Back to Journals » Journal of Pain Research » Volume 12
Bipolar radiofrequency ablation of mandibular branch for refractory V3 trigeminal neuralgia
Authors Huang B, Xie K , Chen Y, Wu J, Yao M
Received 12 December 2018
Accepted for publication 23 March 2019
Published 9 May 2019 Volume 2019:12 Pages 1465—1474
DOI https://doi.org/10.2147/JPR.S197967
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Katherine Hanlon
Bing Huang,1 Keyue Xie,1 Yajing Chen,1 Jiang Wu,2 Ming Yao1
1Department of Anesthesiology and Pain Medicine, The First Affiliated Hospital, Jiaxing University, Jiaxing, Zhejiang 314000, People’s Republic of China; 2Department of Anesthesiology and Pain Medicine, University of Washington Medical Center, University of Washington, Seattle, WA 98195, USA
Background: Percutaneous trans-foramen ovale (FO) radiofrequency ablation (RFA) of Gasserian ganglion (GG) is commonly used to treat V3 trigeminal neuralgia (TN). However, this intracranial approach is less selective and safe.
Objectives: To report a novel percutaneous within-FO RFA of the V3 under CT-guidance and outcomes with both bipolar and monopolar techniques.
Patients and methods: Twenty-six patients with isolated V3 primary TN and FO >6 mm in diameter underwent either monopolar (n=12) or bipolar RFAs (n=14) based on their preference. Successful analgesia over V3, residual pain, recurrent pain, and complications were compared between the two groups. The ex vivo egg albumen model was used to demonstrate the size difference in the thermocoagulation lesion created by monopolar vs bipolar electrodes.
Results: In the bipolar group, there were more cases of masticatory atonia as compared to the monopolar (P=0.104), but no residual pain was observed. In the monopolar group, there were two cases of residual pain found, which led to immediate repeat RFAs. Therefore, during the immediate post-operative period, both groups obtained 100% complete V3 analgesia with a similar risk of facial hematoma (P=0.641). During up to 27-months of post-operative follow-up, in the bipolar group, complete pain relief persisted in all patients; in the monopolar group, 1 case of recurrent pain was found at 14 months. Ex vivo study demonstrated that, at 90 °C/90 seconds of RFA, the width of lesions is significantly larger by the 6-mm spacing parallel-tip bipolar electrodes compared to the monopolar electrode (9.5±0.567 vs 5.5±0.07 mm).
Conclusion: In treating patients with isolated V3 TN and FO >6mm in diameter, this percutaneously within-FO RFA of the V3 under CT guidance is both clinically practical and effective, while bipolar RFA is associated with a lower incidence of residual and recurrent pain likely due to larger lesion sizes.
Keywords: trigeminal neuralgia, mandibular nerve, foramen ovale, radiofrequency ablation, bipolar
Introduction
Trigeminal neuralgia (TN) is characterized by a recurrent, sudden, transient, and stereotyped attack of intense sharp or stabbing pain in the distribution of one or more branches of the trigeminal nerve.1,2 Specific branches are affected in the following percentages: the ophthalmic nerve (V1) 4%, the maxillary nerve (V2) 17%, the mandibular nerve (V3) 15%, and a combination of V2 and V3 around 32% of the time.3
Interventions are usually reserved for patients with debilitating, refractory primary TN who fail pharmacological therapy. For the subset of patients who would not tolerate or are unwilling to undergo surgical treatments such as microvascular decompression (MVD) or Gamma knife radiosurgery, the percutaneous trans-foramen ovale (FO) radiofrequency ablation (RFA) of the Gasserian ganglion (GG) remains one of the more attractive interventions given it is relatively low cost, minimally invasive, and safer.4,5,6,7
The percutaneous trans-FO RFA of GG, accessed via Hartel approach under fluoroscopic guidance, is associated with a treatment success rate of greater than 75%.8–10 The best outcome of RFA comes from primary TN and occurs with isolated V3 affection.11 However, this intracranial approach is less selective and safe. With repetitive RFA needle repositioning to search for the causative branch, it is not only associated with treatment failure and recurrent pain, but also associated with potential collateral damage to adjacent branches and a higher risk for severe neurological complications, such as intracranial hemorrhage, infections, subarachnoid injection, and others.8,9,12,
Incorporation of CT guidance facilitates both reliable identification of and the precise needle position within various orifices (supraorbital foramen, foramen rotundum, foramen ovale) through which, an individual branch of the trigeminal nerve exiting the skull. The intention to improve both clinic outcomes and patient safety profile has promoted the shift in treatment strategy of percutaneous RFA for TN from intracranial localization with the assistance of neurostimulation studies towards selectively extracranial localization of individual branch under CT guidance. The shift of interventional targets from intracranial GG to extracranial branches is reflected in recent literature using the extracranial within-FO monopolar RFA approach to ablate the V3.13,14
This monopolar approach provided better clinical outcomes but was associated with recurrent pain as well as residual pain at focal areas in the distribution of V3. This was particularly evident in patients with FO greater than 6 mm in width. The cause of the incomplete analgesia is unclear but likely due to inadequate thermocoagulation of the entire V3 branch as a result of incomplete coverage of FO by small monopolar lesion size.15 Bipolar RFA, however, is an adaption of monopolar RFA where the circuit is completed between two electrodes. Initially, each electrode forms a separate lesion, but the two lesions quickly coalesce, resulting in ablation of the additional volume of tissue between them as well. As a result, the total volume coagulated from the bipolar electrodes is slightly greater than the combined volume coagulated by two monopolar electrodes placed at the same sites.16
Therefore, to further improve outcomes of the monopolar approach in isolated V3 TN patients with FO greater than 6 mm in width, we assessed the feasibility of a novel bipolar RFA of the V3 branch within-FO under CT guidance. To prove that a larger lesion is created by bipolar RFA at the clinic parameters, we designed an ex vivo egg albumen model enabling direct measurement of the disparity in lesion size created by monopolar vs bipolar RFA. Finally, we report clinical outcomes and complications from both approaches in a set of 26 patients.
Patients and methods
Study patients
One hundred forty-seven patients met the International Classification of Headache Disorders, 3rd edition (ICHD-III) beta diagnostic criteria2 for isolated or combined primary V3 TN between January 2015 and December 2016 at the First Affiliated Hospital of Jiaxing University, China. Only 26 cases (17.7%) were identified as isolated V3 TN with FO greater than 6mm (by pre-procedural CT scan) and agreed to proceed with the RFA intervention, while the remained were not eligible to this study due to smaller FO, combined branches TN or not amendable to proceed with RFA. For each of these patients, there was no apparent hypo- or hyperesthesia in the distribution of the V3 branch or history of postherpetic neuralgia. CT and/or magnetic resonance imaging of brain ruled out potential secondary causes for TN, including both tumors of the cerebellopontine angle and vascular compression.
The study was approved by the Ethics Committee of The First Affiliated Hospital of Jiaxing University, China and conducted in accordance with the Declaration of Helsinki. The indications, benefits, risks, and alternatives of the CT-guided extracranial RFA of V3 within FO were fully disclosed and both monopolar and bipolar technique were offered to patients, who then voluntarily decided the approach of their choices. Subsequently, the written informed consent was obtained from each patient. In the monopolar group, one radiofrequency needle was used to access the center of the inner orifice of the FO. In the bipolar group, two radiofrequency needles were used to access the medial and lateral aspects of the inner orifice of the FO, respectively.
Preoperative workup included complete blood count (CBC), prothrombin time (PT), partial thromboplastin time (PTT), basic metabolic panel (BMP), and electrocardiogram (EKG). On the day of the procedure, patients stopped baseline pain medication and fasted for 6–8 hrs. A single physician performed all procedures under monitored anesthesia care.
Ct-guided selective extracranial radiofrequency neurolysis of mandibular branch within foramen ovale
Patient positioning for a CT scan
Patients were positioned supine with their shoulders supported on a pillow. Their heads were rested comfortably on the head-rest of the CT machine (Siemens Somatom Emotion system - Siemens HealthCare, Malvern, PA, USA) with wide tapes gently applied to prevent accidental head movement. The eyes, neck, and chest were protected with a radiation shield. A positioning grid was placed over the symptomatic cheek (Figure 1A), where a plane extending between the external auditory meatus and 2–3 cm lateral to the corner of the mouth was determined. Subsequently, a semi-coronal scan with a thickness of 3 mm was conducted parallel to this plane (Figure 1B).
The design of the needle pathway
Axial CT images were reviewed, and the FO was identified. The CT image frame that simultaneously captured the targeted FO including its external and internal openings was specifically chosen. The course of the needle trajectory was simulated on CT software and the skin entry point was selected to allow that a safe path existed without bony impediment to the advancement of the needle. Subsequently, the width of the FO, the needle entry angle, and the depth between the point of the needle’s skin entry to the opening of the FO were measured using the intrinsic CT ruler. For example, in a patient with FO diameter of 0.86cm in the bipolar group, the first needle pathway (line #2, 8.06cm in depth) was designed to reach the medial wall of the inner orifice of FO adjacent to the mandibular coronal process and the second needle pathway (line #1, 7.9 cm in depth) was designed to reach the lateral wall of the inner orifice of FO with the lateral to medial angulation of 15° (Figure 2A). Meanwhile, for a patient with FO diameter of 0.703cm in the monopolar group, only one needle pathway (8.438cm in depth) was designed to reach the center of the inner orifice of FO with the lateral to medial angulation of 16.7° (Figure 2C). Subsequently, the needles were marked to this depth.
The needle placement under intermittent CT guidance
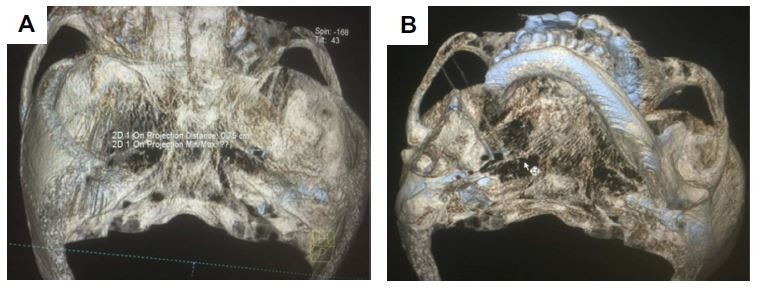
The skin entry site and subcutaneous tissues were first infiltrated with 2 milliliters of 1% lidocaine using a 27-gauge needle. Following the predetermined parameters (the angle, path, and depth), a straight, sharp 5-mm bevel-tipped 20-gauge 3.5-inch radiofrequency cannulas (Cosman) was advanced with intermittent CT guidance until reaching the desired locations (Figure 2B and D). Precise needle control by the operator was required to navigate the narrow passage between the zygomatic arch, the mandible, and the posterior wall of the maxillary sinus. The final position of bipolar needle placement at the skin surface is shown in Figure 3A and B. The final position of bipolar needle placement within right FO (0.75cm in diameter) i further demonstrated in three dimensional CT images via the superior view (Figure 4A) and the inferior view of the skull base the (Figure 4B).
Radiofrequency ablation protocol
Once the needles were in final positions and negative aspiration of blood or cerebral spinal fluids was obtained, the stylet of RFA cannulas was replaced with nitionol TC electrodes (Cosman TCN-10). A sensory test at 50 Hz with pulse width at 500uS and amplitude at 0.2–1.0 mA was performed to generate paresthesia at the distribution of V3 via the radiofrequency machine (Baylis Medical Company Inc. Toronto, ON, Canada). A motor test at 2 Hz with a maximum of 1.0 mA was negative for an unwanted motor response from adjacent branches. Successful needle placement was defined by 1) precise needle placement that reached the desired targets in the FO as planned, and 2) satisfactory neurostimulation tests, which include either a positive sensory test described as paresthesia in the territory of V3 and/or a positive motor test for fine and rhythmic quivering of mandible without any unwanted muscle twitches. After obtaining both subjective and objective endpoints, radiofrequency ablation using two cycles of the fixed-dose mode of 90 °C for 90 seconds was performed under deep sedation. No local anesthetics were injected prior to the ablation in order to enable immediate post-procedural evaluation of sensory block.
Post-procedural observation
Patients were transported back to the postprocedural room for full recovery. The pinprick test was performed to detect sensory block at the skin over the mandible and the fleshy part of the cheek, (buccal nerve), the lower lip (mental nerve), tongue (Lingual nerve), part of the auricle of the ear and part of the temple (auriculotemporal nerve). The complete sensory block is defined as the objective lack of pain to pinprick stimulation over all four areas of main branches; whereas, the residual pain is defined as persistent pain over one or more territories of these four main branches. The sensory blockade was recorded along with continuous monitoring of vital signs for at least four hours prior to the discharge.
The recurrent pain is defined as pain that returns over the symptomatic area after initial pain relief following RFA. Recurrent pain was determined during the post-procedural follow-up visits per their report.
Primary and secondary outcomes
The primary clinical outcome is whether complete sensory block over the V3 distribution is achieved, both immediately and long-term (yes vs no). The secondary clinic outcomes include the presence of residual pain, recurrent pain, and adverse clinical events (hematoma, infection, masticatory weakness, and corneal involvement et al). Each of these outcomes was observed and collected by an independent study coordinator during the post-operative recovery period, at the in-office follow-up after 1 week, and during the 1-, 6-, 12-, 24- and up to 27-month follow-ups over the phone.
In addition to patient’s demographic information, procedural data were also collected including the diameter of FO, procedural length (the time from needle skin insertion to positive V3 paresthesia induced upon electric stimulation), and the neurostimulatory test results between two groups.
Ex vivo study of the lesion created by bipolar vs monopolar RFA
An ex vivo egg albumen model was used as a medium mimicking the in vivo environment. The same RFA cannulas (Cosman) and electrodes as clinically used were completely submerged into the medium so that egg albumen surrounded the active tips. In bipolar group, two electrodes were placed parallelly 6 mm apart and connected to the output jacks of an RF generator (Baylis Medical Company Inc. Toronto, ON, Canada). The generator automatically adjusted the amplitude of a sinusoidal signal to keep the temperature of active tips within the target temperature of 90±2 °C. After heating was complete, the electrode was cooled to near 33 °C. Photographs of lesions were taken directly above the cannulae/electrodes, with a metric ruler lying above it for reference. The width of resultant thermocoagulation lesions from the monopolar group and the bipolar group at 30-, 60- and 90-second time points were manually measured to analyze the effect of heating times on the size of lesions.
Statistical analysis
SPSS 16.0 software (SPSS, Inc, Chicago, IL, USA) was used to analyze the data. Continuous variables were shown as mean ± SD and compared between the groups using Student’s t-test. Whereas categorical data were presented as numbers and percentages and compared using the Fisher’s Exact Test. P-values <0.05 were deemed statistically significant.
Results
There were 26 patients enrolled in either the monopolar (N=12) or bipolar (N=14) group. The age of study patients ranged from 49 to 88 years with an average of 69.35 years (±10.06 [SD]). The duration of pain ranged from 16 to 132 months, with an average duration at 47.54 months (±22.02 [SD]). There were 12 males (8 in the bipolar group and 4 in the monopolar group) and 14 females (6 in the bipolar group and 8 in the monopolar group). There were 14 patients with V3 TN on the left side and 12 patients with symptoms on the right side. The patients consented in the bipolar group were on average about 15 years younger than those in the monopolar group (61.71±5.78 vs 78.25±5.48, P=1.099X10−7). Between monopolar and bipolar groups, there was not a statistically significant difference in either duration of TN (45.64±27.99 vs 49.75±12.91, P=0.6287) or size of FO (6.47±0.61 vs 6.99±0.71, P=0.113). Demographic information and FO measurement data of those 26 patients are summarized in Table 1.
The duration of needle placement, neurostimulatory test results, and both immediate and long-term post-operative complications and outcomes in each group were summarized in Table 2. Intraoperatively, both groups achieved a 100% success rate of optimal needle placement (as defined in Radiofrequency ablation protocol) prior to the continuous radiofrequency thermocoagulation therapy. When compared to the monopolar technique, the bipolar technique was associated with about 3 mins longer procedural time (17.4±5.3 mins vs 14.2±4.7 mins, P=0.038) and similar V3 paresthesia threshold (o.75±0.21 vs 0.65±0.18, P=0.178).
During the immediate post-operative period, both groups obtained 100% complete and persistent V3 sensory block (14/14 vs 12/12) with a comparable risk of post-procedural facial hematoma (2/14 vs 2/12, P=0.641) and risk of masticatory atonia (8/14 vs 2/12, P=0.104) (Table 2). No residual pain was observed in the bipolar group. However, in the monopolar group, there were two cases of residual pain (2/12) found: one had pain at the tip of the tongue in the territory of the lingual branch and another had pain at the ear and temporal region in the territory of the auriculotemporal branch. Subsequently, a repeat monopolar radiofrequency ablation was immediately performed to achieve 100% pain resolution.
The duration of post-operative follow-up ranged from 3 to 27 months, with an average duration at 14.7 months (±5.1 [SD]). In the bipolar group, complete pain relief persisted in all patients (14 out of 14) over an average duration of 15 months (±6.38). In the monopolar group, 1 case of recurrent pain was found at 14-month follow-up over an average duration of 13 months (±7.87) and the rest of the cases (11 out of 12) resulted in sustained and complete pain relief. No statistical difference (P=0.429) in the duration of follow-up was found between these two groups (Table 2). In the up to 27-months of post-operative period, no cases were lost to follow-up.
The ex vivo study using egg albumen as a model demonstrated that the diameters of lesions (n=10) created by the bipolar RFA needle surround its tip in an oblate spheroid shape and are significantly larger than those (n=10) created by the monopolar RFA needle at 90 °C. This was true over 30-second (3.4 mm ±0.516 vs 3.5 mm ±0.527, P=0.678) 60-second (8.1mm ±0.568 vs 4.3 mm ±0.823, P=4.32 X10−6) and 90-second (9.5mm ±0.567 vs 5.5 mm ±0.707, P=8.52X10−8) time points. Specifically, at 90 °C/90 seconds, the monopolar RFA electrode created a lesion of 6 mm in the largest diameter (Figure 5B), whereas the 6 mm spacing parallel-tip bipolar RFA electrodes created a lesion of 10 mm in the largest diameter (Figure 5A).
Discussion
In our study, there was no statistically significant difference in either the preceding duration of TN symptoms or the size of FO between the monopolar and bipolar groups, although the patients consented in the bipolar group were on average about 15 years younger than those in the monopolar group. The age difference is likely due to the non-randomized study design and influenced by the clinic factors such as individual tolerance of procedure, medical comorbidities, the cost associated RFA needle (more expensive with bipolar RFA), the fear of procedural pain and complications. Overall, the elder patients tended to choose the monopolar technique; whereas the younger patients preferred the bipolar technique in hope to achieve better outcomes.
Both extracranial monopolar and bipolar techniques were approved technically feasible. A 100% success rate of intraoperative optimal needle placement was achieved in both groups, with only 3 mins longer in procedural time and similar V3 paresthesia threshold in the bipolar group as compared to the monopolar group. The longer procedural time is expected due to the additional needle placement in the bipolar group. The similar V3 paresthesia threshold obtained below 1 mA between two groups is consistent with the common belief that the positive paresthesia obtained under 1.0 mA usually indicates that the tip of the needle is close enough to incorporate the V3 branch within the thermocoagulation lesion.
Both extracranial monopolar and bipolar techniques led to complete and persistent V3 analgesia with a comparably small risk of immediate post-procedural facial hematoma. The 100% treatment success rate is significantly higher than the reported intracranial GG RFA approach.8,9 Although the bipolar group is associated with a higher incidence of masticatory atonia (P=0.104), we report no cases of residual pain or recurrent pain after over two-year of follow-up. Conversely, the monopolar group had two cases of residual pain during the immediate post-operative period: one at the tip of the tongue and another at the ear and temporal region. The V3, on its extracranial course, divides into four sub-branches: the buccal, lingual, mental, and auriculotemporal nerves. We suspected that the residual pain at the tip of the tongue was from inadequate ablation of the lingual branch, and the residual pain at the ear and the temporal region was from inadequate ablation of the auriculotemporal branch. Therefore, repeat monopolar radiofrequency ablations by advancing the monopolar RF needle towards the medial wall of the FO (to target the lingual branch) and towards the lateral wall of the FO (to target the auriculotemporal branch) were subsequently performed and resulted in complete and persistent V3 analgesia. The monopolar group also resulted in one case of recurrent pain at 14-month follow-up.
RFA lesion size depends on multiple factors, including active tip diameter/gauge, tip length, tip temperature, and lesion time. Furthermore, the inter-tip spacing influences bipolar lesions. It is crucial for the monopolar RFA needle to be close in proximity to the V3 branch for complete ablation. Although the width of the monopolar lesion at 20 Gauge/5 mm/80 °C/120 seconds was reported as 6.1 mm in the Cosman study, neither the average nor standard deviation dimensions of the monopolar or bipolar lesions at our operating parameters of 20 Gauge/5 mm/90 °C/90 seconds were ever reported.16 Egg albumen primarily consists of about 90% water, into which is dissolved about 10% protein, 1% carbohydrates, and negligible fat. It is an excellent medium to simulate the differences in lesion sizes generated by monopolar vs bipolar RFA at out clinic parameters. Using the same cannulae/electrodes in the ex vivo egg albumen model, at 20 Gauge/5 mm/90 °C/90 seconds, our study reported that the lesion created by 6 mm spacing parallel-tip bipolar RFA needles was 10 mm (9.5±0.567, n=10) in the largest diameter vs a lesion of 6 mm (5.5±0.707, n=10) in the largest diameter by the monopolar one.
Based on the results from our ex vivo egg albumen model, in patients with FO greater than 6 mm in diameter, there is an innate likelihood of failing to completely incorporate the targeted V3 by the monopolar RFA at 20 Gauge/5 mm/90 °C/90 seconds, which subsequently leads to the incidence of residual and recurrent pain if the monopolar electrode is not optimally placed. This hypothesis is supported by the data of neurostimulation tests from a previous study, in which the satisfactory sensory endpoints were easily achieved with small currents (0.1–0.3 mA) in patients with FO less than 6 mm. Meanwhile larger currents (0.5 −1.0 mA) were sometimes necessary to induce satisfactory paresthesia.15 To achieve the complete coverage of the FO >6 mm in diameter, the larger lesion created by bipolar electrodes seems essential to better outcomes and reduce the incidence of residual pain and recurrent pain . In addition, our study demonstrates that larger bipolar lesions within the FO are not associated with unwanted adverse events or complications, which is not too surprising in the less anatomically critical extracranial region. However, there is no study to compare the complication rates between intracranial and extracranial approach and our study’s sample size might be too small to make such a favorable conclusion regarding the safety of extracranial approach.
Furthermore, although the placement of bipolar needles within FO has presumably been time-consuming and technically challenging, with an improvement in skill set, the 3 mins of difference in procedural time is probably clinically insignificant. It is, however, possible that this bipolar approach might be limited by the availability of and the experience of operators with using CT guidance. As such, this technique might not be as practical as a matrix lesion created by multiple passages with a single RFA needle. Regardless, our study does provide evidence supporting the feasibility of extracranial bipolar RFA approach and the larger lesion created by bipolar RFA when treating FO greater than 6 mm in diameter.
There are several methodological limitations preventing this study to clearly establish the superiority of bipolar over monopolar RFA techniques. First, there is a potential bias associated with the non-randomization design of this study. While the randomization design is an invaluable statistical strategy for the mathematical exploitation of uncertainty, but it brings inherent ethical issues.17 By accommodating the patients’ preference of RFA techniques based on their choices, our non-randomization design is probably the most practical way to achieve the goals of both improving medical knowledge and benefiting the patients from the results of trials, especially given the highly invasive nature of the procedures and patients’ needs for effective treatment. Second, there is less statistical power associated with the small sample size. In light of the current shift of RFA targets from the intracranial Gasserian Ganglion to the individual branch at the existing foramina under CT guidance to promote the highly selective and safer RFA therapy for TN, our study serves as a feasibility study of the percutaneous within-FO RFA of the V3 with either monopolar or bipolar techniques. To avoid the complicated pain patterns in combined (including V3) primary TN, the highly specific patient population with isolated V3 TN and with FO >6 mm was selected for simplified clinical observation. Once the satisfactory outcomes from bipolar or monopolar within-FO RFA of V3 are confirmed, this approach could be widely applied as part of the extracranial approach for combined branches TN patient population. Despite our extensive experiences in the interventional treatment of TN and the largest TN patient population in East China, the enrollment of such highly selective V3 TN subjects has been very difficult and slow. We have only 26 cases enrolled over the timespan of two years. Therefore, this study might not have large enough sample size to detect a statistically significant difference or reliably prove the absence of difference in the various parameters measured between the two groups such as the incidence of masticatory atonia, residual pain or recurrent pain (all P>0.05). However, we provided the feasibility study of this novel percutaneously within-FO RFA of the V3 under CT-guidance and collected data for the sample size calculation and power analysis for future study design. Third, there is a concern of higher incidence of masticatory atonia in the bipolar group, although no statistical difference between the two groups, which could potentially limit the use of the bipolar technique. On the other hand, V3 branch innervates four mastication muscles including the masseter, temporalis, medial pterygoid and lateral pterygoid. Complete ablation of V3 is inevitably associated with the risks of masticatory weakness, which might be a clinical indicator of complete ablation and a predictor of better outcomes. It was reported that masticatory weakness occurs from 10% to as high as 51% in a certain approach and has no long-term clinical significance.18,19 Luckily most cases of masticatory atonia typically resolved within 6 months but could take as long as 1 year, which is consistent with our clinical observation.
Conclusion
In light of the current shift of RFA targets from the intracranial Gasserian Ganglion to the individual branch at the existing foramen under CT guidance to promote the highly selective and safer RFA therapy for TN, our study demonstrated that this novel percutaneous within-FO RFA of V3 with either monopolar or bipolar techniques can be both safely and reliably performed in patients with larger foramen ovales. Both extracranial monopolar and bipolar techniques led to nearly 100% complete and persistent V3 analgesia. Although the statistical differences in the various parameters measured between the two groups such as the incidence of masticatory atonia, residual pain or recurrent pain have yet to be determined due to the small sample size. Our study suggested this bipolar approach might be a better alternative to the monopolar approach in instances where the FO diameter is greater than 6 mm. The better outcomes from the bipolar approach can be implicated by larger lesion size created by bipolar as compared to monopolar electrodes and supported by our ex vivo study. All these limitations warrant a more cautious attitude advocating of bipolar approach and calls for higher-quality evidence by rigorous larger-scale and well-designed RCTs
Acknowledgments
This work was funded by the research grants from the Key Programs of the Medical Platform of Zhejiang Province (2016ZDA018).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Montano N, Conforti G, Di Bonaventura R, Meglio M, Fernandez E, Papacci F. Advances in diagnosis and treatment of trigeminal neuralgia. Ther Clin Risk Manag. 2015;11:289–299. doi:10.2147/TCRM.S37592
2. Olesen J. International classification of headache disorders. Lancet Neurol. 2018;17(5):396–397. doi:10.1016/S1474-4422(18)30085-1
3. Vorenkamp KE. Interventional procedures for facial pain. Curr Pain Headache Rep. 2013;17(1):
4. Jin HS, Shin JY, Kim YC, et al. Predictive factors associated with success and failure for radiofrequency thermocoagulation in patients with trigeminal neuralgia. Pain Physician. 2015;18(6):537–545.
5. Tang YZ, Wu BS, Yang LQ, et al. The long-term effective rate of different branches of idiopathic trigeminal neuralgia after single radiofrequency thermocoagulation: A cohort study. Medicine (Baltimore). 2015;94(45):e1994. doi:10.1097/MD.0000000000000874
6. Emril DR, Ho KY. Treatment of trigeminal neuralgia: role of radiofrequency ablation. J Pain Res. 2010;3:249–254. doi:10.2147/JPR.S14455
7. Gronseth G, Cruccu G, Alksne J, et al. Practice parameter: the diagnostic evaluation and treatment of trigeminal neuralgia (an evidence-based review): report of the quality standards subcommittee of the american academy of neurology and the european federation of neurological societies. Neurology. 2008;71(15):1183–1190. doi:10.1212/01.wnl.0000326598.83183.04
8. Wu CY, Meng FG, Xu SJ, Liu YG, Wang HW. Selective percutaneous radiofrequency thermocoagulation in the treatment of trigeminal neuralgia: report on 1860 cases. Chin Med J (Engl). 2004;117(3):467–470.
9. Gokalp HZ, Kanpolat Y, Tumer B. Carotid-cavernous fistula following percutaneous trigeminal ganglion approach. Clin Neurol Neurosurg. 1980;82(4):269–272.
10. Tang YZ, Jin D, Li XY, Lai GH, Li N, Ni JX. Repeated CT-guided percutaneous radiofrequency thermocoagulation for recurrent trigeminal neuralgia. Eur Neurol. 2014;72(1–2):54–59. doi:10.1159/000357868
11. Fouad W. Management of trigeminal neuralgia by radiofrequency thermocoagulation. Alexandria J Med. 2011;47(1):79–86. doi:10.1016/j.ajme.2011.02.001
12. Kanpolat Y, Savas A, Bekar A, Berk C. Percutaneous controlled radiofrequency trigeminal rhizotomy for the treatment of idiopathic trigeminal neuralgia: 25-year experience with 1,600 patients. Neurosurgery. 2001;48(3):
13. Telischak NA, Heit JJ, Campos LW, Choudhri OA, Do HM, Qian X. Fluoroscopic C-arm and CT-guided selective radiofrequency ablation for trigeminal and glossopharyngeal facial pain syndromes. Pain Med. 2018;19(1):130–141. doi:10.1093/pm/pnx088
14. Huang B, Yao M, Feng Z, et al. CT-guided percutaneous infrazygomatic radiofrequency neurolysis through foramen rotundum to treat V2 trigeminal neuralgia. Pain Med. 2014;15(8):1418–1428. doi:10.1111/pme.12440
15. Xie K, Huang B, Yao M. Radiofrequency via outside of fossa ovalis to treat auriculotemporal neuralgia in a patient. Chin J Anesthesiol. 2017;37(2):254–255.
16. Cosman ER
17. Colli A, Pagliaro L, Duca P. The ethical problem of randomization. Intern Emerg Med. 2014;9(7):799–804. doi:10.1007/s11739-014-1118-z
18. Ding W, Chen S, Wang R, et al. Percutaneous radiofrequency thermocoagulation for trigeminal neuralgia using neuronavigation-guided puncture from a mandibular angle. Medicine (Baltimore). 2016;95(40):e4940. doi:10.1097/MD.0000000000004864
19. Broggi G, Siegfried J. The effect of graded thermocoagulation on trigeminal evoked potentials in the cat. Acta Neurochir (Wien). 1977;(issue 24):175–178.
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.







