Back to Journals » Journal of Pain Research » Volume 12
Bidirectional alterations in ALFF across slow-5 and slow-4 frequencies in the brains of postherpetic neuralgia patients
Authors Gu L, Hong S, Jiang J, Liu J, Cao X, Huang Q, Zeng X , Zhou F , Zhang D
Received 4 July 2018
Accepted for publication 9 November 2018
Published 18 December 2018 Volume 2019:12 Pages 39—47
DOI https://doi.org/10.2147/JPR.S179077
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor E Alfonso Romero-Sandoval
Lili Gu,1,* Shunda Hong,2,* Jian Jiang,2 Jiaqi Liu,2 Xintian Cao,1 Qing Huang,2 Xianjun Zeng,2 Fuqing Zhou,2 Daying Zhang1
1Department of Pain, The First Affiliated Hospital, Nanchang University, Nanchang, Jiangxi, People’s Republic of China 2Department of Radiology, The First Affiliated Hospital, Nanchang University, Nanchang, Jiangxi, People’s Republic of China
*These authors contributed equally to this work
Purpose: Postherpetic neuralgia (PHN) detrimentally affects brain function. Recent studies have suggested that frequency-dependent changes in electroencephalography in chronic pain patients and blood oxygenation level dependent (BOLD) fluctuations can reflect neuronal activity in different frequencies. The current study aimed to investigate PHN-related brain oscillatory activity in a specific frequency band by using the amplitude of low-frequency fluctuation (ALFF) method.
Materials and methods: ALFF changes were analyzed across different frequencies (slow-4 band: 0.027–0.073 Hz; slow-5 band: 0.01–0.027 Hz; and typical band: 0.01–0.08 Hz) in the brains of PHN patients and compared with those in the brains of healthy controls (HCs) during resting-state fMRI. Eighteen HCs and PHN patients underwent fMRI scanning.
Results: In the typical band, compared with HCs, PHN patients showed prominently decreased ALFF in the right prefrontal cortex (Brodmann area 10/46) and increased ALFF in the bilateral brain stem/cerebellum anterior lobe (BS/CAL). In the slow-4 band, PHN patients exhibited significantly decreased ALFF in the bilateral cuneus/lingual gyrus and the right prefrontal cortex. In the slow-5 band, PHN patients presented significantly increased ALFF in the bilateral BS/CAL and left parieto-occipital cortex. Moreover, the increased ALFF in the left parieto-occipital cortex in the slow-5 band was positively correlated with VAS scores (P=0.022), and the increased ALFF in the bilateral BS/CAL in the slow-5 band was positively correlated with disease duration (P=0.020).
Conclusion: Our results suggested that the intrinsic brain activity of PHN patients was abnormal and frequency dependent, especially the bidirectional alteration in ALFF across the slow-4 and slow-5 frequencies in the brains of PHN patients.
Keywords: amplitude of low-frequency fluctuation, postherpetic neuralgia, functional magnetic resonance imaging, resting state, pain
Introduction
Postherpetic neuralgia (PHN) is a chronic neuropathic pain syndrome usually defined as persistent pain for >3 months after shingles skin lesions heal.1 This sharp PHN pain may affect patients physically and psychologically and may impact their social life.2
Cerebral structural and functional alterations in PHN have been demonstrated by several neuroimaging techniques. For example, microstructural alterations in the pain matrix (thalamus, insula, cerebellum, parietal, and prefrontal cortex) and regions in charge of pain modulation (prefrontal–limbic–brain stem areas), emotional activity, and affective processes have been observed.3,4 Functional alterations in PHN patients include regions involved in affective responses, sensory discrimination (primary and secondary somatosensory, anterior cingulate cortices, insula, thalamus), emotion, and reward (orbital frontal cortex, amygdala, ventral striatum).5–7 In addition, cerebral blood flow is increased in the inferior parietal lobule, amygdala, S1 area, thalamus, insula, and striatum but decreased in the frontal cortex.8 An interhemispheric intrinsic connective study showed decreased homotopic connectivity in the posterior cingulate cortex, dorsolateral prefrontal cortex, and precuneus (PCUN),9 indicating decreased functional integration.
In a recent neuroimaging study of chronic pain, oscillation frequency changes were detected by electrophysiology. Sarnthein et al and Stern et al10,11 reported frequency (theta and beta bands)-related increases in the anterior cingulate, prefrontal, and somatosensory cortices in chronic neuropathic pain patients. Fallon et al12 also found frequency (theta band)-related increases in the prefrontal and anterior cingulate cortices in fibromyalgia syndrome patients by using electroencephalography. Enhanced activity has been observed in low-frequency spectral power of resting brain electroencephalography in paraplegic neuropathic pain patients13 and spinal cord injury patients with chronic pain.14 Moreover, abnormal amplitude of low-frequency fluctuation (ALFF) values have been reported in the pain matrix, brain stem, limbic system, and regions involved in affective and emotional activity in PHN patients.15,16 Although alterations in ALFF were observed in PHN, specific frequency bands within the low-frequency oscillation (by ALFF quantitative analysis) range may contribute differentially to changes in patients with PHN. In fact, ALFF values in the slow-4 band (0.027–0.073 Hz) were most powerful in the basal ganglia.17 Various neuropsychiatric diseases exhibit frequency-dependent changes in ALFF values; for example, alterations in the middle frontal gyrus and the cerebellum in the slow-5 band were greater than those in the slow-4 band in Wilson’s disease.18 Moreover, altered intrinsic functional connectivity strength was observed in several regions in both the slow-4 and slow-5 bands in amyotrophic lateral sclerosis.19
In this study, we hypothesized that altered brain oscillatory activity in distinct low-frequency bands is related to clinical variables and may provide meaningful information regarding the brain in PHN. Accordingly, we used ALFF to examine the changes in brain oscillatory activity in different low-frequency bands (slow-4 band: 0.027–0.073 Hz; slow-5 band: 0.01–0.027 Hz; and typical band: 0.01–0.08 Hz) between PHN patients and healthy controls (HCs).
Materials and methods
Participants
Data were obtained from 18 right-handed PHN patients from the First Affiliated Hospital of Nanchang University. Clinical diagnosis was made by two pain specialists according to the International Association for the Study of Pain (IASP) criteria.20 The age of PHN patients ranged from 46 to 72 years. All patients underwent the VAS evaluation for pain intensity prior to undergoing MRI scanning. All the recruited patients experienced pain with VAS scores ≥5. The mean disease duration was 116.78±25.96 days, which was calculated from disease onset to the date of MRI examination. All patients with other pain disorders were excluded, and none of the included patients had a history of any other major psychiatric illness, neurological illness, head injury, or alcohol and drug abuse. Using advertisements posted in the department bulletin board, we recruited 18 right-handed HCs who were age- and sex-matched with the PHN patients. The age of the HCs ranged from 45 to 70 years. No HCs had any pain disorders, genetic diseases, neurological or psychiatric disorders, or history of substance abuse. Those who had a history of head injury were also excluded.
All participants and participants’ guardians signed a written informed consent form prior to data acquisition. The present study was conducted according to approved guidelines and in compliance with the principles of the Declaration of Helsinki. The study was also approved by the Medical Research Ethics Committee and the Institutional Review Board of The First Affiliated Hospital of Nanchang University.
MRI acquisition
MRI scanning was performed on a 3.0-Tesla Siemens Trio TIM Scanner (Siemens Medical Solutions, Erlangen, Germany) at the Radiology Department, the First Affiliated Hospital of Nanchang University. Each participant underwent a conventional T1-weighted and T2-weighted MRI scan, a resting-state functional magnetic resonance imaging (rs-fMRI) scan and a three-dimensional, high-resolution T1-weighted structural MRI scan. First, conventional T1-weighted imaging (repetition time [TR]=250 ms, TE=2.46 ms, slices = 19, slice thickness = 5 mm, gap = 1.5 mm, and field of view [FOV]=220×220 mm) and T2-weighted imaging (TR=4,000 ms, TE=113 ms, slices = 19, slice thickness = 5 mm, gap = 1.5 mm, and FOV=220×220 mm) were performed. Then, rs-fMRI data were obtained using an echo planar imaging sequence (TR=2,000 ms, TE=30 ms, flip angle = 90°, FOV=220×220 mm, matrix = 64×64, 4 mm slice thickness, 30 interleaved axial slices, 240 acquisitions). The high-resolution anatomic three-dimensional T1 sequence had the following parameters: TR=1900 ms, TE=2.26 ms, flip angle=9°, FOV=215×230 mm, matrix = 240×256, slice thickness = 1.0 mm, 176 sagittal slices. For the resting-state scan, all participants were instructed to keep their eyes closed, clear their minds, and remain awake.
MRI data preprocessing
Conventional T1-weighted imaging and T2-weighted imaging were performed to rule out structural brain lesions before preprocessing. rs-fMRI images and structural images were preprocessed using a toolbox for Data Processing and Analysis of Brain Imaging21 (DPABI) (http://rfmri.org/dpabi) running on Matlab 7.14.0 (MathWorks, Natick, MA, USA). Preprocessing comprised the following steps: 1) rejection of the first ten functional volumes for stabilization; 2) slice-timing correction; 3) head motion correction; 4) linear transformation: coregistration of the high-resolution structural images to the mean functional image; 5) spatial normalization to the Montreal Neurological Institute template and resampling to 3×3×3 mm voxels; 6) linear detrending and nuisance signal removal, including white matter, cerebrospinal fluid, Friston 24-parameter, and global signal as covariates. In this study, four participants were excluded according to the head motion criteria, which included a maximum spin (x, y, z) of <3.0° and a maximum cardinal direction displacement (x, y, z) of <3.0 mm; the group differences in head motion between PHN patients (n=18) and HCs (n=18) were evaluated according to framewise displacement (FD) criteria based on the method of van Dijk et al.22
ALFF analysis
ALFF was calculated using DPABI (http://rfmri.org/dpabi). First, fast Fourier transformation was used to convert the time series to the frequency domain for each voxel. Second, the square root of the power spectrum was calculated. Third, the square root was averaged across a predefined frequency interval, and ALFF was calculated as the averaged square root in a voxel. Finally, the ALFF of each voxel was divided by the global mean value to reduce the global effects of variability across participants.23
ALFF is an effective method for estimating the absolute strength or intensity of low-frequency fluctuations. To investigate PHN-related brain oscillatory activity, we calculated the ALFF for the typical frequency band (0.01–0.08 Hz), the slow-4 band (0.027–0.073 Hz), and the slow-5 band (0.01–0.027 Hz).
Statistical analysis
First, we used Student’s t-tests to analyze the effects of head motion in ALFF analysis of rs-fMRI, and mean FD was applied as a covariate in the group comparisons of the ALFF.24
Then, two-sample t-tests were performed to examine differences between the groups in the typical frequency band (0.01–0.08 Hz). Next, to analyze the main effects of group, frequency band, and their interaction, a two-way ANOVA with factors of condition (PHN, HCs) and frequency band (slow-4, slow-5) was performed. Finally, post hoc tests were performed to determine the regional group differences in ALFF. Age, gender, and FD values were used as covariates, and the significance threshold correction was based on the Gaussian random field theory with a voxel-level P<0.025 and cluster-level P<0.05.
Brain–clinical variable relationship
For correlational analyses between the ALFF values of group-difference regions and clinical variables in PHN patients, Pearson’s correlation coefficients were calculated with a significance level of P<0.05.
Results
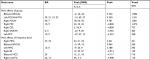
Demographic and clinical characteristics
Demographic and clinical information are listed in Table 1. No significant differences in age, sex, and FD were observed between the two groups. In this study, PHN patients reported a mean VAS score of 6.61±1.47, indicating a moderate-high intensity of pain before MRI scanning (0 indicates no pain and 10 indicates the highest unbearable pain).
  | Table 1 Participant information Notes: FDvox is the voxel-specific frame wise displacement for in-scanner head motion. **P<0.01. Abbreviations: HCs, healthy controls; PHN, postherpetic neuralgia. |
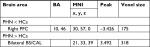
ALFF analysis of the typical frequency band (0.01–0.08 Hz)
The ALFF results revealed significantly higher ALFF values in the typical frequency band (0.01–0.08 Hz) than the global average in the PHN and HC groups, as shown in Figure 1. Next, we compared these ALFF patterns between the two groups and found a significant decrease in ALFF values in the right prefrontal cortex (PFC, Brodmann area 10/46) in PHN patients. In contrast, ALFF values were significantly increased in the bilateral brain stem/cerebellum anterior lobe (BS/CAL) in the PHN group (Figure 1; Table 2).
ALFF changes in different frequency bands
The main effects from the two-way repeated-measures ANOVA are shown in Figure 2A and Table 3. Brain regions with a main effect of group included significantly increased ALFF (PHN > HCs) regions in the BS/CAL, the left PCUN/superior middle temporal gyrus (sMTG), and the right PCUN and significantly decreased ALFF (PHN < HCs) regions in the right cerebellum posterior lobe (CPL), the right PFC, the left PFC, and the right supplementary motor area/M1 (SMA/M1).
Several brain regions showed a significant main effect for frequency band (Figure 2B; Table 3), including a significantly increased ALFF (slow-5 > slow-4) in the right medial frontal gyrus (MFG), the left MFG, the bilateral BS/CAL, and a significantly decreased ALFF (slow-5 < slow-4) in the right BS, the bilateral midcingulate cortex, and the right insular/superior temporal gyrus. There were no significant interactions between different groups and frequency bands (Figure 2C).
Further post hoc t-tests showed bidirectional changes in ALFF across slow-4 and slow-5 frequencies between the PHN and HC groups. Significantly decreased ALFF values were identified in the bilateral cuneus/lingual gyrus and the right PFC in the slow-4 band, but significantly increased ALFF values were identified in the bilateral BS/CAL and the left parieto-occipital cortex (POC) in the slow-5 band (Figure 3; Tables 4 and 5).
Correlations between ALFF and clinical variables in the PHN group
The ALFF values of the patients were extracted from significantly different regions between groups in different frequency (typical, slow-5, slow-4) bands to evaluate this relationship. In the PHN patients (Figure 4), increased ALFF values of the slow-5 band in the left POC were positively correlated with VAS scores (P=0.022) and increased ALFF values of the slow-5 band in the bilateral BS/CAL were positively correlated with disease duration (P=0.020). However, significant correlations were not detected between abnormal ALFF values in the slow-4 and typical bands and clinical scores (P=0.124–0.942).
Discussion
In the current study, we investigated abnormalities in PHN-related brain oscillatory activity in different frequency bands (typical, slow-4 and slow-5 bands). PHN patients exhibited decreased ALFF values in the right PFC and increased ALFF values in the BS/CAL in the typical band. Moreover, several regions exhibited significant differences in ALFF values between the slow-5 and slow-4 bands and between PHN patients and HCs. However, there was no significant interaction between frequency band and group. Interestingly, ALFF values were significantly decreased in the bilateral cuneus/lingual gyrus and the right PFC in the slow-4 band but were significantly increased in the bilateral BS/CAL and the left POC in the slow-5 band. These findings indicated bidirectional changes in ALFF values across the slow-4 and slow-5 frequencies between the PHN and HC groups. In addition, increased ALFF values in the bilateral BS/CAL and the left POC in the slow-5 band were positively correlated with disease duration and VAS scores, respectively.
Differential ALFF values between groups in the typical frequency band (0.01–0.08 Hz)
Compared with HCs, PHN patients showed significantly decreased ALFF values in the right PFC and increased ALFF values in the BS/CAL in the typical band. The PFC is the hub region of the default mode network (DMN);25 the DMN most commonly shows the highest intrinsic activity during rest, and this activity declines during some attention-demanding cognitive tasks.25,26 The reduction in intrinsic activity in the DMN may be due to the maintenance of attention in PHN pain; pain sensations conflict with the resting state of the brain, which is dominated by the DMN.27 The PFC is also a vital region in the cognitive control network28 and is involved in cognitive decision making, such as pain evaluation and response decisions.29 Therefore, the reduced activity of the PFC may be an underlying reason for the cognitive symptoms of depression in PHN patients. Other previous neuroimaging studies also suggested microstructural abnormalities,3 decreased interhemispheric intrinsic connectivity,9 and reduced ALFF values15 in the PFC in PHN patients.
In addition, we found significantly increased ALFF values in the BS/CAL; this result is consistent with a recent functional neuroimaging study showing increased regional homogeneity (ReHo) and fractional aptitude of low-frequency fluctuation (fALFF) in the brain stem and cerebellum in PHN patients.16 The cerebellum is part of the pain matrix30 and is involved in nocifensive behavior.31 Activation of the cerebellum is often reported during the processing of pain. The CAL is an important region in the cerebellum, and the CAL and BS are closely linked in structure and function. The BS is a major part of pain processing and modulation of nociceptive input; thus, the BS/CAL may be a key region involved in descending pain modulation.
Main effect of the groups and frequency bands
The main effect of the groups in ANOVA showed significant differences in ALFF values between PHN patients and HCs, including increased ALFF values (PHN > HCs) in the bilateral BS/CAL, the left PCUN/sMTG, and the right PCUN and decreased ALFF values (PHN < HCs) in the right CPL, the right PFC, the left PFC, and the right SMA/M1. Changes in ALFF values in the BS/CAL and the PFC were the same as those in the typical frequency band between groups. The PCUN/sMTG is an information processing region. The PCUN continuously gathers information from both external and internal milieu and plays vital roles in monitoring sensory information32 and implementing a wide range of higher-order cognitive functions.33 The MTG might be involved in the processing of somatosensory stimuli.34 Therefore, the increased ALFF values in the PCUN/sMTG could be explained by the increases in spontaneous neuronal activity in the information processing regions, which show functional compensation or plasticity. The CPL plays an important role in pain regulation.35 Cerebellar areas are activated by painful stimulation in chronic neuropathic pain patients.35,36 Nociception may induce activation of the CPL in PHN patients. Moreover, the SMA is part of the pain matrix,15 which is involved in motor responses to pain. In the past, researchers have reported that pain-related regions (SMA/M1,37 cerebellum,38 S1,39 and S240) play a vital role in sensorimotor control, and increased functional connectivity in the SMA has been reported in chronic low back pain patients.41
In addition, the main effect of frequency band revealed increased ALFF (slow-5 > slow-4) in the MFG, the left MFG, and the bilateral BS/CAL and significantly decreased ALFF (slow-5 < slow-4) in the right BS, the bilateral midcingulate cortex, and the right insular/superior temporal gyrus. Different neurophysiological mechanisms induce different oscillatory bands and have varying physiological functions.42 Our results are similar to previous rs-fMRI studies, showing that the lower frequency band has higher power in the prefrontal, occipital, and parietal cortices. The higher frequency band has lower power in subcortical structures, including the thalamus and the basal ganglia.42 The ventromedial prefrontal cortices in the slow-5 band are more dominant than those in the slow-4 band.17
Frequency-dependent alterations in ALFF in PHN patients
Interestingly, we found bidirectional alterations in ALFF values across slow-4 and slow-5 frequency bands between the PHN and HC groups, which represent a novel discovery regarding frequency-dependent alterations in PHN patients. We observed significantly decreased ALFF values in the bilateral cuneus/lingual gyrus and the right PFC in the slow-4 band but significantly increased ALFF values in the bilateral BS/CAL and the left POC in the slow-5 band. Decreased ALFF values in the right PFC and increased ALFF values in the bilateral BS/CAL were consistent with the results of the typical frequency band; combined with the slow-4 and slow-5 bands, these values may be more sensitive for detecting alterations in spontaneous brain activity in PHN patients. However, this idea requires further study. Moreover, increased ALFF values in the slow-5 band in the left POC were positively correlated with VAS scores. The POC may be involved in the integration of visual information and somatosensory signals;43 additionally, the POC is activated in response to the prickle sensation induced by cold stimuli.44 Thus, we suggest that increased neuronal activity in the POC in the slow-5 band may indicate that patients were enduring sharp pain, and pain intensity may play a dominating role. In addition, increased ALFF values in the slow-5 band in the bilateral BS/CAL were positively correlated with disease duration. The BS/CAL is a pain processing and modulation region; long-term PHN pain may aggravate pain processing and modulation in the BS/CAL and may induce spontaneous neuronal activity.
Limitations
Several limitations should be noted. First, the sample size was limited, and the pain duration (mean 116.78 days) was relatively short in the present study. Cao et al reported increased ReHo and fALFF values in the cerebellum, pons, frontal lobe thalamus, insula, putamen, PCUN, and midbrain and decreased ReHo and fALFF values in the limbic system, temporal lobe, occipital lobe, and parietal lobe in PHN brains (mean 12.2 months).16 Comparing the results of this former study and our present study, fewer abnormal regions were found in PHN brains (mean 116.78 days) in the present study. We speculate that pain duration may be an important cause. Thus, a larger sample and a longer period for monitoring pain should be incorporated in future studies to increase the reliability of the results. Second, although medication may not have affected our results, we cannot completely exclude effects of medication. Comparing brain activity before and after pharmacological treatment in PHN patients may be interesting in further studies. Third, all patients have different degrees of dermatome involvement. Although no studies have evaluated the impact of the distribution of skin lesions on the brain in PHN patients, differences in the affected areas may potentially lead to differences in the brain. These concepts need further exploration. Finally, although no patients in the present study had depression or anxiety, many studies have reported that PHN is associated with depression and anxiety,45 which may influence neural activity. However, our study lacked a cognitive and emotional evaluation. Correlations between cognitive abilities and neural activity should be investigated in future studies.
Conclusion
In the current study, we detected abnormalities in brain oscillatory activity in PHN patients in the pain matrix, the DMN, and information processing and modulation regions. Moreover, bidirectional alterations were found in ALFF values across the slow-4 and slow-5 frequencies in the brains of PHN patients; thus, the slow-4 and slow-5 frequency bands could reflect the spontaneous brain activity of PHN from different perspectives. These findings illuminate alterations in PHN-related frequency-dependent changes in ALFF and provide new insights into the pathophysiology of PHN.
Acknowledgments
This work was supported by grants from the Jiangxi Province Health Department Support Program (grant nos. 20181057 and 2017A026) and the Jiangxi Province Education Department Support Program (grant no. GJJ170075).
Author contributions
LG, SH, DZ, and FZ designed the study. LG, SH, JJ, JL, XC, and QH acquired the data. LG, SH, FZ, and JJ processed the neuroimaging data. DZ and FZ performed the statistical analyses. LG, SH, DZ, FZ, JL, QH, JJ, XC, and XZ wrote the initial draft. All authors contributed to data analysis, drafting and revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
Shingles KGM. Herpes zoster vaccine (Zostavax®): a review in the prevention of herpes zoster and postherpetic neuralgia. BioDrugs. 2016;30:1–12. | ||
Drolet M, Brisson M, Schmader KE, et al. The impact of herpes zoster and postherpetic neuralgia on health-related quality of life: a prospective study. CMAJ. 2010;182(16):1731–1736. | ||
Zhang Y, Yu T, Qin B, Li Y, Song G, Yu B. Microstructural abnormalities in gray matter of patients with postherpetic neuralgia: a diffusional kurtosis imaging study. Pain Physician. 2016;19(4):E601–E611. | ||
Chen F, Chen F, Shang Z, et al. White matter microstructure degenerates in patients with postherpetic neuralgia. Neurosci Lett. 2017;656:152–157. | ||
Geha PY, Baliki MN, Wang X, et al. Brain dynamics for perception of tactile allodynia (touch-induced pain) in postherpetic neuralgia. Pain. 2008;138(3):641–656. | ||
Zhang Y, Liu J, Li L, et al. A study on small-world brain functional networks altered by postherpetic neuralgia. Magn Reson Imaging. 2014;32(4):359–365. | ||
Geha PY, Baliki MN, Chialvo DR, et al. Brain activity for spontaneous pain of postherpetic neuralgia and its modulation by lidocaine patch therapy. Pain. 2007;128(1–2):88–100. | ||
Liu J, Hao Y, du M, et al. Quantitative cerebral blood flow mapping and functional connectivity of postherpetic neuralgia pain: a perfusion fMRI study. Pain. 2013;154(1):110–118. | ||
Jiang J, Gu L, Bao D, et al. Altered homotopic connectivity in postherpetic neuralgia: a resting state fMRI study. J Pain Res. 2016;9:877–886. | ||
Sarnthein J, Stern J, Aufenberg C, Rousson V, Jeanmonod D. Increased EEG power and slowed dominant frequency in patients with neurogenic pain. Brain. 2006;129(Pt 1):55–64. | ||
Stern J, Jeanmonod D, Sarnthein J. Persistent EEG overactivation in the cortical pain matrix of neurogenic pain patients. Neuroimage. 2006;31(2):721–731. | ||
Fallon N, Chiu Y, Nurmikko T, Stancak A. Altered theta oscillations in resting EEG of fibromyalgia syndrome patients. Eur J Pain. 2018;22(1):49–57. | ||
Vuckovic A, Hasan MA, Fraser M, et al. Dynamic oscillatory signatures of central neuropathic pain in spinal cord injury. J Pain. 2014;15(6):645–655. | ||
Jensen MP, Sherlin LH, Gertz KJ, et al. Brain EEG activity correlates of chronic pain in persons with spinal cord injury: clinical implications. Spinal Cord. 2013;51(1):55–58. | ||
Cao S, Song G, Zhang Y, et al. Abnormal local brain activity beyond the pain matrix in postherpetic neuralgia patients: a resting-state functional MRI study. Pain Physician. 2017;20(2):E303. | ||
Cao S, Li Y, Deng W, et al. Local brain activity differences between herpes zoster and postherpetic neuralgia patients: a resting-state functional MRI study. Pain Physician. 2017;20(5):E687. | ||
Zuo XN, di Martino A, Kelly C, et al. The oscillating brain: complex and reliable. Neuroimage. 2010;49(2):1432–1445. | ||
Hu X, Chen S, Huang CB, Qian Y, Yu Y. Frequency-dependent changes in the amplitude of low-frequency fluctuations in patients with Wilson’s disease: a resting-state fMRI study. Metab Brain Dis. 2017;32(3):685–692. | ||
Li F, Zhou F, Huang M, Gong H, Xu R. Frequency-specific abnormalities of intrinsic functional connectivity strength among patients with amyotrophic lateral sclerosis: a resting-state fMRI study. Front Aging Neurosci. 2017;9:351. | ||
Merskey H, Bogduk N. Classification of Chronic Pain: Descriptions of Chronic Pain Syndromes and Definitions of Pain Terms. 2nd ed. Seattle: International Association for the Study of Pain; 1994. | ||
Yan CG, Wang XD, Zuo XN, Zang YF. DPABI: Data Processing and Analysis for (Resting-State) Brain Imaging. Neuroinformatics. 2016;14(3):339–351. | ||
van Dijk KR, Sabuncu MR, Buckner RL. The influence of head motion on intrinsic functional connectivity MRI. Neuroimage. 2012;59(1):431–438. | ||
Zang YF, He Y, Zhu CZ, et al. Altered baseline brain activity in children with ADHD revealed by resting-state functional MRI. Brain Dev. 2007;29(2):83–91. | ||
Gao L, Bai L, Zhang Y, et al. Frequency-dependent changes of local resting oscillations in sleep-deprived brain. PLoS One. 2015;10(3):e0120323. | ||
Raichle ME. The brain’s default mode network. Annu Rev Neurosci. 2015;38:433–447. | ||
Whitfield-Gabrieli S, Ford JM. Default mode network activity and connectivity in psychopathology. Annu Rev Clin Psychol. 2012;8:49–76. | ||
Wang Y, Xu C, Zhai L, et al. Spatial-temporal signature of resting-state BOLD signals in classic trigeminal neuralgia. J Pain Res. 2017;10:2741–2750. | ||
Cole MW, Schneider W. The cognitive control network: Integrated cortical regions with dissociable functions. Neuroimage. 2007;37(1):343–360. | ||
Lorenz J, Minoshima S, Casey KL. Keeping pain out of mind: the role of the dorsolateral prefrontal cortex in pain modulation. Brain. 2003;126(Pt 5):1079–1091. | ||
Garcia-Larrea L, Peyron R. Pain matrices and neuropathic pain matrices: a review. Pain. 2013;154(Suppl 1):S29–S43. | ||
Sinding C, Gransjøen AM, Schlumberger G, Grushka M, Frasnelli J, Singh PB. Grey matter changes of the pain matrix in patients with burning mouth syndrome. Eur J Neurosci. 2016;43(8):997–1005. | ||
Raichle ME, Macleod AM, Snyder AZ, Powers WJ, Gusnard DA, Shulman GL. A default mode of brain function. Proc Natl Acad Sci. 2001;98(2):676–682. | ||
Cavanna AE, Trimble MR. The precuneus: a review of its functional anatomy and behavioural correlates. Brain. 2006;129(Pt 3):564–583. | ||
Pijnenburg M, Brumagne S, Caeyenberghs K, et al. Resting-state functional connectivity of the sensorimotor network in individuals with nonspecific low back pain and the association with the sit-to-stand-to-sit task. Brain Connect. 2015;5(5):303–311. | ||
Moulton EA, Schmahmann JD, Becerra L, Borsook D. The cerebellum and pain: passive integrator or active participator? Brain Res Rev. 2010;65(1):14–27. | ||
Huang T, Zhao Z, Yan C, et al. Altered spontaneous activity in patients with persistent somatoform pain disorder revealed by regional homogeneity. PLoS One. 2016;11(3):e0151360. | ||
Herrington JD, Nymberg C, Schultz RT. Biological motion task performance predicts superior temporal sulcus activity. Brain Cogn. 2011;77(3):372–381. | ||
Manto M, Bower JM, Conforto AB, et al. Consensus paper: roles of the cerebellum in motor control--the diversity of ideas on cerebellar involvement in movement. Cerebellum. 2012;11(2):457–487. | ||
Borich MR, Brodie SM, Gray WA, Ionta S, Boyd LA. Understanding the role of the primary somatosensory cortex: opportunities for rehabilitation. Neuropsychologia. 2015;79(Pt B):246–255. | ||
Chen TL, Babiloni C, Ferretti A, et al. Human secondary somatosensory cortex is involved in the processing of somatosensory rare stimuli: an fMRI study. Neuroimage. 2008;40(4):1765–1771. | ||
Vrana A, Hotz-Boendermaker S, Stämpfli P, et al. Differential neural processing during motor imagery of daily activities in chronic low back pain patients. PLoS One. 2015;10(11):e0142391. | ||
Buzsáki G, Draguhn A. Neuronal oscillations in cortical networks. Science. 2004;304(5679):1926–1929. | ||
Calvert GA. Crossmodal processing in the human brain: insights from functional neuroimaging studies. Cereb Cortex. 2001;11(12):1110–1123. | ||
Davis KD, Pope GE, Crawley AP, Mikulis DJ. Neural correlates of prickle sensation: a percept-related fMRI study. Nat Neurosci. 2002;5(11):1121–1122. | ||
Denkinger MD, Lukas A, Nikolaus T, Peter R, Franke S; ActiFE Study Group. Multisite pain, pain frequency and pain severity are associated with depression in older adults: results from the ActiFE Ulm study. Age Ageing. 2014;43(4):510–514. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.