Back to Journals » Integrated Blood Pressure Control » Volume 14
Blood Pressure Control with Reference to Intensive Blood Pressure Targets Among Hypertension Patients on Chronic Follow-Up at Dessie Referral Hospital, Northeast Ethiopia
Received 22 October 2020
Accepted for publication 14 December 2020
Published 22 January 2021 Volume 2021:14 Pages 1—7
DOI https://doi.org/10.2147/IBPC.S268186
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Konstantinos Tziomalos
Kassahun Bogale,1 Assasu Aderaw2
1Clinical Pharmacy Unit, Department of Pharmacy, College of Medicine and Health Sciences, Wollo University, Dessie, Ethiopia; 2Department of Pharmacy, Wollo University, Dessie, Ethiopia
Correspondence: Kassahun Bogale
Clinical Pharmacy Unit, Department of Pharmacy, College of Medicine and Health Sciences, Wollo University, PO Box: 1145, Dessie, Ethiopia
Tel +251-913290505
Fax +251-331190586
Email [email protected]
Background: Hypertension is a risk factor for heart, brain, kidney, and other diseases. It is also the major cause of premature death. Thus, it is important to prevent, treat, and control hypertension and to reduce the risk of cardiovascular disease.
Objective: To determine the level of blood pressure control and associated factors based on the new intensive blood pressure goals (< 130/80 mmHg).
Methods: A cross-sectional study design was used to assess the level of blood pressure control and associated factors from February 15 to April 15, 2019. Two hundred and sixteen patients were selected through a systematic sampling technique.
Results: From 203 hypertension patients incorporated in the study, 102 (50.2%) were females. The mean age of patients documented during the last date of follow-up was 55.2 (SD=± 14.47). About 51.2% of patients were less than 5 years from the day of diagnosis of hypertension. The majority of the study participants (111, 54.7%) were using two antihypertensives. The most common anti-hypertensive medication was hydrochlorothiazide (HCT), at 25 (12.3%). The most common combination drug therapy used was the combination of HCT and calcium channel blockers, at 62 (30.5%). Heart failure (22, 20.8%), stroke (18, 16.98%), and dyslipidemia (17, 16.04%) were the top three comorbidities. Based on the new intensive targets of blood pressure control (< 130/80 mmHg), the blood pressure was controlled for only 25 (12%) patients.
Conclusion: The level of blood pressure control for hypertensive patients on chronic follow-up at Dessie Referral Hospital was very poor.
Keywords: blood pressure control, Dessie Referral Hospital, hypertension
Background
Cardiovascular disease (CVD) is responsible for the death of 17.3 million people annually and it is expected to increase to greater than 23.6 million by 2030.1
In 2015, 1.13 billion peoples were affected by hypertension globally. It is more common with higher age, with a prevalence of greater than 60%. This higher prevalence of hypertension is consistent across different parts of the world irrespective of income status.2 In Ethiopia, the prevalence of hypertension was nearly 19.6% in 2015, which is higher in the urban (23.7%) than rural population (14.7%). The prevalence among males (20.6%) and females (19.2%) was relatively similar.3
The 2017 American College of Cardiology/American Heart Association guidelines recommend intensive systolic blood pressure (BP) targets (<120 mmHg) for most patients which was based on evidences from the Systolic BP Intervention Trial (SPRINT). The trial concluded that a primary composite outcome of cardiovascular disease risk and death was reduced by 25% in the intensive treatment group compared with the standard treatment group. Similarly, all-cause mortality was reduced by 27% in the intensive treatment group.4
It is known that there is a graded association between higher blood pressure and increased CVD risk. In a meta-analysis of 61 prospective studies, the risk of CVD increased in a log-linear fashion as Systolic BP levels increased from <115 mmHg to >180 mmHg and Diastolic BP levels from <75 mmHg to >105 mmHg.5
Worldwide, hypertension is not adequately controlled, and it is worse in lower-income countries. In 2010, control of hypertension (defined as <140/<90 mmHg) was estimated to be 28% in high-income and 8% in middle- and low-income countries.6
Hypertension control is a complex issue. To achieve an optimal blood pressure control it needs active cooperation between healthcare providers, patients, and healthcare systems. Hence this study aims to determine the level of blood pressure control and associated factors in a hypertension clinic of Dessie Referral Hospital (DRH), Dessie town, North-East Ethiopia.
Methods
Study Setting and Period
The study was conducted at the hypertension clinic of DRH, Dessie town from February 15 to April 15, 2019. DRH is a referral hospital with 560 beds. Dessie is the capital city of South Wollo zone, Amhara region, which is 401 km from the capital city of the country, Addis Ababa.
Study Design
A hospital-based cross-sectional study design was employed.
Population
All adult hypertension patients on chronic follow-up at Dessie Referral Hospital were taken as a source population.
Selection Criteria
After explaining the purpose of the study and informed consent, hypertension patients ≥18 years who visited the hypertension clinic of DRH during the study period were included in the study after confirmation of being on antihypertensive drug treatment for at least 6 months. Pregnant women and patients with poor cognitive functions were excluded.
BP Measurement
BP (on the day of the visit) was measured using a standard mercury sphygmomanometer of an appropriate size cuff twice with an interval of 2 minutes after resting for at least 5–10 minutes. The mean of two BP readings was calculated and recorded.
Sample Size Determination and Sampling Techniques
The sample size for the study was determined using single population proportion formula. A similar study was done at Gondar Hospital with the prevalence of blood pressure control nearly 45%.7 Hence a P-value of 0.45 and confidence interval 90%, α=0.1, and Margin of error/degree of accuracy=5% was used for sample size calculation. Based on this the calculated sample size was 266. The total population of patients on follow-up at DRH were 750. Using the correction formula, the final sample size was found to be 216. When we divide the total population (750) with the final sample size (216) we can get the sampling interval which is nearly three. Hence patients were selected using systematic sampling method with a sampling interval of three. The first patient was selected based on lottery method. At the first day of data collection 20 patients were appointed. Hence with lottery method the fourth patient was the first to be incorporated into the study.
Data Collection Tool
A structured data abstraction format was prepared and used to collect data from patients as well as patient’s medical record chart. A pilot study was done on 10% of the sample size on Boru-Meda General Hospital located at the same city before the actual data collection was done.
Data Analysis
After collection, data was entered to EPI-info 3.5.4 software and exported to SPSS version 20.0 for analysis. Both binary and multivariable logistic regressions models were used to identify factors affecting BP control. Statistical significance was measured with P-values less than 0.05 at 95% confidence interval.
Result
Socio-Demographic Characteristics
From the total of 216 hypertensive patients included in the study, 13 patient medical records were incomplete, hence excluded from the study. From 203 hypertensive patients incorporated in the study, 102 (50.2%) were females. The mean age of patients documented during the last date of visit was 55.2 (SD=±14.47) years, ranging from 20– 85 years. The majority (52, 25.6%) of patients were in the age group 50–59 years. Most (91, 44.8%) patients were found to be illiterate. With regard to their occupation, merchants predominate (72, 35.5%); 54.7% of patients came from rural areas (Table 1).
 |
Table 1 Socio-Demographic Characteristics of Hypertension Patients at Dessie Referral Hospital, Ethiopia, 2019 |
Lifestyle of Patients
All study participants were asked about their lifestyle, which may affect the level of blood pressure control. Based on this, 97 (47.8%) respondents use salt in their food. The majority of patients have no history of cigarette smoking or chronic alcohol use, (196, 96.6% and 190, 93.6%, respectively). When patients were asked about the use of hot drinks such as coffee and tea, 136 (67%) use during certain holidays only. Only 41 (20.2%) respondents were doing regular exercise. Except two patients all hypertensive patients participating in this study did not use traditional medicines (Table 2). The mean duration of patients diagnosed with hypertension was 5.2 (±4.27) years, with the range of 6 month, to 30 years. The majority of patients (170, 83.7) did not have a BP measuring device at their home and they were measured at hospital during medication refill time. With regard to the number of anti-hypertensives used to control blood pressure, the majority of the study participants (111, 54.7%) were using two antihypertensives. The use of three combinations was found to be 34 (16.7%) and monotherapy was used by 58 (28.6%) hypertensive patients. The use of more than three drug combinations was not documented (Table 2).
 |
Table 2 Lifestyle of Hypertension Patients Attending Medical OPD of Dessie Referral Hospital, Dessie, Ethiopia, 2019 |
Number and Type of Anti-Hypertensives
The most common class of anti-hypertensive medication was a diuretic hydrochlorothiazide (HCT) (25, 12.3%) followed by calcium channel blockers (12, 5.9%), and angiotensin converting enzyme inhibitors (ACEI) (18, 8.9%). The most common combination drug therapy used was found to be the combination of HCT and CCBs 62 (30.5%), which is followed by HCT+ACEI (12.3%), and HCT+CCB+ACEI (7.9%) (Table 3).
 |
Table 3 Type of Anti-Hypertensives Drugs Used by Hypertension Patients Attending Medical OPD of Dessie Referral Hospital, Dessie, Ethiopia, 2019 |
Comorbidities
From 203 study participants, 106 (52.2%) have comorbidities. Heart Failure (22, 20.8%), Stroke (18, 16.98%), and Dyslipidemia (17, 16.04%) are the top three diseases occurring in hypertensive patients (Table 4).
 |
Table 4 Comorbidities Diagnosed on Hypertensive Patients Attending Chronic OPD of Dessie Referral Hospital, Dessie, Ethiopia, 2019 |
Laboratory Investigations
The average total cholesterol, LDL cholesterol, HDL cholesterol, and triglyceride levels were found to be 200.74±46.4, ranging from 112–309 mg/dL, 140.86±63.7, ranging from 67–404 mg/dL, 35.83±9, ranging from 18–56 mg/dL, and 16.7±88.9, ranging from 44–410 mg/dL. As shown in the table, 50% of patients whose total cholesterol level measured has elevated level (>200 mg/dL) of total cholesterol. From the total of 30 patients, 72.4% have elevated level of LDL cholesterol. From the total of 64 patients who have documented liver function test, almost all have normal level of ALT and AST levels. From the total of 203 patients (137, 67.5%) have documented renal function tests. The mean Scr level was 0.899±0.28 ranging from 0.1 up to 1.5 mg/dL (Table 5).
 |
Table 5 Latest Laboratory Investigations Done for Hypertension Patients Attending Medical OPD of Dessie Referral Hospital, Dessie, Ethiopia, 2019 |
Blood Pressure Control
The mean systolic blood pressure and diastolic blood pressure documented during the day of visit was 133.07±16.9 mmHg (ranging from 90–190 mmHg) and 85.09±10.6 mmHg (ranging from 60–110 mmHg).
Based on the new intensive targets of blood pressure control (≤130/80 mmHg) recommended by AHA/ACC only (25, 12.3%) patients have controlled blood pressure. The rest (87.7%) of the patients have suboptimal blood pressure. The blood pressure control based on JNC 7 guidelines (≤140/90 mmHg) was found to be 43.8% (Figure 1).
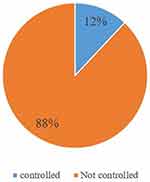 |
Figure 1 The level of blood pressure control for hypertension patients attending medical OPD of Dessie Referral Hospital, Dessie, Ethiopia, 2019. |
When the blood pressure targets were compared against the previous recommendations (<140/90 mmHg) the level of blood pressure control is slightly higher (12.3% vs 43.8%) (Figure 2).
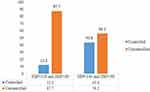 |
Figure 2 The level of blood pressure control <130/80 mmHg vs <140/90 mmHg for hypertension patients attending outpatient department of Dessie Referral Hospital, Dessie, Ethiopia, 2019. |
Factors Affecting Blood Pressure Control
From the bivariate analysis age, marital status, use of salt in food was having significant association with P≤0.05. But on multivariate analysis all the factors mentioned does not have significant association.
Discussion
From the total of 203 study participants, 102 (50.2%) were females. It was similar with that of a study done at Zewditu Memorial hospital in Addis Ababa (55.6%).8 The same study was done in Gondar which reported that 61.9% of patients were females.9 The mean age of patients in this study was found to be 55.2 which is almost similar with that of a study done in Gondar (57 years).10
Heart failure, stroke, and dyslipidemia were found to be the top three comorbid conditions documented at Dessie Referral Hospital; 20.75%, 16.98%, and 16.04%, respectively. In a study done in Jordan, diabetes mellitus was the leading followed by dyslipidemia and coronary artery disease.11 A similar study done in Kenya mentioned that 41.85% of patients have DM as a comorbid condition.12 These differences were observed since DM patients with hypertension were followed separately at the diabetic clinic.
The mean duration after the diagnosis of hypertension in this study was found to be 5.2 (±4.27) years. Similarly, since the start of drug therapy, patients were treated on average for 8.22±7.07 years (range=0.5–39) in a similar study done in Gondar.8 The duration was 11.27±8.34 at Zewditu Memorial hospital according to the study done in 2016.13
The majority of patients (33.7%) participated in a study done on four health centers in New York used a single drug to control their blood pressure as compared to the present study which showed that 54.7% of the study participants were on two drugs.14 A similar finding like the present one was observed on a study done at six public primary care clinics in Malaysia (46.7% were on dual therapy).15 From the class of anti-hypertensives used, the diuretic, HCT was the most common (12.3%) followed by calcium channel blockers and ACE inhibitors. The same is true for HCT but ACE inhibitors slightly higher than CCBs (8.1% vs 5.52%) according to a study done by Tadesse et al16 in Gondar hospital. In a study done in Cameroon, Yaounde beta-blockers are the second next to diuretics.17 A combination of HCT and CCBs was the most common. But this combination is not the preferred one since most guidelines recommend the combination of HCT and ACEIs.
According to the recommendation by ACC/AHA intensive blood pressure targets (<130/80 mmHg) should be implemented so as to reduce cardiovascular morbidity and mortality.18 On the current study only 12% of the study participants were found to have controlled blood pressure (<130/90 mmHg). With reference to less intensive blood pressure targets (<140/90), 43.8% of study participants have controlled blood pressure. One hundred and sixty-two (36.81%) patients had their blood pressure controlled (<140/90) in a study done at Cameroon17 which is slightly less as compared to the current study. The prevalence of uncontrolled hypertension in a study done at the rural communities of Thailand was 54.4%.19
Conclusion
Based on the study findings, the level of blood pressure control for hypertensive patients at Dessie Referral Hospital was very poor (12.3%) with a reference to the intensive blood pressure targets. A combination of two antihypertensive medications was most commonly used by those patients. Hydrochlorothiazide is the most commonly used drug from monotherapy. The combination of HCT and CCBs is the most prevalent combination anti-hypertensive drug used. Heart failure and stroke were the most common comorbid conditions identified.
Data Sharing Statement
All the data used for the study is contained within the manuscript.
Ethics Approval and Consent to Participate
The ethical clearance was obtained from the Department of Pharmacy, College of Medicine and Health Sciences, Wollo University. Informed verbal consent was obtained from the respondents and the Department of Pharmacy Ethical Review Board approved the verbal consent process. To keep the privacy, name of participants were omitted from the data collection format. The confidentiality of their personal information was kept according to the Declaration of Helsinki.
Acknowledgment
We would like to acknowledge administrators and pharmacists of DRH who help us during data collection and our deep appreciation goes to data collectors.
Author Contributions
All authors contributed to data analysis, drafting or revising the article, have agreed on the journal to which the article will be submitted, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Funding
No specific fund was available to undertake this study.
Disclosure
The authors declare that they have no conflict of interest.
References
1. Zhou D, Xi B, Zhao M, Wang L, Veeranki SP. Uncontrolled hypertension increases risk of all-cause and cardiovascular disease mortality in US adults: the NHANES III linked mortality study. Sci Rep. 2018;8(1):9418. doi:10.1038/s41598-018-27377-2
2. Chow CK, Teo KK, Rangarajan S, et al. Prevalence, awareness, treatment, and control of hypertension in rural and urban communities in high-, middle-, and low-income countries. JAMA. 2013;310(9):959–968. doi:10.1001/jama.2013.184182
3. Kibret KT, Mesfin YM. Prevalence of hypertension in Ethiopia: a systematic meta-analysis. Public Health Rev. 2015;36(1):14. doi:10.1186/s40985-015-0014-z
4. Wright JT, Whelton PK, Reboussin DM. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 374(23):2294.
5. Whelton PK, Carey RM, Aronow WS, et al. ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2017;71(6):e13–e115.
6. Williams B, Mancia G, Spiering W, et al. ESC/ESH guidelines for the management of arterial hypertension. Eur Heart J. 2018;39(33):3021–3104.
7. Teshome DF, Demssie AF, Zeleke BM, Shimosawa T. Determinants of blood pressure control amongst hypertensive patients in Northwest Ethiopia. PLoS One. 2018;13(5):e0196535. doi:10.1371/journal.pone.0196535
8. Horsa BA, Tadesse Y, Engidawork E. Assessment of hypertension control and factors associated with the control among hypertensive patients attending at Zewditu Memorial Hospital: a cross sectional study. BMC Res Notes. 2019;12(1):152. doi:10.1186/s13104-019-4173-8
9. Abdu O, Diro E, Abera Balcha MA, et al. Blood pressure control among hypertensive patients in University of Gondar Hospital, Northwest Ethiopia: a cross sectional study. Hypertension. 2017;140(1):6.
10. Animut Y, Assefa AT, Lemma DG. Blood pressure control status and associated factors among adult hypertensive patients on outpatient follow-up at University of Gondar Referral Hospital, northwest Ethiopia: a retrospective follow-up study. Integr Blood Press Control. 2018;11:37. doi:10.2147/IBPC.S150628
11. Bulatova NR, Yousef A-M, AbuRuz SD, Farha RA. Hypertension management and factors associated with blood pressure control in Jordanian patients attending cardiology clinic. Trop J Pharm Res. 2013;12(5):827–833.
12. Ernest Muthami Mutua MMG, Mbuthia B, Muiruri N, Jebet Cheptum J, Maingi T. Level of blood pressure control among hypertensive patients on follow-up in a Regional Referral Hospital in Central Kenya. Pan Afr Med J. 2014;18(278).
13. Degarege Yazie WS, Alebachew M, Berha AB. Assessment of blood pressure control among hypertensive patients in Zewditu Memorial Hospital, Addis Ababa, Ethiopia: a cross-sectional study. J Bioanal Biomed. 2018;10(3).
14. Shelley D, Tseng T-Y, Andrews H, et al. Predictors of blood pressure control among hypertensives in community health centers. Am J Hypertens. 2011;24(12):1318–1323. doi:10.1038/ajh.2011.154
15. Cheong A, Sazlina S-G, Tong S, Azah AS, Salmiah S. Poor blood pressure control and its associated factors among older people with hypertension: a cross-sectional study in six public primary care clinics in Malaysia. Malays Fam Physician. 2015;10(1):19.
16. Tadesse M, Abegaz OAA, Bhagavathula AS, Teni FS. Magnitude and determinants of uncontrolled blood pressure among hypertensive patients in Ethiopia: hospital-based observational study. Pharm Pract (Granada). 2018;16(2):1173. doi:10.18549/PharmPract.2018.02.1173
17. Alain Menanga SE, Nkoke C, Boombhi J, Musa AJ, Kuate L, Mfeukeu SK. Factors associated with blood pressure control amongst adults with hypertension in Yaounde, Cameroon: a cross-sectional study. Cardiovasc Diagn Ther. 2016;6(5):439–445. doi:10.21037/cdt.2016.04.03
18. Carey RM, Whelton PK. Prevention, detection, evaluation, and management of high blood pressure in adults: synopsis of the 2017 American College of Cardiology/American Heart Association Hypertension Guideline. Ann Intern Med. 2018;168(5):351–358. doi:10.7326/M17-3203
19. Meelab S, Bunupuradah I, Suttiruang J, et al. Prevalence and associated factors of uncontrolled blood pressure among hypertensive patients in the rural communities in the central areas in Thailand: a cross-sectional study. PLoS One. 2019;14(2):e0212572. doi:10.1371/journal.pone.0212572
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
