Back to Journals » Therapeutics and Clinical Risk Management » Volume 11
Bivalirudin plus loading dose of cilostazol-based triple-antiplatelet in treatment of non-ST-elevation myocardial infarction following percutaneous coronary intervention
Authors Wang M, Zhang G, Wang Y, Zhou K, Liu T, Zhang Y, Guo A, An Y, Zhang X, Li Y, Xie H
Received 17 April 2015
Accepted for publication 11 August 2015
Published 28 September 2015 Volume 2015:11 Pages 1469—1473
DOI https://doi.org/10.2147/TCRM.S86799
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Deyun Wang
Mei Wang, Guoru Zhang, Yaling Wang, Kun Zhou, Tao Liu, Yang Zhang, Anjun Guo, Yu An, Xiaodan Zhang, Yongjun Li
Department of Cardiology, The Second Hospital of Hebei Medical University, Shijiazhuang, Hebei, People’s Republic of China
Objective: To study the effect of bivalirudin plus loading dose of cilostazol-based triple-antiplatelet therapy strategy in patients undergoing percutaneous coronary intervention (PCI).
Methods: One hundred and fifty-three patients with non-ST-segment elevation myocardial infarction who underwent PCI were divided into control group and cilostazol group. Patients in control group were given aspirin and clopidogrel and those in cilostazol group were given aspirin, clopidogrel, and cilostazol once 2 hours before PCI and for 30 days after PCI. Bivalirudin was given to all patients before and during the PCI.
Results: After PCI, the Thrombolysis In Myocardial Infarction myocardial perfusion grade (TMPG) III in cilostazol group was higher than that in control group (89.19% versus 72.15%, P<0.05). At 30 days, the incidence of major adverse cardiac events was significantly lower in cilostazol group compared with that in control group (6.76% versus 17.72%, P<0.05). However, the rates of cardiac death, nonfatal reinfarction, target vessel revascularization, new congestive heart failure, and subacute stent thrombosis did not significantly differ between the two groups. In addition, the rates of minor or major bleeding or thrombocytopenia did not significantly differ between the two groups.
Conclusion: Bivalirudin plus loading dose of cilostazol-based triple-antiplatelet therapy strategy in PCI increased TMPG III, decreased major adverse cardiac events, and did not increase the incidence of bleeding and thrombocytopenia.
Keywords: triple-antiplatelet therapy, bivalirudin, percutaneous coronary intervention
Introduction
To reduce the incidence of thrombotic and bleeding complications during and following percutaneous coronary intervention (PCI), many different antithrombotic regimens have been investigated. Compared with the combination of heparin and glycoprotein IIb/IIIa inhibitors, the direct thrombin inhibitor bivalirudin significantly reduced the incidence of major bleeding after 30 days in patients with ST-segment elevation myocardial infarction undergoing primary PCI in a HORIZONS-AMI trial, but the risk of acute stent thrombosis increased within 24 hours.1 The early elevation in stent thrombosis with bivalirudin alone probably results from platelet activation induced by adenosine diphosphate before maximal thienopyridine blockade of the P2Y12 receptor or by the activity of residual thrombin following the discontinuation of bivalirudin. Cilostazol, as a selective and reversible phosphodiesterase type III inhibitor, exerts a unique vasodilatory and antithrombotic effect, according to a new mechanism.2,3 After PCI, triple-antiplatelet therapy (aspirin, clopidogrel, and cilostazol) has been proven to be correlated with a decreased incidence of stent thrombosis and major adverse cardiac events (MACE) compared with standard dual-antiplatelet therapy in certain clinical investigations.4,5 However, the effect of loading dose of cilostazol before PCI plus bivalirudin strategy in PCI procedure is largely elusive. This study is designed to evaluate the effects of loading dose of cilostazol-based triple-antiplatelet therapy plus bivalirudin strategy in patients with non-ST-segment elevation myocardial infarction treated with PCI.
Methods
Study patients
The patients who were diagnosed with non-ST-segment elevation myocardial infarction and underwent PCI were enrolled. Inclusion criteria were: 1) aged between 20 and 80 years; 2) accelerated or prolonged angina enduring over 20 minutes or recurrent episodes of angina at rest or during minimal exertion within the preceding 48 hours; 3) cardiac biomarker (creatine kinase MB or troponin) levels exceeding the upper limit of the normal range; 4) coronary stenoses which should be treated with PCI; and 5) undergoing PCI with drug-eluting stent implantation. Exclusion criteria were: 1) acute ST-segment elevation myocardial infarction or shock; 2) known bleeding disorders or liver disease; 3) thrombocytopenia; 4) calculated creatinine clearance level of <30 mL/min; 5) current warfarin use; 6) use of glycoprotein IIb/IIIa inhibitor, abciximab, or fibrinolytic; and 7) allergy to selected drugs or iodinated contrast which could not be premedicated. This study protocol was approved by the ethics committees of our hospital (The Second Hospital of Hebei Medical University, Shijiazhuang, Hebei, People’s Republic of China). Written informed consent was obtained from all of the patients.
Randomization and antiplatelet therapy
Patients were randomly divided into triple-antiplatelet group (cilostazol group) and dual-antiplatelet group (control group) according to a computer-generated randomization list. At least 2 hours before PCI, patients in the cilostazol group were given with 300 mg of aspirin (Bayer AG, Leverkusen, Germany), 600 mg of clopidogrel (Sanofi SA, Paris, France), and 200 mg of cilostazol (Otsuka Pharmaceutical Co, Zhejiang, People’s Republic of China), followed by aspirin 100 mg/day, clopidogrel 75 mg/day, and cilostazol 100 mg twice daily for 30 days. Those in the control group were given 600 mg of clopidogrel and 300 mg of aspirin, followed by aspirin 100 mg/day and clopidogrel 75 mg/day for 30 days.
Procedures of stent implantation
A dosage of 3,000 U of heparin was administered via intravenous route prior to coronary angiography. After the decision to conduct PCI, all patients received a dose of 0.75 mg of bivalirudin/kg (Litai pharmaceutical co., Ltd, Shenzhen, People’s Republic of China) followed by an infusion of 1.75 mg/kg/hour throughout the procedure. The activated clotting time was not monitored intraoperatively. Then, strictly according to the standard procedures, balloon predilatation and stent implantation were conducted.
Evaluation of therapeutic efficacy
Thrombolysis In Myocardial Infarction (TIMI) flow grade6 and TIMI myocardial perfusion grade (TMPG)7 were utilized to evaluate the culprit vessel flow and myocardial tissue-level perfusion. TMPG was evaluated merely in the region provided by the culprit vessel. Standard 2-dimensional echocardiography was used to evaluate left ventricular ejection fraction before and at 30 days after PCI. MACE, such as cardiac death, nonfatal reinfarction, target vessel revascularization, new congestive heart failure, or subacute stent thrombosis were also assessed at 30 days after PCI. Major bleeding was defined as a decrease in hemoglobin ≥2.0 mmol/L and the requirement for transfusion of ≥2 units of blood, or as retroperitoneal, intracranial, or gastrointestinal bleeding. Minor bleeding was defined as a decline in hemoglobin <2.0 mmol/L without the requirement to perform blood transfusion.8
Statistical analysis
Continuous data were expressed as x ± standard deviation (standard deviation). Continuous variables were statistically analyzed by Student’s t-test. Categorical variables were assessed by chi-square analysis. P<0.05 was considered as a statistical significance.
Results
Clinical and angiographic data at baseline
Enrollment of 153 patients was completed between October 2010 and August 2012. The baseline clinical and angiographic data of the patients are illustrated in Table 1. No significant differences were found in baseline characteristics between the two groups.
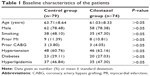  | Table 1 Baseline characteristics of the patients |
Coronary angiography results
No obvious difference was noted in the characteristics of the culprit vessels or the use of drug-eluting stents between two groups (Table 2). Prior to PCI, the mean TIMI flow grade and TMPG were almost equivalent between the two groups. Following PCI, the TMPG III in the cilostazol group was significantly higher than that in the control group, as shown in Table 3 (P<0.05).
Clinical results
As demonstrated in Table 4, the left ventricular ejection fraction did not significantly differ between the two groups before and at 30 days after PCI (both P<0.05). The MACE rate in the cilostazol group was significantly lower than that in the control group at 30 days after PCI (P<0.05). However, the rates of cardiac death, nonfatal reinfarction, target vessel revascularization, new congestive heart failure, and subacute stent thrombosis did not significantly differ between two groups.
Thrombocytopenia and bleeding complications
The rates of minor or major bleeding or thrombocytopenia did not significantly differ between the two groups (Table 4, P>0.05).
Discussion
Previous studies of antithrombotic strategy in patient who underwent PCI focused mostly on bivalirudin or triple-antiplatelet therapy after PCI. The ISAR-REACT 3 trial had shown that although bivalirudin failed to offer a net clinical benefit as compared with unfractionated heparin, it significantly decreased the incidence of major bleeding for patients with stable/unstable angina undergoing PCI after pretreatment with clopidogrel.9 In the ACUITY trial, patients with a moderate or high risk of acute coronary syndromes and receiving invasive therapy using glycoprotein IIb/IIIa inhibitors were enrolled, and it was demonstrated that bivalirudin was correlated with the incidence of bleeding and ischemia resembling those treated with heparin.10 In the HORIZONS-AMI trial,1 the risk of acute stent thrombosis was increased within 24 hours in patients who were diagnosed with ST-segment elevation myocardial infarction and underwent PCI. The early elevation in stent thrombosis with bivalirudin alone possibly results from platelet activation caused by adenosine diphosphate prior to maximal thienopyridine blockade of the P2Y12 receptor or by the activity of residual thrombin following the suspended use of bivalirudin. Adequate platelet inhibition probably leads to the reduced risk of ischemic clinical events.
Cilostazol is a potent type III phosphodiesterase inhibitor which was already well-known for its various benefits, such as antiplatelet and antithrombotic effects, vasodilating properties, reductions in clopidogrel resistance, and other pleiotropic actions.11–13 Cilostazol has been proven to suppress ADP-induced platelet aggregation, collagen, arachidonic acid, and epinephrine.14 Based on the studies above, combined administration of cilostazol, clopidogrel, and aspirin known as triple-antiplatelet therapy had been recommended. A previous study demonstrated that the incidences of death, myocardial infarction, target lesion revascularization, or stent thrombosis after stenting were reduced by approximately 50% using triple-antiplatelet therapy compared with those by dual-antiplatelet therapy.15 Recent clinical trials found that triple-antiplatelet therapy exerts a more potent inhibition upon ADP-induced platelet aggregation compared with dual-antiplatelet therapy.16,17 Previous studies demonstrated that triple-antiplatelet therapy decreased the risk of long-term cardiac and cerebral events after PCI for patients with acute coronary syndromes, especially those with high-risk profiles.18 But a trial involving 120 patients with stable angina demonstrated that adjunctive cilostazol pretreatment might not significantly reduce postprocedural myonecrosis after elective PCI in patients with stable angina.19
We found in the present study that triple-antiplatelet therapy plus bivalirudin strategy improved TMPG, was correlated with less MACE, and did not appear to raise the incidence of bleeding or thrombocytopenia in patients diagnosed with non-ST-segment elevation myocardial infarction who underwent PCI.
To our knowledge, this trial is the first research to show the effects of loading dose of cilostazol-based triple-antiplatelet therapy plus bivalirudin strategy in patients undergoing PCI. This investigation was designed to evaluate the clinical value of loading dose of cilostazol pretreatment prior to PCI. A recently published study showed that the loading dose of 200 mg cilostazol in addition to aspirin and clopidogrel improved platelet responsiveness to clopidogrel in the pre- and postprocedural phases and reduced the prevalence of high posttreatment platelet reactivity.20 In the present study, loading dose of cilostazol-based triple-antiplatelet therapy plus bivalirudin strategy in patients undergoing PCI improved myocardial perfusion and prognosis.
Obviously, the present study had some limitations. Firstly, the duration of the study period was not long. Moreover, the changes in pharmacokinetic and pharmacodynamic profiles early after antiplatelet therapy probably have affected the outcomes. Secondly, the number of study subjects was too small to accurately evaluate the clinical efficacy and safety of the regimens. Thirdly, the study specifically focused on the patients who were diagnosed with non-ST-segment elevation myocardial infarction and who underwent PCI. A study concerning people with no cardiovascular risk factors and with cardiovascular risk factors should be done to further extend our results.
Considering that drugs currently approved to coat stents used in PCI do not discriminate between proliferating vascular smooth muscle cells (VSMCs) and endothelial cells (ECs), which delays reendothelialization and vascular healing, increasing the risk of late thrombosis following angioplasty, Santulli et al21 developed a microRNA-based approach to inhibit proliferative VSMCs, thus preventing restenosis, while selectively promoting reendothelialization and preserving EC function. The results provide the basis for designing the next generation of selective therapy in PCI. The combination of a better stent platform and biodegradable polymer with this selective inhibition of VSMCs, without affecting ECs, has the potential to revolutionize the future of vascular interventional medicine.
Conclusion
Cilostazol-based triple-antiplatelet therapy improved TMPG and decreased MACE, and did not affect the incidence of bleeding or thrombocytopenia in non-ST-segment elevation myocardial infarction patients undergoing PCI.
Disclosure
The authors report no conflicts of interest in this work.
References
Stone GW, Witzenbichler B, Guagliumi G, et al. Bivalirudin during Primary PCI in Acute Myocardial Infarction. N Engl J Med. 2008;358:2218–2230. | ||
Yagi H, Yamaguchi N, Shida Y, et al. Cilostazol down-regulates the height of mural platelet thrombi formed under a high-shear rate flow in the absence of ADAMTS13 activity. Eur J Pharmacol. 2012;691(1–3):151–155. | ||
Meadows TA, Bhatt DL. Clinical aspects of platelet inhibitors and thrombus formation. Circ Res. 2007;100:1261–1275. | ||
Chen KY, Rha SW, Li YJ, et al. Triple versus dual antiplatelet therapy in patients with acute ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention. Circulation. 2009;119:3207–3214. | ||
Lee SW, Chun KJ, Park SW, et al. Comparison of Triple antiplatelet therapy and dual antiplatelet therapy in patients at high risk of restenosis after drug-eluting stent implantation (from the DECLARE-DIABETES and -LONG Trials). Am J Cardiol. 2010;105:168–173. | ||
No authors listed. The Thrombolysis in Myocardial Infarction (TIMI) trial. Phase I findings. TIMI Study Group. N Engl J Med. 1985;312:932–936. | ||
Zhao YJ, Fu XH, Ma XX, et al. Intracoronary fixed dose of nitroprusside via thrombus aspiration catheter for the prevention of the no-reflow phenomenon following primary percutaneous coronary intervention in acute myocardial infarction. Exp Ther Med. 2013;6:479–484. | ||
Bolognese L, Falsini G, Liistro F, et al. Randomized comparison of upstream tirofiban versus downstream high bolus dose tirofiban or abciximab on tissue-level perfusion and troponin release in high-risk acute coronary syndromes treated with percutaneous coronary interventions: the EVEREST trial. J Am Coll Cardiol. 2006;47:522–528. | ||
Kastrati A, Neumann FJ, Mehilli J, et al. Bivalirudin versus unfractionated heparin during percutaneous coronary intervention. N Engl J Med. 2008;359:688–696. | ||
Stone GW, Ware JH, Bertrand ME, et al. Antithrombotic strategies in patients with acute coronary syndromes undergoing early invasive management: one-year results from the ACUITY trial. JAMA. 2007;298:2497–2506. | ||
Kim IS, Jeong YH, Park Y, et al. Interaction analysis between genetic polymorphisms and pharmacodynamic effect in patients treated with adjunctive cilostazol to dual antiplatelet therapy: results of the ACCEL-TRIPLE (Accelerated Platelet Inhibition by Triple Antiplatelet Therapy According to Gene Polymorphism) study. Br J Clin Pharmacol. 2012;73:629–640. | ||
Shim CY, Yoon SJ, Park S, et al. The clopidogrel resistance can be attenuated with triple antiplatelet therapy in patients undergoing drug-eluting stents implantation. Int J Cardiol. 2009;134:351–355. | ||
Jeong YH, Lee SW, Choi BR, et al. Randomized comparison of adjunctive cilostazol versus high maintenance dose clopidogrel in patients with high post-treatment platelet reactivity: results of the ACCEL-RESISTANCE (Adjunctive Cilostazol Versus High Maintenance Dose Clopidogrel in Patients With Clopidogrel Resistance) randomized study. J Am Coll Cardiol. 2009;53:1101–1109. | ||
Holmes MV, Perel P, Shah T, Hingorani AD, Casas JP. CYP2C19 genotype, clopidogrel metabolism, platelet function, and cardiovascular events: a systematic review and meta-analysis. JAMA. 2011;306:2704–2714. | ||
Zhou H, Feng XL, Zhang HY, Xu FF, Zhu J. Triple versus dual antiplatelet therapy for coronary heart disease patients undergoing percutaneous coronary intervention: A meta-analysis. Exp Ther Med. 2013;6(4):1034–1040. | ||
Lee BK, Lee SW, Park SW, et al. Effects of triple antiplatelet therapy (aspirin, clopidogrel, and cilostazol) on platelet aggregation and P-selectin expression in patients undergoing coronary artery stent implantation. Am J Cardiol. 2007;100:610–614. | ||
Price MJ, Endemann S, Gollapudi RR, et al. Prognostic significance of post-clopidogrel platelet reactivity assessed by a point-of-care assay on thrombotic events after drug-eluting stent implantation. Eur Heart J. 2008;29:992–1000. | ||
Han Y, Li Y, Wang S, et al. Cilostazol in addition to aspirin and clopidogrel improves long-term outcomes after percutaneous coronary intervention in patients with acute coronary syndromes: a randomized, controlled study. Am Heart J. 2009;157:733–739. | ||
Kim BK, Oh SJ, Yoon SJ, Jeon DW, Ko YG, Yang JY. A randomized study assessing the effects of pretreatment with cilostazol on periprocedural myonecrosis after percutaneous coronary intervention. Yonsei Med J. 2011;52(5):717–726. | ||
Jin EZ, Yu LH, Li XQ. Loading effect of 200 mg cilostazol on platelte inhibition in patients undergoing percutaneous coronary intervention. Int Heart J. 2012;53:1–4. | ||
Santulli G, Wronska A, Uryu K, et al. A selective microRNA-based strategy inhibits restenosis while preserving endothelial function. J Clin Invest. 2014;124:4102–4114. |
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



