women were more accurate than men in identifying the correct Stunkard figure for their BMI, as supported by other studies.41,42 Befort and Rickard43 found that women are more influenced by all types of feedback than men, because they tend to look for evidence of their competence. Moreover, women, in particular, seem to be more preoccupied with their physical appearance and to focus on the current beauty ideals, which can lead to body weight dissatisfaction and excessive attention paid to BI.44–46
The results confirm the results of previous studies that have highlighted the role of social support in buffering obesity-related impairments in WR-QoL47,48 as well as the role of socioeconomic status which had been demonstrated shown to have a strong negative impact on QoL, especially in obese individuals.49,50 Perceived health was also negatively associated with all the outcome variables. The median BMI was 4 kg/m2 higher for those who perceived their health to be good, which may explain the influence of perceived health on the other outcome variables. However, based on the descriptive results, it is difficult to come to any conclusion about the effect of perceived health on the other outcome variables: differences between the groups which perceived their health to be good and those which perceived their health to be bad could be attributed to the difference in BMI or to the perceived health variable itself or to the other variables that are associated with the perceived health variable.
Nevertheless, overall, the descriptive results discussed above indicate the need to take into consideration demographic and socioeconomic variables as control factors when studying mediation/moderation effects, as followed in a previous study.51
It was hypothesized that BID and/or SN were mediators and/or moderators of the relationship between BMI and QoL, and, if they were, this could lead to new therapeutic strategies that target QoL rather than BMI. BID was found to be a partial mediator of the relationship between BMI and PHY-QoL, PSY/SOC-QoL, and TOT-QoL and a moderator of the relationship between BMI and PSY/SOC-QoL in both genders. This dual effect of BID is of major importance as it better explains the role of BID as a novel determinant in the obesity epidemic.52
The mediation effect of BID may be interpreted as follows: to preserve their QoL, individuals tend to underestimate their BMI as a psychological protective mechanism, which is consistent with the results obtained by Hayward et al.20 The moderator effect is more difficult to interpret as, for people who markedly underestimate their BMI, the link between a higher BMI and a lower QoL seems to be stronger. Part of the interpretation of the results could involve the tendency for most obese people, and particularly very obese people, to be in denial about their weight,53 that is, they refuse to see themselves as obese and, therefore, fail to identify the correct Stunkard figure. In addition, in a previous study, the authors postulated that males may see themselves as “big and strong” rather than “fat” and this viewpoint may protect them from BI dissatisfaction.54 However, if obese people try to maintain a positive BI of themselves, QoL does not follow the same way. The results concerning BID strengthen the evidence regarding the need to develop new weight management indicators to help develop new therapeutic approaches. For example, dance therapy would be especially suitable for improving body perception.55
Based on the results, SN is a partial mediator of the relationships between BMI and PHY-QoL, PSY/SOC-QoL, and TOT-QoL in women and a moderator of the relationship between BMI and both PSY/SOC-QoL and TOT-QoL in men. BMI causally influences SN in women. A previous study demonstrated how women adhere to the SN that involves placing a great deal of importance on thinness.45 Therefore, it can be hypothesized that, in order to protect their QoL, people tend to give less importance to the eyes of others until SN plays a mediation role between BMI and QoL. The role of SN is not so large for men, and SN only acts as a moderator: in men who place a large importance on SN, the link between a higher BMI and a lower QoL is stronger, which indicates that men are not indifferent to the eyes of others.
Testing BID and SN together confirms their roles in the BMI–QoL relationship and strengthens the evidence regarding the importance of using multiple weight management indicators. The results also show that the relationship between BMI and PSY/SOC-QoL is more affected by the variables studied than the relationship between BMI and PHYS-QoL, which can be explained by the psychosocial nature of BID and SN.
Interpreting mediation and moderation effects is challenging because they must be supported by theory.56 Further research is needed to explain the results of this study. Qualitative studies could be used to gain an understanding of patients’ experiences and perspectives, and analysis by BMI categories would be useful to provide detailed explanations according to the patient’s BMI.
The results of this study should be put into perspective with those of other studies that explored the mediating or moderating variables in the relationship between BMI and QoL. Vilhena et al51 explored the mediating role of stigma on the relationship between positive/negative affect and QoL in obese patients in Portugal. Cox et al19 showed how BI dissatisfaction helped WR-QoL in 149 black women in the US. These results emphasize the consideration of individuals’ everyday experiences of their obesity and how these experiences affect their QoL. Further studies are needed to understand what enables individuals to better preserve their QoL and mental health, and to determine the most appropriate treatments and management strategies.
Several public health and clinical implications arise from these studies. This study results reflect the model of health determinants and their complex interactions, a system in which psychosocial factors have a special place.57 Health care providers require training to encourage them to develop accurate attitude about BI satisfaction in obese patients.
This study has several limitations. The survey involved voluntary participation; so, the sample is not necessarily representative of the target population. However, the participants were not seeking weight loss treatment (as is often the case in studies on obesity and QoL), which means that the results are more likely to be generalizable. The study was cross sectional in nature, and confirmation of the mediating/moderating effects would require longitudinal studies and experimental designs to better interpret the influences between the variables.21 The coefficient of determination, R2, showed that the variables under study poorly predicted QoL (the highest R2 was 0.45), indicating that other covariates are needed in future investigations. BMI was self-reported, and thus was only as accurate as the participants’ responses. The number of respondents to the survey allowed a satisfactory distribution of individuals in all the BMI categories for statistical analysis. Most studies on the QoL of obese individuals are based on smaller sample sizes and/or restricted age ranges. However, a large sample can be problematic as cautious interpretation is required, because highly statistically significant results (due to the large sample size) are not necessarily clinically meaningful. Indeed, measurement of effect sizes indicated the weak nature of the effects.
Conclusion
The findings suggest that strategies that target only BMI may not be sufficient to improve the QoL of overweight and obese individuals, and that other variables, including perceptual factors, must be considered in the management of overweight and obesity. More health education is needed to address issues related to overweight, obesity, and body weight perception.
Acknowledgments
This work was supported by the European Regional Development Fund and the Belgian public health authorities.
Disclosure
The authors report no conflicts of interest in this work.
References
James WP, Jackson-Leach R, Mhurchu CN, et al. Comparative quantification of health risks: global and regional burden of disease attribution to selected major risk factors. In: Ezzati M, Lopez AD, Rodgers A, Murray CJL, editors. Overweight and Obesity (high body mass index). Geneva: World Health Organization; 2004:497–596. | ||
Flegal KM, Graubard BI, Williamson DF, Gail MH. Excess deaths associated with underweight, overweight, and obesity. JAMA. 2005;293(15):1861–1867. | ||
Haslam DW, James WP. Obesity. Lancet. 2005;366(9492):1197–1209. | ||
Muller-Riemenschneider F, Reinhold T, Berghofer A, Willich SN. Health-economic burden of obesity in Europe. Eur J Epidemiol. 2008;23(8):499–509. | ||
Arterburn DE, DeLaet DE, Schauer DP. Obesity. BMJ Clin Evid. 2006;15:1–2. | ||
Segula D. Complications of obesity in adults: a short review of the literature. Malawi Med J. 2014;26(1):20–24. | ||
World Health Organization. Obesity: Preventing and Managing the Global Epidemic: Report of a WHO Consultation. Geneva: World Health Organization; 2000. | ||
Taylor VH, Forhan M, Vigod SN, McIntyre RS, Morrison KM. The impact of obesity on quality of life. Best Pract Res Clin Endocrinol Metab. 2013;27(2):139–146. | ||
Kolotkin RL, Meter K, Williams GR. Quality of life and obesity. Obes Rev. 2001;2(4):219–229. | ||
The WHOQOL Group. The World Health Organization Quality of Life Assessment (WHOQOL): Development and psychometric properties. Soc Sci Med. 1998;46(12):1569–1585. | ||
Lewis S, Thomas SL, Hyde J, Castle DJ, Komesaroff PA. A qualitative investigation of obese men’s experiences with their weight. Am J Health Behav. 2011;35(4):458–469. | ||
Furber CM, McGowan L. A qualitative study of the experiences of women who are obese and pregnant in the UK. Midwifery. 2011;27(4):437–444. | ||
Kolotkin RL, Zeller M, Modi AC, et al. Assessing weight-related quality of life in adolescents. Obesity (Silver Spring). 2006;14(3):448–457. | ||
Fontaine KR, Barofsky I. Obesity and health-related quality of life. Obes Rev. 2001;2(3):173–182. | ||
Wing RR, Phelan S. Long-term weight loss maintenance. Am J Clin Nutr. 2005;82(Suppl 1):222S–225S. | ||
Curioni CC, Lourenço PM. Long-term weight loss after diet and exercise: a systematic review. Int J Obes (Lond). 2005;29(10):1168–1174. | ||
Laxy M, Holle R, Döring A, Peters A, Hunger M. The longitudinal association between weight change and health-related quality of life: the KORA S4/F4 cohort study. Int J Public Health. 2014;59(2):279–288. | ||
Döring N, de Munter J, Rasmussen F. The associations between overweight, weight change and health related quality of life: longitudinal data from the Stockholm Public Health Cohort 2002–2010. Prev Med. 2015;75:12–17. | ||
Cox TL, Ard JD, Beasley TM, Fernandez JR, Howard VJ, Affuso O. Body image as a mediator of the relationship between body mass index and weight-related quality of life in black women. J Womens Health. 2011;20(10):1573–1578. | ||
Hayward J, Millar L, Petersen S, Swinburn B, Lewis AJ. When ignorance is bliss: weight perception, body mass index and quality of life in adolescents. Int J Obes (Lond). 2014;38(10):1328–1334. | ||
Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Personal Soc Psychol. 1986;51(6):1173–1182. | ||
MacKinnon DP, Fairchild AJ, Fritz MS. Mediation analysis. Annu Rev Psychol. 2007;58:593–614. | ||
Hayes AF. 2012. PROCESS: A versatile computational tool for observed variable mediation, moderation, and conditional process modeling [White paper]. Available from: http://www.afhayes.com/public/process2012.pdf. Accessed October 3, 2016. | ||
Fairchild AJ, MacKinnon DP. A general model for testing mediation and moderation effects. Prev Sci. 2009;10(2):87–99. | ||
Maruf FA, Akinpelu AO, Nwankwo MJ. Perceived body image and weight: discrepancies and gender differences among University undergraduates. Afr Health Sci. 2012;12(4):464–472. | ||
Wetmore C, Modkdad AH. In denial: misperceptions of weight change among adults in the United States. Prev Med. 2012;55(2):93–100. | ||
Wardle J, Haase AM, Steptoe A. Body image and weight control in young adults: international comparisons in university students from 22 countries. Int J Obes (Lond). 2006;30(4):644–651. | ||
Liechty JM. Body image distortion and three types of weight loss behaviors among nonoverweight girls in the United States. J Adolesc Health. 2010;47(2):176–182. | ||
Herman KM, Hopman WM, Rosenberg MW. Self-rated health and life satisfaction among Canadian adults: associations of perceived weight status versus BMI. Qual Life Res. 2013;22(10):2693–2705. | ||
Lewis S, Thomas SL, Hyde J, Castle DJ, Blood RW, Komesaroff PA. ‘I don’t eat a hamburger and large chips every day!’ a qualitative study of the impact of public health messages about obesity on obese adults. BMC Public Health. 2010;10:309. | ||
Cuypers K, Kvaløy K, Bratberg G, Midthjell K, Holmen J, Holmen TL. Being normal weight but feeling overweight in adolescence may affect weight development into young adulthood – an 11-year followup: the HUNT study, Norway. J Obes. 2012;2012:601872. | ||
Friedman KE, Reichmann SK, Costanzo PR, Musante GJ. Body image partially mediates the relationship between obesity and psychological distress. Obes Res. 2002;10(1):33–41. | ||
Scheen A, Bourguignon JP, Hubermont G, et al. Education therapeutique et preventive face au diabete et a l’obesite a risque chez l’adulte et l’adolescent: le projet Interreg IV EDUDORA2 [Patient education facing diabetes and at risk obesity in adults and teenagers: Interreg IV EDUDORA2 project]. Diabetes Metab. 2010;36(Suppl 1):193. | ||
Pétré B, Donneau A-F, Crutze C, Husson E, Scheen A, Guillaume M. Obese subjects involvement in a population-based survey: the use of information and communication technologies (ICT) to avoid stigmatization. Qual Life Res. 2015;24(5):1131–1135. | ||
Stunkard A, Sùrensen T, Schulsinger F. Use of the Danish Adoption Register for the study of obesity and thinness. In: Kety S, Roland L, Sidman R, Matthysse S, editors. The Genetics of Neurological and Psychiatric Disorders. New York: Raven Press; 1983. | ||
Bulik CM, Wade TD, Heath AC, Martin NG, Stunkard AJ, Eaves LJ. Relating body mass index to figural stimuli: population-based normative data for Caucasians. Int J Obes Relat Metab Disord. 2001;25(10):1517–1524. | ||
Ziegler O, Filipecki J, Girod I, Guillemin F. Development and validation of a French obesity-specific quality of life questionnaire: Quality of Life, Obesity and Dietetics (QOLOD) rating scale. Diabetes Metab. 2005;31(3 Pt 1):273–283. | ||
Preacher KJ, Rucker DD, Hayes AF. Addressing moderated mediation hypotheses: theory, methods, and prescriptions. Multivariate Behav Res. 2007;42(1):185–227. | ||
Fairchild AJ, MacKinnon DP, Taborga MP, Taylor AB. R2 effect-size measures for mediation analysis. Behav Res Methods. 2009;41(2):486–498. | ||
Seidell JC, Bakx KC, Deurenberg P, Burema J, Hautvast JG, Huygen FJ. The relation between overweight and subjective health according to age, social class, slimming behavior and smoking habits in Dutch adults. Am J Public Health. 1986;76(12):1410–1415. | ||
Emslie C, Hunt K, Macintyre S. Perceptions of body image among working men and women. J Epidemiol Community Health. 2001;55(6):406–407. | ||
Madrigal H, Sánchez-Villegas A, Martínez-González MA, et al. Underestimation of body mass index through perceived body image as compared to self-reported body mass index in the European Union. Public Health. 2000;114(6):468–473. | ||
Befort CA, Rickard KM. Gender similarities in response to figure-size feedback in a selected non-clinical population. Sex Roles. 2003;49(1):71–80. | ||
Stunkard AJ, Sobal J. Psychosocial consequences of obesity. In: Brownell KD, Fairburn C, editors. Eating Disorders and Obesity: A Comprehensive Handbook. New York: Guilford Press; 1995. | ||
Katzmarzyk PT, Davis C. Thinness and body shape of Play-boy centerfolds from 1978 to 1998. Int J Obes Relat Metab Disord. 2001;25(4):590–592. | ||
Kiefer I, Leitner B, Bauer R, Rieder A. Body weight: the male and female perception. Sozial-und Präventivmedizin. 2000;45(6):274–278. | ||
Wiczinski E, Döring A, John J, von Lengerke T; KORA Study Group. Obesity and health-related quality of life: does social support moderate existing associations? Br J Health Psychol. 2009;14(Pt 4):717–734. | ||
Herzer M, Zeller MH, Rausch JR, Modi AC. Perceived social support and its association with obesity-specific health-related quality of life. J Dev Behav Pediatr. 2011;32(3):188–195. | ||
Minet Kinge J, Morris S. Socioeconomic variation in the impact of obesity on health-related quality of life. Soc Sci Med. 2010;71(10):1864–1871. | ||
Burkert NT, Rásky É, Großschädl F, Muckenhuber J, Freidl W. The influence of socioeconomic factors on health parameters in overweight and obese adults. PLoS One. 2013;8(6):e65407. | ||
Vilhena E, Cardoso H, Silva I, Pais-Ribeiro J, Mendonça D. Predictors of quality of life in portuguese obese patients: a structural equation modeling application. J Obes. 2014;2014:684919. | ||
Powell TM, de Lemos JA, Banks K, et al. Body size misperception: a novel determinant in the obesity epidemic. Arch Intern Med. 2010;170(18):1695–1697. | ||
Lykouras L. Psychological profile of obese patients. Dig Dis. 2008;26(1):36–39. | ||
Schwartz MB, Brownell KD. Obesity and body image. Body Image. 2004;1(1):43–56. | ||
Muller-Pinget S, Carrard I, Ybarra J, Golay A. Dance therapy improves self-body image among obese patients. Patient Educ Couns. 2012;89(3):525–528. | ||
Andersson U, Cuervo-Cazurra A, Nielsen BB. From the editors: explaining interaction effects within and across levles of analysis. J Int Bus Stud. 2014;45(9):1063–1071. | ||
Government Office for Science and Department of Health. Tackling obesities: future choices – 1 year review; 2012. Available from: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/288000/08-1565-tackling-obesities-future-choices-1-year-review.pdf. Accessed April 17, 2016. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.