Back to Journals » Substance Abuse and Rehabilitation » Volume 14
Bio-Psycho-Social Profile of People with Substance Use Disorders Treated in Locally Assigned Treatment Facilities in Kandahar, Afghanistan
Authors Stanikzai MH , Wahidi MW
Received 16 March 2023
Accepted for publication 2 August 2023
Published 7 August 2023 Volume 2023:14 Pages 89—98
DOI https://doi.org/10.2147/SAR.S412821
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Rajendra D. Badgaiyan
Muhammad Haroon Stanikzai, Mohammad Wahid Wahidi
Department of Public Health, Faculty of Medicine, Kandahar University, Kandahar, Afghanistan
Correspondence: Muhammad Haroon Stanikzai, Department of Public Health, Faculty of Medicine, Kandahar University, District # 10, Kandahar, 3801, Afghanistan, Tel +93704775578, Email [email protected]
Background: Substance use and its associated bio-psycho-social problems are public health concerns with harmful individual and social consequences.
Objective: This study assessed the bio-psycho-social profile of people with substance use disorders (SUD) treated at locally assigned treatment facilities in Kandahar, Afghanistan.
Methods: We conducted this facility-based cross-sectional study among 621 substance users receiving care at three locally assigned treatment facilities in November-December 2022. We performed multiple linear regression to determine factors associated with psychological symptoms.
Results: The mean age of the participants was 34.41 (± 10.10 SD) years. The majority of our subjects (81.2%) perceived their physical health as very good or fair. More than two-thirds (73.4%) rated their social support as high. Of all participants, 541 (87.1%) had symptoms of depression, 569 (91.6%) of anxiety, and 442 (71.2%) of stress. The prevalence of severe depression, anxiety, and stress was 34.8%, 65.8%, and 27.3%, respectively. The multiple linear regression showed that several attributes of people with substance use disorders [ie, having a low level of education (β=0.12, p=< 0.001), being unemployed (β=0.31, p=< 0.001), having a low level of social support (β=− 0.35, p=< 0.001), had a pre-existing medical condition (β=− 0.28, p=< 0.001), and having lived abroad in the past ten years (β=0.10, p=0.001)] were significantly associated with higher DASS-21 total scores.
Conclusion: This study highlights the importance of providing bio-psycho-social support programs and implementing therapeutic interventions to help people with substance use disorders, particularly those who are most susceptible to higher levels of bio-psycho-social problems.
Keywords: depression, anxiety, stress, social support, co-morbidity, rehabilitation centers
Introduction
Afghanistan, in addition to the decades of armed conflict and the severity of the humanitarian crisis, is frequently at the top news headlines or global agenda for opium production, drug trafficking, and substance use.1,2 Although there are local routine reports on opium production and drug trafficking, they discount the information on its long-term bio-psycho-social sequelae, such as adverse health outcomes and social problems, which in turn may lead to ill health and even social malfunctioning.2 While it is well-known that substance use leads to the emergence of bio-psycho-social imperfections in a large number of cases, these disorders are largely under-reported.
Depending upon substance use vulnerability factors, such as socioeconomic conditions, substance availability, peer behavior, and access to therapeutic and preventive measures, the prevalence of substance use disorders (SUD) is significantly variable.3–5 Worldwide, over 2% of the population has alcohol or other substance use.6 The prevalence of these disorders is high as 5% in the USA and Eastern Europe.6 In 2015, the Afghanistan National Drug Use Survey (ANDUS) found that the prevalence of substance use was 11% and higher among male adults.7,8 This high prevalence is attributed, in part, to the ongoing decades of conflict, unlimited availability of cheap narcotics, and limited access to treatment and preventive services.5,7 Opioids (4.9%), cannabis (2.2%), and prescription sedatives (about 1%) are the most common substances used in Afghanistan.7,8
The biological impact of substance use has been explored in the relevant literature.9,10 According to the literature, substance use, including alcohol, heroin, marijuana, and cocaine, is independently associated with an increased risk for chronic pain, cancer, and heart disease that compromise the normal functioning of people with substance use disorders.3,9 In addition to chronic disorders, there has been an increase in the risk of infectious disease transmission, including Human Immunodeficiency Virus (HIV) and hepatitis C virus (HCV).9,10 However, in the developing world, especially Afghanistan, its impact is under-reported.
The psychological consequences of substance use and its effects on family members are substantial.9,11 Depression, anxiety, stress, and sleeplessness are frequently reported.9 Long-term impacts include paranoia, psychosocial dependence and a higher inclination to chronic mental disorders, suicidal ideation, and self-harm intentions.9–11 Pertinent literature reported that patients with mental health disorders are prone to substance use and vice versa.10,11 Additionally, substance use and its related bio-psycho-social challenges are likely to harm the families of the substance users involved.12 The nearly four decades-long persistent warfare in Afghanistan and its inevitable multitude of consequences have most certainly contributed immensely to the increased psychological burden, particularly among Afghans with substance use disorders.
In light of the aforementioned global data from peaceful and resourceful countries, the extent of the impact of this public health concern in Afghanistan, a country torn by nearly half a century-long war that continues to this day, is almost neglected. Considering the above gap in knowledge, this study aimed to address this lacuna by assessing the bio-psycho-social profile of people with substance use disorders treated at locally assigned treatment facilities in Kandahar, Afghanistan. This assessment will probably prove worthwhile in reflecting the necessity for healthcare services, especially mental health services, in these settings and providing implicit insight to relevant humanitarian assistance providers.
Materials and Methods
Study Settings and Design
We conducted this facility-based cross-sectional study among people with substance use disorders receiving care at three locally assigned treatment facilities in Kandahar, Afghanistan, from November to December 2022. The locally assigned treatment facilities were a public rehabilitation center (22 clients), private rehabilitation center (13 clients), and correctional institution (586 clients). At the time of inclusion, the aforementioned centers were locally assigned to treat people with substance use disorders and were supported by governmental and non-governmental organizations. People with substance use disorders come to these centers in multiple ways; about 80% of them are referred by local authorities, and the remaining are self-referred. Patients admitted to these centers can receive primary health screening at the on-site health clinics. This initial visit also serves as an opportunity to test for sexually transmitted diseases, including HIV and HCV. Within the first week of arrival, the substance users at these centers visit the treatment facilities to develop a treatment plan. Psychiatric services are also routinely provided on-site; additional referrals to Mirwais Regional Hospital are arranged (if required) for more specialized care. The services provided in these three centers are largely similar to those described in our paper, with predominately several advantages (better treatment) in private rehabilitation centers.
Study Population
All people with substance use disorders living in the southwest of Afghanistan during the data collection period were the source population. The study population consisted of all substance users treated at locally assigned treatment facilities in Kandahar, Afghanistan. We excluded substance users with severe illness, those with compromised consciousness (unable to understand/utter a normal verbal response or not fully awake/alert), and those who refused to participate in the study. We approached 685 people with substance used disorders treated at locally assigned treatment facilities. The response rate was 92.2% (632). The final analysis consists of 621 participants with their complete data sets.
Study Measures
The socio-demographical characteristics of our participants encompassed age, gender, marital status, educational background, occupation, and documented travel history or living abroad.
In this study, we employed the term substance use disorder to “any problematic pattern of using alcohol or another substance that results in impairment in daily life or noticeable distress” based on DSM-5.13 Additionally, the term “psychological” refers to the symptoms of depression, anxiety, and stress.
Substance use-related variables were the type and frequency of drugs used and the age at first use. Other variables of interest included a prior attempt to quit and their reasons for failure. The presence of concomitant medical conditions and hospitalization were health-related characteristics of the people with substance use disorders.
This study employed the Depression, Anxiety, and Stress (DASS-21) scale to measure the presence and severity of psychological symptoms during the last two weeks and assess the prevalence of probable depression, anxiety and stress.14,15 DASS-21 is a 4-point scale from 0 (not at all) to 4 (extremely) that yields a total score from 0 to 84. The questionnaire is a globally credible instrument with good psychometric properties for assessing depression, anxiety, and stress based on DSM-IV criteria.15 The internal consistency (Cronbach’s alpha) value for the Pashtu version in the present study, respectively, was 0.75, 0.77, 0.70, and 0.88 for depression, anxiety, stress, and DAS-21 total scales.
Data Collection
The study questionnaire was initially drafted in English and subsequently translated into local language (Supplementary Figure 1) for the convenience of interviewing the respondents. After the translation process, a pilot test was conducted to assess the clarity and simplicity of the questionnaire among a small group of participants who were similar to the study population in terms of age, sex, and education level (Kandahar Teaching Hospital). The pilot test results were used to refine the questionnaire and ensure that it was culturally appropriate and linguistically accurate for the target population.
The data were collected by four male nurses and one supervisor (Master of Public Health Program trainee). They were provided with one-day classroom training on sampling, interviewing, filling out questionnaires, and addressing potential ethical concerns that may emerge during the study, followed by one day of practical field training. The interviewer screened and interviewed every consecutive client (non-probability sampling technique) treated in one of the locally assigned treatment facilities. Before their invitation to voluntarily participate, the recruiters offered the potential participants a written synopsis of the study objectives and information on the course of the research. If the client would like to participate, they could willfully date and sign the consent form. Only then the survey team interviewed the participants. Each interview took about 15–20 minutes. Daily, we checked the questionnaires for completion. We kept the completed questionnaires in locked cabinets and stored the electronic data in password-protected computers to which only the principal investigators had access.
Statistical Analysis
We employed the Statistical Package for Social Sciences (SPSS) version 22 for data analysis.16 We conducted descriptive statistics to understand participants’ bio-psycho-social characteristics. The total score of DAS-21-total, depression, anxiety, and stress was calculated as the sum of the component scores and multiplied by two.14 Since the three subscales of depression, anxiety, and stress were strongly associated with each other (depression-anxiety: Pearson r= 0.7, P <0.001; anxiety-stress: Pearson r= 0.7, P <0.001; depression-stress: Pearson r= 0.8, P <0.001). Therefore, we used the DASS-21 total score in a linear regression model to assess factors associated with psychological symptoms in the sample.17 The alpha level was set at P < 0.05.
The following characteristics of the people with substance use disorders were entered into the model:
Model: Educational attainment, employment status, marital status, pre-existing medical condition, level of social support, and history of living abroad in the past ten years.
Results
From the three locally assigned treatment facilities, a total of 621 male substance users were included in the analyses. The mean age of the participants was 34.41 (± 10.10 SD) years with a range of 17–70 years, and a majority (475; 76.5%) of them were younger than 40 years. Regarding their marital status, the majority (528, 85.0%) of them were married. About 11.1% (69) of the participants have lived abroad in the past ten years. Data on participants’ educational attainment and employment status are summarized in Table 1.
 |
Table 1 Socio-Demographic Characteristics of the Study Participants (N=621) |
The mean age at first substance use was 23.01 (± 5.89 SD) years, with 82.4% (512) reporting hashish as an initiation to substance use. About half (331, 53.3%) of the substance users in our sample reported daily substance use prior to their treatment. The most common reasons for substance use were friend offers (303, 48.8%) and family disputes (112, 18%). Almost all (99%, 615) participants had made unsuccessful attempts to quit substance use in the past. The top three reasons for relapse to substance use were peer pressure (58.8%), economic problems (18.4%), and lack of social support (14.0%). Table 2 portrays the detailed characteristics of the participants about their substance use behaviors.
 |
Table 2 Substance Use and Addictive Behaviors of the Study Participants (N=621) |
The majority of the subjects (81.2%) perceived their physical health as either very good or fair. More than two-thirds (73.4%) rated their social support as high. Overall, 46 (7.4%) and 32 (5.2%) of the study enrollees, respectively, had a physical injury or illness and were hospitalized in the past 30 days (Table 3).
 |
Table 3 Health and Other Related Characteristics of the Study Participants (N=621) |
Of all participants, 541 (87.1%) had symptoms of depression, 569 (91.6%) of anxiety, and 442 (71.2%) of stress. The prevalence of severe depression, anxiety, and stress was 34.8%, 65.8%, and 27.3%, respectively (Figure 1).
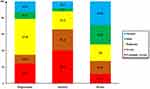 |
Figure 1 Depression, anxiety, and stress levels in people with substance use disorders treated in locally assigned treatment facilities in Kandahar, Afghanistan, 2022. |
Factors Associated with Psychological Symptoms in People with Substance Use Disorders
The results in Table 3 portray the multiple linear regressions. The multiple linear regression showed that several attributes of people with substance use disorders [ie, having a low level of education (β=0.12, p=<0.001), being unemployed (β=0.31, p=<0.001), having a low level of social support (β=−0.35, p=<0.001), had a pre-existing medical condition (β=−0.28, p=<0.001), and having lived abroad in the past ten years (β=0.10, p=0.001)] were significantly associated with higher DASS-21 total scores (Table 4).
 |
Table 4 Multivariable Regression Analysis on DAS-21 Total Scores in People with Substance Use Disorders |
Discussion
This study reveals bio-psycho-social profile of people with substance use disorders treated at locally assigned treatment facilities in Kandahar, Afghanistan. Most of our subjects (81.2%) perceived their physical health as very good or fair. Notably, the majority of the participants rated their social support as high. This study portrays a high prevalence of depression, anxiety, and stress in our subjects, reflecting the necessity for mental health services. We observed that several attributes of people with substance use disorders (ie, their level of education, employment status, level of social support, history of a pre-existing medical condition, and history of living abroad in the past ten years) were highly associated with psychological symptoms.
The majority of substance users (81.2%) in this study rated their physical health either as very good or fair. Parallel studies conducted on substance users in diverse developing countries show mixed results on the physical health of people with substance use disorders.11,13 We argue that our participants may have adjusted their responses and made the responses appropriate for the interview setting. From a more realistic standpoint, however, a lack of bio-psycho-social support programs, financial restraints, and an increased risk for sexually transmittable infections, including HIV and HCV are hypothesized to be the crucial underlying factors that may have led to a poor physical health in our sample.13
Our findings indicate that hashish (82.4%) is commonly used as a starting point for individuals who later develop substance use disorders. Moreover, our results support the findings of pertinent literature that social factors, such as peer influence and family conflict, play a significant role in the development of substance use disorders.18,19
In the present study, the DASS-21 scale has been used to screen the existence of depression, anxiety, and stress in our subjects. The high levels of depression, anxiety, and stress are illustrated in Figure 1, with notably higher rates of psychological symptoms than that reported in other studies from developing countries.11,13,20 A limited number of rehabilitation facilities in terms of infrastructure and personnel, the exceptional severity and lengthy duration of warfare, social discrimination and marginalization, unemployment, poverty, and illiteracy in this geography are some of the factors that may have brought about such a staggering level of psychological symptoms. Therefore, the provision of mental health services for this population is of paramount importance.
Our results epitomize the difference in psychological symptoms based on the participants’ educational attainment. A significantly higher number (357; 57.1%) of people with substance use disorders with a low level of education were more susceptible to psychological symptoms than their educated counterparts. This finding, reported in the literature, may somehow signify the difficulty in accessing care, poor resilience capability, limited access to health awareness programs, and other sociocultural impediments in populations with a low level of education.11,21,22
Consistent with the pertinent literature, our findings indicate that psychological symptoms were higher in respondents who were unemployed than those who were employed. This result is supported by other studies revealing that unemployed individuals are more likely to report psychological symptoms.11,23 This finding may elucidate additional stressors, such as severe financial hardship and poverty, debt, boredom, homelessness, and the loss of confidence and self-esteem that people with substance use disorders may have to endure.23 Thus, government and health authorities should develop appropriate intervention strategies and policy guidelines to protect and preserve the psychological health of those susceptible to psychological symptoms.
A great deal of evidence has shown that low social support markedly increased the rate of psychological symptoms.11,23,24 Notably, we have found that people with substance use disorders with low social support were more likely to report higher rates of psychological symptoms than their counterparts with high social support. The higher levels of depression, anxiety, and stress in people with substance use disorders having low social support have been attributed to the impeded social interactions on the family and societal levels that may have been quite stressful. Considering the high rates of the psychological burden from low social support in people with substance use disorders, families and friends should provide social support and help them in lessening the bio-psycho-social problems linked to substance use.
Expectedly, and as established in previous studies, we found that the presence of a pre-existing medical condition was highly associated with psychological symptoms, including depression, anxiety, and stress.18,23 A significant body of epidemiologic studies highlights that the solo presence of medical conditions, such as cancer, Diabetes Mellitus (DM), and HIV, is associated with poor mental health.25,26 Hence, people with substance use disorders having pre-existing medical condition should be identified and treated at the earliest to circumvent additional medical conditions and their psychosocial sequelae.
Substance use is common among Afghans settled in refugee camps in neighboring countries.1,27 Additionally, we observed that people with substance use disorders having a history of living abroad in the last ten years were more likely to develop psychological symptoms than their counterparts. The ongoing multidimensional conflict and subsequent displacement crises have resulted in severe psychological trauma for many Afghans on multiple levels.
Limitations
Several limitations of this study should be considered. Firstly, this is not a detailed bio-psycho-social profile of people with substance use disorders, as we were more inclined to specific aspects of biological, social, and mental health problems. Therefore, our findings might be biased, not representing a comprehensive profile of bio-psycho-social diagnosis in our sample. Secondly, we only included people with substance use disorders who were treated for substance use. It is likely that individuals not seeking care could have substantially more severe conditions. Thirdly, this study was done in one area (Kandahar province); generalization should be made with caution. Finally, the study is also limited by a relative lack of access to reliable HIV and HCV data, which were deemed confidential and could not be disclosed.
Implications for Future Research
Future research may investigate chronic medical conditions in people with substance use disorders as well as their associations with the time span since initiation to substance use. Another venue to explore may be related to the effective role of the rehabilitation programs on their bio-psycho-social health. Furthermore, the bio-psycho-social health of people with substance use disorders not enrolled in rehabilitation programs will be an area for future research.
Conclusion
We concluded that people with substance use disorders were vulnerable to a high magnitude of bio-psycho-social problems, necessitating multilevel bio-psycho-social interventions to alleviate the burden of substance use. Moreover, with an additional emphasis on those with a low level of education, those who have lived abroad in the past ten years, are unemployed, have a low level of social support, and those with a pre-existing medical condition.
Data Sharing Statement
The primary data used to support the findings of this study are available from the corresponding author upon request.
Ethical Approval
The study was approved by the Research and Ethics Committee (REC) of Kandahar University (Letter No. 76; Dated: 15/09/2022). We followed the ethical principles outlined in the Declaration of Helsinki. Additionally, the interviewer provided every potential participant with information concerning the study objectives, benefits/risks of participation, and their right to retract from the study at any time they desire. We obtained written informed consent from every subject.
Acknowledgments
We express our gratitude to the local authorities in Kandahar. We offer special thanks to the subjects and the data collectors of this study whose contribution made this study possible.
Author Contributions
Both authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
The authors received no specific funding for this work.
Disclosure
The authors have no conflicts of interest in this work.
References
1. Mohd Saleem S, Shoib S, Dazhamyar AR, Chandradasa M. Afghanistan: decades of collective trauma, ongoing humanitarian crises, Taliban rulers, and mental health of the displaced population. Asian J Psychiatr. 2021;65:102854. doi:10.1016/j.ajp.2021.102854
2. Todd CS, Nasir A, Stanekzai MR, et al. Impact of conflict and displacement on risk behaviours amongst people who inject drugs in Kabul, Afghanistan. Int J Drug Policy. 2016;27:173–177. doi:10.1016/j.drugpo.2015.07.014
3. Bizzarri JV, Rucci P, Sbrana A, et al. Reasons for substance use and vulnerability factors in patients with substance use disorder and anxiety or mood disorders. Addict Behav. 2007;32(2):384–391. doi:10.1016/j.addbeh.2006.04.005
4. Le Moal M. Drug abuse: vulnerability and transition to addiction. Pharmacopsychiatry. 2009;42(S 01):S42–55. doi:10.1055/s-0029-1216355
5. Naseh M, Wagner EF, Abtahi Z, Potocky M, Zahedi L. Prevalence of and risk factors for substance use among Afghan refugees in Iran: an exploratory study. J Ethn Subst Abuse. 2019;20(1):34–59. doi:10.1080/15332640.2019.1571976
6. Ritchie H, Roser M. Drug use. Our world in data; 2019. Available from: https://ourworldindata.org/drug-use.
7. SGI-Global. Afghanistan national drug use survey 2015; 2015. Available from: https://colombo-plan.org/wp-content/uploads/2020/03/Afghanistan-National-Drug-Use-Survey-2015-compressed.pdf.
8. Nafeh F, Fusigboye S, Sornpaisarn B. Understanding injecting drug use in Afghanistan: a scoping review. Subst Abuse Treat Prev Policy. 2022;17(1). doi:10.1186/s13011-022-00491-1
9. Khalsa JH, Treisman G, McCance-Katz E, Tedaldi E. Medical consequences of drug abuse and co-occurring infections: research at the national institute on drug abuse. Substan Abuse. 2008;29(3):5–16. doi:10.1080/08897070802218661
10. Chen C-Y, Lin K-M. Health consequences of illegal drug use. Curr Opin Psychiatry. 2009;22(3):287–292. doi:10.1097/yco.0b013e32832a2349
11. Jones CM, McCance-Katz EF. Co-occurring substance use and mental disorders among adults with opioid use disorder. Drug Alcohol Depend. 2019;197:78–82. doi:10.1016/j.drugalcdep.2018.12.030
12. Shamsaei F, Baanavi M, Hassanian ZM, Cheraghi F. The impact of addiction on family members mental health status. Curr Drug Res Rev. 2019;11(2):129–134. doi:10.2174/2589977511666190319162901
13. Morgen K. Diagnostic issues: DSM-5 overview for substance-related disorders. Substan Use Disord Addict. 2017;56–85. doi:10.4135/9781071800485.n7
14. Lovibond PF, Lovibond SH. The structure of negative emotional states: comparison of the Depression Anxiety Stress Scales (DASS) with the beck depression and anxiety inventories. Behav Res Ther. 1995;33(3):335–343. doi:10.1016/0005-7967(94)00075-u
15. Beaufort IN, De Weert-Van Oene GH, Buwalda VAJ, de Leeuw JRJ, Goudriaan AE. The Depression, Anxiety and Stress Scale (DASS-21) as a screener for depression in substance use disorder inpatients: a pilot study. Eur Addict Res. 2017;23(5):260–268. doi:10.1159/000485182
16. Cattell RB. The scree test for the number of factors. Multivariate Behav Res. 1966;1(2):245–276. doi:10.1207/s15327906mbr0102_10
17. International Business Machines Corporation. IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY, USA: IBM Corporation; 2012.
18. Branstetter SA, Low S, Furman W. The influence of parents and friends on adolescent substance use: a multidimensional approach. J Subst Use. 2010;16(2):150–160. doi:10.3109/14659891.2010.519421
19. Barrett AE, Turner RJ. Family structure and substance use problems in adolescence and early adulthood: examining explanations for the relationship. Addiction. 2006;101(1):109–120. doi:10.1111/j.1360-0443.2005.01296.x
20. Luo D, Tan L, Shen D, et al. Characteristics of depression, anxiety, impulsivity, and aggression among various types of drug users and factors for developing severe depression: a cross-sectional study. BMC Psychiatry. 2022;22(1):1. doi:10.1186/s12888-022-03933-z
21. Goldstick JE, Bohnert KM, Davis AK, et al. Dual trajectories of depression/anxiety symptoms and alcohol use, and their implications for violence outcomes among drug-using urban youth. Alcohol Alcohol. 2018. doi:10.1093/alcalc/agy036
22. Lincoln A, Paasche-Orlow MK, Cheng DM, et al. Impact of health literacy on depressive symptoms and mental health-related quality of life among adults with addiction. J Gen Intern Med. 2006;21(8):818–822. doi:10.1111/j.1525-1497.2006.00533.x
23. Mokona H, Yohannes K, Ayano G. Youth unemployment and mental health: prevalence and associated factors of depression among unemployed young adults in Gedeo zone, Southern Ethiopia. Int J Ment Health Syst. 2020;14. doi:10.21203/rs.2.22998/v3
24. Dobkin PL, Civita MD, Paraherakis A, Gill K. The role of functional social support in treatment retention and outcomes among outpatient adult substance abusers. Addiction. 2002;97(3):347–356. doi:10.1046/j.1360-0443.2002.00083.x
25. Kravitz RL, Ford DE. Introduction: chronic medical conditions and depression—the view from primary care. Am J Med. 2008;121(11):S1–7. doi:10.1016/j.amjmed.2008.09.007
26. Lotfaliany M, Bowe SJ, Kowal P, Orellana L, Berk M, Mohebbi M. Depression and chronic diseases: co-occurrence and communality of risk factors. J Affect Disord. 2018;241:461–468. doi:10.1016/j.jad.2018.08.011
27. Deilamizade A, Moghanibashi-Mansourieh A, Mohammadian A, Puyan D. The sources of stigma and the impacts on Afghan refugees with substance abuse disorders: a qualitative study in Iran. J Ethn Subst Abuse. 2019;19(4):610–622. doi:10.1080/15332640.2018.1556764
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
