Back to Journals » Journal of Pain Research » Volume 10
Benzodiazepine use in patients with chronic pain in an interdisciplinary pain rehabilitation program
Authors Cunningham JL, Craner JR, Evans MM, Hooten WM
Received 29 September 2016
Accepted for publication 18 November 2016
Published 9 February 2017 Volume 2017:10 Pages 311—317
DOI https://doi.org/10.2147/JPR.S123487
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Michael Schatman
Julie L Cunningham,1 Julia R Craner,2,3 Michele M Evans,2 W Michael Hooten4
1Department of Pharmacy, Mayo Clinic College of Medicine, Rochester, MN, 2Department of Psychiatry and Psychology, Mayo Clinic, Mayo Clinic College of Medicine, Rochester, MN, 3Department of Psychiatry and Behavioral Medicine, Spectrum Health System, Grand Rapids, MI, 4Department of Anesthesiology, Mayo Clinic, and Mayo Clinic College of Medicine, Rochester, MN, USA
Objectives: In the context of widespread opioid use, increased emphasis has been placed on the potentially deleterious effects of concurrent benzodiazepine (BZD) and opioid use. Although use of opioids in chronic pain has been a major focus, BZD use is equally concerning. Thus, the primary aim of this study was to determine the associations between BZD and opioid use in adults with chronic pain upon admission to an outpatient interdisciplinary pain rehabilitation (IPR) program.
Methods: The study cohort involved 847 consecutive patients admitted to a 3-week outpatient IPR program from January 2013 through December 2014. Study variables included baseline demographic and clinical characteristics, Center for Epidemiologic Studies-Depression Scale, Pain Catastrophizing Scale, and the pain severity subscale of the Multidimensional Pain Inventory.
Results: Upon admission, 248 (29%) patients were taking BZDs. Patients using BZDs were significantly more likely to use opioids and to be female. Additionally, patients using BZDs had significantly greater depression, pain catastrophizing, and pain severity scores. In univariable logistic regression analysis, opioid use, female sex, and greater scores of depression, pain catastrophizing, and pain severity were significantly associated with BZD use. In multivariable logistic regression analysis adjusted for age, sex, pain duration, opioid use, depression, pain catastrophizing, and pain severity, only female sex and greater depression scores were significantly associated with BZD use.
Discussion: Among patients participating in an outpatient IPR program, female sex and greater depression scores were associated with BZD use. Results identify a high prevalence of BZD use in patients with chronic pain and reinforce the need to weigh the risks versus benefits when prescribing in this patient population.
Keywords: benzodiazepine, chronic pain, opioid, pain rehabilitation
Introduction
In the context of widespread opioid use in the United States, increased emphasis has been placed on the potentially deleterious effects of concurrent benzodiazepine (BZD) and opioid use.1 Among individuals with chronic pain, the coadministration of BZDs and opioids have been associated with elevated rates of cognitive dysfunction, sedation, central sleep apnea, respiratory depression, and overdose deaths.2–7 The pharmacological effects of BZDs are due to the potentiation of the inhibitory neurotransmitter γ-aminobutyric acid (GABA) on GABAA-receptors. When administered concurrently, BZD-related inhibitory effects can be synergistic with the inhibitory effects of opioids.
BZDs are widely used to treat a broad range of mental health problems. This is relevant because the prevalence of commonly occurring mental health disorders in adults with chronic pain exceeds 50%–60%.8 Although associations between BZDs, opioids, and various clinical factors have been observed in primary care and population-based studies,9–11 the potential correlates of BZD use in patients undergoing interdisciplinary pain rehabilitation (IPR) have not been reported. This is important because this patient population has high rates of long-term opioid use and high levels of depressive symptoms, pain catastrophizing, and pain severity.12–14 Thus, the primary aim of this study was to determine the associations between BZD use and opioid use in adults with chronic pain upon admission to an outpatient IPR program. Secondary aims include investigating the associations between BZD use and depressive symptoms, pain catastrophizing, pain severity, and demographic characteristics.
Methods
This study was approved by the Mayo Foundation Institutional Review Board, and all patients provided prior written consent for use of their medical records for research purposes.
Study participants
Participants in this study included 847 patients who were consecutively admitted to the Mayo Comprehensive Pain Rehabilitation Center from January 2013 through December 2014. Inclusion criteria were as follows: admission to the pain rehabilitation center, chronic noncancer pain of greater than 6 months duration, and age greater than 18 years. Exclusion criteria included medical, surgical or psychiatric conditions that prevented full participation in the treatment protocols of the pain rehabilitation program.
Study setting
The clinical setting of the outpatient IPR program has been previously described.15 In summary, patients attended the outpatient IPR program 8 hours daily for 15 consecutive working days. A cognitive behavioral model served as the basis for treatment, and the primary treatment goal was restoration of physical and emotional functioning. The established treatment protocols included daily physical and occupational therapy. In addition, all patients attended educational group sessions about management of depressive symptoms, relaxation training, stress management, activity moderation, and elimination of pain behaviors.
Demographic and clinical characteristics
Baseline demographic and clinical characteristics were collected at admission and included detail about age, sex, pain duration, marital status, years of education, ethnicity, and concurrent opioid use. The primary diagnoses of patients admitted to this program were low back pain, fibromyalgia, and chronic headaches (as previously described).15,16
Determination of BZD daily dose
Each patient was interviewed at program admission by a Doctor of Pharmacy to obtain an accurate medication list as previously described.16 Medications were categorized individually and by drug class. The average daily BZD dose was converted to an oral diazepam equivalent dose based on established equivalency dosing.17 Patients were separated into four groups for comparison: patients taking BZDs, those taking opioids, those taking both BZD and opioids, those and not taking either BZD or opioids on admission.
Measures
At IPR program admission, study participants completed questionnaires to assess pain severity, depressive symptoms, and pain catastrophizing.
Pain severity
Pain severity was assessed using the pain severity subscale of the Multidimensional Pain Inventory.18 Three questions comprise the pain severity subscale: 1) “Rate the level of your pain at the present moment”; 2) “On the average, how severe has your pain been during the last week”; and 3) “How much suffering do you experience because of your pain.” This self-report questionnaire has proven reliability and construct validity.19
Depressive symptoms
Depressive symptoms were assessed using the Center for Epidemiologic Studies-Depression (CES-D) scale. This scale provides a measure of the presence and severity of depressive symptoms that have occurred in the past week.20 The 20-item self-administered questionnaire has established reliability and validity and is scored on a 5-point Likert scale (ranging from 0 to 4).21 Total scores range from 0 to 60, with higher scores indicating greater levels of depression. A cutoff score of 16 or greater has been used to identify patients with minor depressive symptoms,22 while a cutoff score of 27 or greater has been used to identify major depressive symptoms in patients who have chronic pain.23
Pain catastrophizing
The Pain Catastrophizing Scale (PCS) is a 13-item scale that assesses rumination, magnification, and helplessness.24 Pain catastrophizing is defined as a negative set of cognitions and emotions associated with an actual or anticipated pain experience. The PCS has been associated with increased disability, pain and illness behaviors, greater use of health care services, longer durations of hospital stays, and the use of analgesic medications.25
Statistical analyses
The demographic and clinical characteristics were recorded. Mean and standard deviation (±) were reported for the continuous variables, and count and proportion were reported for the categorical variables. Continuous and categorical variables were compared using a nonparametric test (Kruskal–Wallis Test). Focused contrast analysis of group differences in depression, pain catastrophizing, and pain severity were performed using the Tukey HSD test. Univariate logistic regression analyses were performed using BZD use as the binary (BZD use versus no BZD use) dependent variable. Independent variables included age, sex, pain duration, opioid use, depression, pain catastrophizing, and pain severity. These variables were selected because 1) significant group differences were observed based on categories of medication use and 2) they have been previously shown to influence the clinical outcomes of pain rehabilitation.12,13,16,25–28 Multiple logistic regression analyses were then performed using the abovementioned dependent and independent variables, and goodness of fit was assessed using the Hosmer and Lemeshow Test. The level of significance for all statistical tests was set at P<0.05, and all analyses were completed using Statistical Package for the Social Sciences (SPSS) (Version 21.0, IBM, Inc., Chicago, IL, USA).
Results
Sample characteristics
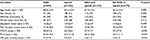
Demographic and clinical characteristics are summarized in Table 1. The majority of study participants were married female Caucasians with an average age of 48 years. BZD use without opioids occurred in 11% of patients, 38% were using opioids without BZDs, 18% were using BZDs and opioids, and 33% were using no BZDs or opioids. Women were more likely to use a BZD with or without an opioid, and married patients were more likely to use BZDs, opioids, or both. Patients using BZDs and opioids reported greater levels of depression, pain catastrophizing, and pain severity (Figure 1).
BZD use
The median diazepam equivalent dose was 15 mg (25th to 75th interquartile range =7.5–25 mg). Clonazepam was used by 28.1% of patients; lorazepam was used by 24.4%, alprazolam was used by 24.0%, diazepam was used by 15.7%, and 7.8% of patients were using other BZDs. Twenty-six (10.5%) patients used two or more BZDs.
Associations between BZD use, demographic factors, and clinical characteristics
In univariable logistic regression analysis, opioid use and female sex were significantly associated with BZD use (Table 2). In addition, greater depression, pain catastrophizing, and pain severity scores were significantly associated with BZD use. However, in multivariable logistic regression analysis adjusted for age, sex, pain duration, opioid use, depression, pain catastrophizing, and pain severity, only female sex and greater depression scores were significantly associated with BZD use (Homsmer and Lemeshow Test, P=0.140 indicating adequate goodness of fit).
Discussion
The primary finding of the current study is that BZD use was associated with important patient characteristics in a large sample of patients with chronic pain (N=847) admitted to an IPR program. In the current sample, there was a large group of patients taking BZD (29.3%), and the majority of these patients (62%) were using both a BZD and opioid agent. Furthermore, patients taking BZDs reported greater perceived pain severity, depressive symptoms, and pain catastrophizing compared to patients not using BZDs. However, when taking into account demographic and clinical characteristics simultaneously, results indicated that patients taking BZDs were significantly more likely to be women and have higher levels of depressive symptoms. Accordingly, sex and depressive symptoms were unique predictors of BZD use on admission beyond the effects of age, ethnicity, education, marital status, pain severity, pain duration, pain catastrophizing, or opioid use.
These findings are consistent with and expand upon the results of several prior studies. It has been well documented that women, especially women over age 65, have a higher incidence of BZD use than men in both the general population and in patients with psychiatric diagnoses.29–32 Previous research also indicates a high prevalence of BZD use among patients with chronic opioid use9,10,33 and an association between BZD use and higher opioid dose.10,33 Furthermore, BZD use has been found to predict subsequent opioid use beyond the effects of the presence of a chronic pain condition.34 Collectively, these findings are in direct contrast to the recent guidelines for the use of opioids in CNP, which have recommended avoiding concurrent use of BZDs, especially in the elderly and patients at risk or recovering from addiction1,5,35,36 and caution about risk of adverse events with the concurrent use of the two substances.37
The risk of combined opioids and BZD for drug-related overdoses is well documented,38–41 and women and individuals with higher levels of depressive symptoms may be at especially high risk. Research has found an association of higher opioid dose, depression, and long BZD use durations as increasing risk for drug overdose.42 A recent study of patients who filled opioid prescriptions and had a subsequent drug overdose found a strong association between BZD use and overdose and greater incidence of overdose in women despite lower morphine equivalent doses compared to men.43 In women, depression or psychosis was found to be the second most important risk factor for overdose. These findings suggest that the high rates of concurrent opioid and BZD use in the current sample and the strong association between sex and depressive symptoms with BZD may present a concern for elevated risk of adverse outcomes in this population.
Prior literature also supports the finding of greater impairment among chronic pain patients using BZDs. For example, Nielsen et al10 found similar results of higher pain severity and pain interference for BZD users compared to non-BZD substance users. In addition, this study identified that patients using BZDs reported lower self-efficacy, higher use of antidepressants and antipsychotics, as well as substance use. Further, BZD use has previously been associated with worsening depression in CNP populations.9 However, it is unclear based on current research whether high rates of BZD use in CNP patients is the result of psychiatric problems that predate or develop as a result of CNP, or whether BZDs are being prescribed as a therapeutic treatment of CNP. Following a thorough review of the literature, Dellemijn and Fields44 conclude there is some limited evidence to suggest BZDs may be useful in reducing the affective component of acute pain and may be useful in chronic conditions such as chronic tension headaches, TMJ disorders, and tic douloureux.44 King and Strain9 reviewed a CNP population and found in more than 90% of the patients the BZD agent was started after the onset of pain. In this patient population, 86% of patients reported the use of BZDs to improve sleep; however, they continued to report as many sleep problems as the non-BZD group. The current findings that patients using BZDs endorse greater depressive symptoms and catastrophic thinking compared to those not using BZDs lends support to the claim that these patients may have more psychiatric symptoms. However, the reason for this association cannot be determined based on current results.
The current study also provides useful information about BZD prescribing patterns for patients with CNP. A recent study in Australia reported that diazepam was the most commonly used BZD agent; however, in our US-based sample, clonazepam was the most common BZD agent, whereas diazepam was the fourth most common agent. This result is somewhat unexpected, as diazepam is frequently used as an adjunctive agent due to its muscle relaxant properties.45 On the other hand, the high rate of clonazepam use may suggest further evidence of a link between anxiety-related indications for BZD use among CNP patients.
Limitations
There are several strengths of the current study, including the use of a large treatment-seeking clinical sample and the collection of data from both self-report measures and medical chart review. However, there are also several important limitations to this study design. Given that patients in this study reported long illness duration and severities, presented for program admission, and were primarily Caucasian, married, and college-educated, this limits the applicability of our findings to other populations of patients with CNP. Furthermore, the presence of psychiatric distress was based on the results of self-report measures of depressive symptoms and catastrophic thinking, without structured clinical interview or diagnostic information available. In addition, the study design was cross-sectional; accordingly, causality between clinical characteristics and outcomes cannot be determined based on the results of this study.
Conclusion
The results of the current study suggest that patients with CNP who are using BZDs on admission to a chronic pain rehabilitation program are characterized by greater levels of impairment and may be at higher risk adverse outcomes. In addition, women and those with worse depressive symptoms were significantly more likely to use BZDs. CNP providers should weigh the risks versus benefits when prescribing BZDs to patients with CNP, especially in combination with opioid, and work with patients to taper and eliminate BZDs when present.
Acknowledgment
The authors acknowledge David Cloptin for his expertise and contributions to the literature review.
Disclosure
The authors report no conflicts of interest in this work.
References
Dowell D, Haegerich TM, Chou R. CDC Guideline for prescribing opioids for chronic pain – United States, 2016. JAMA. 2016;315(15): | ||
Burrows DL, Hagardorn AN, Harlan GC, Wallen ED, Ferslew KE. A fatal drug interaction between oxycodone and clonazepam. J Forensic Sci. 2003;48(3):683–686. | ||
de Wet C, Reed L, Glasper A, Moran P, Bearn J, Gossop M. Benzodiazepine co-dependence exacerbates the opiate withdrawal syndrome. Drug Alcohol Depend. 2004;76(1):31–35. | ||
Kouyanou K, Pither CE, Wessely S. Medication misuse, abuse and dependence in chronic pain patients. J Psychosom Res. 1997;43(5): | ||
Manchikanti L, Abdi S, Atluri S, et al. American Society of Interventional Pain Physicians (ASIPP) guidelines for responsible opioid prescribing in chronic non-cancer pain: Part 2 – guidance. Pain Physician. 2012;15(3 Suppl):S67–S116. | ||
Marriott S, Tyrer P. Benzodiazepine dependence. Avoidance and withdrawal. Drug Saf. 1993;9(2):93–103. | ||
Webster LR, Choi Y, Desai H, Webster L, Grant BJ. Sleep-disordered breathing and chronic opioid therapy. Pain Med. 2008;9(4):425–432. | ||
Hooten WM. Chronic pain and mental health disorders: shared neural mechanisms, epidemiology, and treatment. Mayo Clin Proc. 2016;91(7):955–970. | ||
King SA, Strain JJ. Benzodiazepine use by chronic pain patients. Clin J Pain. 1990;6(2):143–147. | ||
Nielsen S, Lintzeris N, Bruno R, et al. Benzodiazepine use among chronic pain patients prescribed opioids: associations with pain, physical and mental health, and health service utilization. Pain Med. 2015; | ||
Simon GE, VonKorff M, Barlow W, Pabiniak C, Wagner E. Predictors of chronic benzodiazepine use in a health maintenance organization sample. J Clin Epidemiol. 1996;49(9):1067–1073. | ||
Crisostomo RA, Schmidt JE, Hooten WM, Kerkvliet JL, Townsend CO, | ||
Hooten WM, Shi Y, Gazelka HM, Warner DO. The effects of depression and smoking on pain severity and opioid use in patients with chronic pain. Pain. 2011;152(1):223–229. | ||
Hooten WM, Townsend CO, Bruce BK, Warner DO. The effects of smoking status on opioid tapering among patients with chronic pain. Anesth Analg. 2009;108(1):308–315. | ||
Townsend CO, Bruce BK, Hooten WM, Rome JD. The role of mental health professionals in multidisciplinary pain rehabilitation programs. J Clin Psychol. 2006;62(11):1433–1443. | ||
Cunningham JL, Rome JD, Kerkvliet JL, Townsend CO. Reduction in medication costs for patients with chronic nonmalignant pain completing a pain rehabilitation program: a prospective analysis of admission, discharge, and 6-month follow-up medication costs. Pain Med. 2009;10(5):787–796. | ||
Chouinard G. Issues in the clinical use of benzodiazepines: potency, withdrawal, and rebound. J Clin Psychiatry. 2004;65(Suppl 5):7–12. | ||
Kerns RD, Turk DC, Rudy TE. The West Haven-Yale Multidimensional Pain Inventory (WHYMPI). Pain. 1985;23(4):345–356. | ||
Bernstein IH, Jaremko ME, Hinkley BS. On the utility of the West Haven-Yale Multidimensional Pain Inventory. Spine (Phila Pa 1976). 1995;20(8):956–963. | ||
Radloff L. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401. | ||
Radloff LS, Locke BZ. The community mental health assessment survey and the CES-D scale. In: Weissman MM, Myers JK, Ross CE, editors. Community Surveys of Psychiatric Disorders. Piscataway, NJ: Rutgers University Press; 1977. | ||
Weissman MM, Sholomskas D, Pottenger M, Prusoff BA, Locke BZ. Assessing depressive symptoms in five psychiatric populations: a validation study. Am J Epidemiol. 1977;106(3):203–214. | ||
Geisser ME, Roth RS, Robinson ME. Assessing depression among persons with chronic pain using the Center for Epidemiological Studies-Depression Scale and the Beck Depression Inventory: a comparative analysis. Clin J Pain. 1997;13(2):163–170. | ||
Sullivan M, Bishop S, Pivik J. The pain catastrophizing scale: development and validation. Psychol Assess.1995;7:524–532. | ||
Sullivan MJ, Thorn B, Haythornthwaite JA, et al. Theoretical perspectives on the relation between catastrophizing and pain. Clin J Pain. 2001;17(1):52–64. | ||
Hooten WM, Knight-Brown M, Townsend CO, Laures HJ. Clinical outcomes of multidisciplinary pain rehabilitation among African American compared with caucasian patients with chronic pain. Pain Med. 2012;13(11):1499–1508. | ||
Hooten WM, Townsend CO, Decker PA. Gender differences among patients with fibromyalgia undergoing multidisciplinary pain rehabilitation. Pain Med. 2007;8(8):624–632. | ||
Hooten WM, Townsend CO, Sletten CD, Bruce BK, Rome JD. Treatment outcomes after multidisciplinary pain rehabilitation with analgesic medication withdrawal for patients with fibromyalgia. Pain Med. 2007;8(1):8–16. | ||
Morgan SG, Weymann D, Pratt B, et al. Sex differences in the risk of receiving potentially inappropriate prescriptions among older adults. Age Ageing. 2016;45(4):535–542. | ||
Boyd A, Van de Velde S, Pivette M, et al. Gender differences in psychotropic use across Europe: results from a large cross-sectional, population-based study. Eur Psychiatry. 2015;30(6):778–788. | ||
Karanti A, Bobeck C, Osterman M, et al. Gender differences in the treatment of patients with bipolar disorder: a study of 7354 patients. J Affect Disord. 2015;174:303–309. | ||
McCabe SE, West BT. Medical and nonmedical use of prescription benzodiazepine anxiolytics among US high school seniors. Addict Behav. 2014;39(5):959–964. | ||
Hermos JA, Young MM, Gagnon DR, Fiore LD. Characterizations of long-term oxycodone/acetaminophen prescriptions in veteran patients. Arch Intern Med. 2004;164(21):2361–2366. | ||
Skurtveit S, Furu K, Bramness J, Selmer R, Tverdal A. Benzodiazepines predict use of opioids – a follow-up study of 17,074 men and women. Pain Med. 2010;11(6):805–814. | ||
Miotto K, Kaufman A, Kong A, Jun G, Schwartz J. Managing co-occurring substance use and pain disorders. Psychiatr Clin North Am. 2012;35(2):393–409. | ||
Interagency Guideline on Prescribing Opioids for Pain. In: (CSAT) WSAMDGAAT, ed. Vol 3rd edition; 2015:1–105. | ||
Chou R, Fanciullo GJ, Fine PG, et al. Clinical guidelines for the use of chronic opioid therapy in chronic noncancer pain. J Pain. 2009;10(2):113–130. | ||
Dasgupta N, Funk MJ, Proescholdbell S, Hirsch A, Ribisl KM, Marshall S. Cohort study of the impact of high-dose opioid analgesics on overdose mortality. Pain Med. 2016;17(1):85–98. | ||
Gomes T, Mamdani MM, Dhalla IA, Paterson JM, Juurlink DN. Opioid dose and drug-related mortality in patients with nonmalignant pain. Arch Intern Med. 2011;171(7):686–691. | ||
Jones CM, McAninch JK. Emergency department visits and overdose deaths from combined use of opioids and benzodiazepines. Am J Prev Med. 2015;49(4):493–501. | ||
Jones CM, Mack KA, Paulozzi LJ. Pharmaceutical overdose deaths, United States, 2010. JAMA. 2013;309(7):657–659. | ||
Turner BJ, Liang Y. Drug overdose in a retrospective cohort with non-cancer pain treated with opioids, antidepressants, and/or sedative-hypnotics: interactions with mental health disorders. J Gen Intern Med. 2015;30(8):1081–1096. | ||
Liang Y, Goros MW, Turner BJ. Drug overdose: differing risk models for women and men among opioid users with non-cancer pain. Pain Med. Epub 2016 Apr 28. | ||
Dellemijn PL, Fields HL. Do benzodiazepines have a role in chronic pain management? Pain. 1994;57(2):137–152. | ||
See S, Ginzburg R. Skeletal muscle relaxants. Pharmacotherapy. 2008;28(2):207–213. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.