Back to Journals » International Medical Case Reports Journal » Volume 16
Bilateral Posterior Ischemic Optic Neuropathy Due to Bilateral Anterior-Drainage Dural Carotid-Cavernous Fistulas: A Case Report
Authors Thammakumpee K, Padungkiatsagul T , Putthirangsiwong B, Chokthaweesak W , Jindahra P, Kobkitsuksakul C , Vanikieti K
Received 13 December 2022
Accepted for publication 16 January 2023
Published 24 January 2023 Volume 2023:16 Pages 53—57
DOI https://doi.org/10.2147/IMCRJ.S401291
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Kanyarat Thammakumpee,1 Tanyatuth Padungkiatsagul,1 Bunyada Putthirangsiwong,1 Weerawan Chokthaweesak,1 Panitha Jindahra,2 Chai Kobkitsuksakul,3 Kavin Vanikieti1
1Department of Ophthalmology, Faculty of Medicine Ramathibodi Hospital, Mahidol University, Bangkok, Thailand; 2Department of Medicine, Faculty of Medicine Ramathibodi Hospital, Mahidol University, Bangkok, Thailand; 3Department of Radiology, Faculty of Medicine Ramathibodi Hospital, Mahidol University, Bangkok, Thailand
Correspondence: Kavin Vanikieti, Department of Ophthalmology, Faculty of Medicine Ramathibodi Hospital, Mahidol University, 270 Rama VI Road, Bangkok, 10400, Thailand, Tel +662 201 1526, Email [email protected]
Purpose: To report a case of bilateral posterior ischemic optic neuropathy (PION) due to bilateral anterior-drainage dural carotid-cavernous fistulas (CCFs).
Case Description: We report on a 62-year-old woman with a history of poorly controlled hypertension who presented with sudden bilateral visual loss and headache for 5 days. She denied a history of head trauma. On examination, her visual acuities were no light perception (NLP) with fixed pupils in both eyes. The ocular motility of both eyes was limited in all directions. Both eyelids were difficult to open. Anterior segment examination revealed bilateral chemosis and episcleral corkscrew vessels. Intraocular pressures were 45 and 48 mmHg in her right and left eyes, respectively. Gonioscopy revealed blood in Schlemm’s canal at the nasal angle of the right eye. Fundus examination showed slightly dilated and tortuous retinal veins with normal-appearing optic discs in both eyes. The cup-to-disc ratios were 0.3 bilaterally. Other neurological examinations were unremarkable. Magnetic resonance imaging demonstrated dilation of the bilateral superior ophthalmic veins (SOVs), and marked orbital and periorbital congestion bilaterally. However, there was no compression or stretching of the bilateral optic nerves. Diffusion restriction on diffusion-weighted imaging, with corresponding reduced apparent diffusion coefficient, in the entire bilateral orbital segment of the optic nerves was revealed, consistent with bilateral PION. Magnetic resonance angiography revealed arterialization of the bilateral cavernous sinuses and SOVs. Cerebral angiography confirmed the diagnosis of bilateral anterior-drainage dural CCFs. Treatment with transvenous coil embolization was successful. Three months after embolization, ophthalmic examination demonstrated progressive improvement of aforementioned ophthalmic signs; however, her visual acuities remained NLP in both eyes.
Conclusion: To our knowledge, this is the first reported case of bilateral PION due to bilateral anterior-drainage dural CCFs. In spite of its rarity, PION should be considered as a severe, irreversible ophthalmic complication of anterior-drainage dural CCF.
Keywords: dural carotid-cavernous fistula, posterior ischemic optic neuropathy, anterior drainage, bilateral, complications
Introduction
A dural carotid-cavernous fistula (CCF) is a low-flow fistula with communication between the cavernous sinus and dural branches of the internal carotid artery (ICA) and/or external carotid artery (ECA).1,2 Clinical symptoms include conjunctival injection, chemosis, proptosis, binocular diplopia, retroorbital pain and subjective bruits.3 Several ophthalmic complications associated with dural CCF have been reported, including optic neuropathies. The major etiologies of dural CCF-related optic neuropathies are glaucomatous optic nerve damage and compressive/stretching of the optic nerve.4 Posterior ischemic optic neuropathy (PION) has rarely been reported as an ophthalmic complication of dural CCF. Herein, we report a case of bilateral PION due to bilateral anterior-drainage dural CCFs.
Case Description
A 62-year-old Thai woman presented with sudden bilateral visual loss and headache for 5 days. She denied a history of head trauma. Her medical history was significant for poorly controlled hypertension.
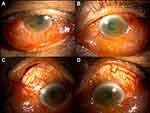
Vital signs were normal except for blood pressure of 200/105 mmHg. Visual acuity was no light perception (NLP) with fixed pupils in both eyes. The ocular motility of both eyes was limited in all directions. Both eyelids were difficult to open. Hertel exophthalmometer measurements were 16 mm in the right eye and 14 mm in the left eye. There were significant chemosis and episcleral corkscrew vessels in both eyes (Figure 1). Both corneas showed mild, diffuse stromal edema without any infiltration. The anterior chambers were deep and quiet in both eyes. Intraocular pressures were 45 mmHg and 48 mmHg in the right and left eyes, respectively. Gonioscopy revealed blood in Schlemm’s canal at the nasal angle of the right eye. Fundus examination showed slightly dilated and tortuous retinal veins with normal-appearing optic discs in both eyes. The cup-to-disc ratio was 0.3 bilaterally. Optical coherence tomography demonstrated normal thickness of the macula in each eye (Figure 2). There was no audible bruit. Other neurological examinations were unremarkable.
 |
Figure 2 Optical coherence tomography of the macula at presentation demonstrating normal thickness in the right (A) and left (B) eyes. |
Magnetic resonance imaging (MRI) with gadolinium of the brain and orbits demonstrated dilation of the bilateral superior ophthalmic veins (SOVs) and a marked degree of orbital and periorbital congestion bilaterally. However, neither compression nor stretching of the bilateral optic nerves was observed. Interestingly, diffusion restriction, with corresponding reduction of the apparent diffusion coefficient (ADC), in the entire orbital segment of the optic nerves bilaterally was revealed on diffusion-weighted imaging (DWI). That is consistent with bilateral PION (Figures 3A and B). Magnetic resonance angiography (MRA) of the brain and orbits revealed arterialization of the bilateral cavernous sinuses and SOVs (Figures 3C and D).
Cerebral angiography confirmed the diagnosis of bilateral anterior-drainage dural CCFs. The right dural CCF was fed by the dural branches of the ICA (right meningohypophyseal trunk, Figure 4A). The left dural CCF was fed by the dural branches of the ECA (left-middle meningeal artery and the left artery of the foramen rotundum, Figure 4B) and the dural branches of the ICA (left meningohypophyseal trunk). Each side of the dural CCF contributed arterial blood flow into the bilateral SOVs (contralateral SOV through inter-cavernous communication, Figures 4A and B). No cortical venous reflux of arterial blood flow was noted. Based on these findings, transvenous coil embolization was performed. The bilateral cavernous sinuses were embolized using coils to occlude the feeding vessels from the dural branches of both the ICA and ECA. Immediate post-embolization cerebral angiography showed complete closure of the fistulas.
Three months after embolization, ophthalmic examination demonstrated progressive improvement of the aforementioned ophthalmic signs; however, the patient’s visual acuities remained NLP in both eyes.
Discussion
Damage to the optic nerve(s) in dural CCF is usually the result of a glaucomatous or compressive/stretching optic neuropathy.4 In our patient, although the intraocular pressure in both eyes was extremely high, glaucomatous optic neuropathy was unlikely to have caused the patient’s visual loss, as the cup-to-disc ratio was 0.3 bilaterally. Although our patient demonstrated substantial bilateral orbital and periorbital congestion clinically and radiographically, neither compression nor stretching of her bilateral optic nerves was visible on MRI. This suggests that mechanical optic neuropathies were unlikely to be the cause of visual loss in this patient. In our patient, the diagnosis of bilateral PION was confirmed based on DWI and ADC maps that showed diffusion restriction and reduced ADC, respectively, bilaterally throughout the orbital segment of the optic nerves. This finding has previously been described in PION.5,6 PION usually presents acutely as severe loss of vision.7,8 It is distinguished from anterior ischemic optic neuropathy by the lack of optic disc edema.
Dural CCF-related PION is extremely uncommon. To our knowledge, there are only two reported cases of PION as an ophthalmic complication of dural CCF.9,10 Hashimoto et al described a case of presumed unilateral PION in an ipsilateral posterior-drainage dural CCF, which was fed by dural branches from the ICA and ECA; however, no DWI and ADC maps for confirmation of the PION were undertaken.9 Recently, Hoang et al reported a case of unilateral posterior-drainage dural CCF (fed by dural branches from the ICA and ECA) with ipsilateral PION.10 The authors of both studies hypothesized that the PION was caused by arterial steal in the setting of posterior-drainage dural CCF, which shifted the arterial blood flow from the orbital to intracranial direction. In contrast, the dural CCFs in our patient involved the anterior drainage, which was confirmed on cerebral angiography. Therefore, we hypothesize that ischemia in both optic nerves could have been the consequence of orbital venous hypertension, which led to the reduction of arterial blood flow (hypoperfusion) in the ophthalmic artery branches, rather than having been the consequence of the “arterial steal” phenomenon.
The visual prognosis in cases of PION is typically poor and irreversible;7,8 despite the complete closure of the bilateral dural CCFs and progressive improvement in the presenting ophthalmic signs, our patient’s visual acuities remained NLP in both eyes at the 3-month follow-up.
To our knowledge, this is the first reported case of bilateral PION due to bilateral anterior-drainage dural CCFs. Despite its rarity, PION should be considered as a severe, irreversible ophthalmic complication of anterior-drainage dural CCF.
Ethical Approval and Consent for Publication
Institutional Review board (IRB) approval for this study was not required. The patient gave her consent for the publication of information related to her medical condition.
Acknowledgments
We thank Yanin Suwan, MD, Department of Ophthalmology, Faculty of Medicine Ramathibodi Hospital, Mahidol University, Bangkok, Thailand, for her assistance on the photography for Figure 1. We thank Claire Barnes, PhD, from Edanz (https://jp.edanz.com/ac) for editing a draft of this manuscript.
Funding
There is no funding to report.
Disclosure
The authors declare that they have no competing interests for this study.
References
1. Ke L, Yang YN, Yuan J. Bilateral carotid-cavernous fistula with spontaneous resolution: a case report and literature review. Medicine. 2017;96:e6869. doi:10.1097/MD.0000000000006869
2. Henderson AD, Miller NR. Carotid-cavernous fistula: current concepts in aetiology, investigation, and management. Eye. 2018;32:164–172. doi:10.1038/eye.2017.240
3. Newton TH, Hoyt WE. Dural arteriovenous shunts in the region of the cavernous sinus. Neuroradiology. 1970;1:71–81. doi:10.1007/BF00389438
4. Tan AC, Farooqui S, Li X, et al. Ocular manifestations and the clinical course of carotid cavernous sinus fistulas in Asian patients. Orbit. 2014;33:45–51. doi:10.3109/01676830.2013.851253
5. Mathur S, Karimi A, Mafee MF. Acute optic nerve infarction demonstrated by diffusion-weighted imaging in a case of rhinocerebral mucormycosis. AJNR Am J Neuroradiol. 2007;28:489–490.
6. Bodanapally UK, Shanmuganathan K, Shin RK, et al. Hyperintense optic nerve due to diffusion restriction: diffusion-weighted imaging in traumatic optic neuropathy. AJNR Am J Neuroradiol. 2015;36:1536–1541. doi:10.3174/ajnr.A4290
7. Hayreh SS. Posterior ischaemic optic neuropathy: clinical features, pathogenesis, and management. Eye. 2004;18:1188–1206. doi:10.1038/sj.eye.6701562
8. Hayreh SS. Ischemic optic neuropathy. Prog Retin Eye Res. 2009;28:34–62. doi:10.1016/j.preteyeres.2008.11.002
9. Hashimoto M, Ohtsuka K, Suzuki Y, Hoyt WF. A case of posterior ischemic optic neuropathy in a posterior-draining dural cavernous sinus fistula. J Neuroophthalmol. 2005;25:176–179. doi:10.1097/01.wno.0000177297.60092.f6
10. Hoang TT, Nguyen CN, Ha TTH, Subramanian PS. A lesson learnt from a dural carotid cavernous fistula-induced superior ophthalmic vein occlusion with posterior ischaemic optic neuropathy. Neuroophthalmology. 2021;46:199–202. doi:10.1080/01658107.2021.2000622
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.