Back to Journals » Clinical and Experimental Gastroenterology » Volume 12
Benign biliary strictures: prevalence, impact, and management strategies
Authors Ma MX , Jayasekeran V, Chong AK
Received 24 October 2018
Accepted for publication 17 January 2019
Published 18 February 2019 Volume 2019:12 Pages 83—92
DOI https://doi.org/10.2147/CEG.S165016
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Anastasios Koulaouzidis
Michael Xiang Ma,1,2 Vanoo Jayasekeran,1 Andre K Chong1
1Department of Gastroenterology and Hepatology, Fiona Stanley Hospital, Murdoch, Perth, WA 6150, Australia; 2Midland Physician Service, St John of God Midland Public Hospital, Midland, Perth, WA 6056, Australia
Abstract: Benign biliary strictures (BBSs) may form from chronic inflammatory pancreaticobiliary pathologies, postoperative bile-duct injury, or at biliary anastomoses following liver transplantation. Treatment aims to relieve symptoms of biliary obstruction, maintain long-term drainage, and preserve liver function. Endoscopic therapy, including stricture dilatation and stenting, is effective in most cases and the first-line treatment of BBS. Radiological and surgical therapies are reserved for patients whose strictures are refractory to endoscopic interventions. Response to treatment is dependent upon the technique and accessories used, as well as stricture etiology. In this review, we discuss the various BBS etiologies and their management strategies.
Keywords: benign biliary stricture, endoscopic retrograde cholangiopancreatography, metal stent, plastic stent, stricture dilatation, chronic pancreatitis, liver transplantation, primary sclerosing cholangitis
Introduction
BBSs most often arise from postoperative or inflammatory etiologies. Surgery-related BBS most frequently results from LC, bile-duct surgery, and liver transplantation. The incidence of LC-related BS is ~0.5%, usually caused by direct surgical bile-duct injury, including thermal injury, scissors, ligatures, or clips. 1 BSs that form following liver transplantation occur in ~10%–40% of cases, and most commonly occur at the anastomotic site.2,3
CP-related BSs are the most common nonsurgical BBSs, occurring in up to 13%–21% of patients.4,5 These CP-related strictures usually involve the distal CBD, and may be difficult to treat, due to fibrosis, scarring, and calcification of the bile-duct wall. Other causes of BBS include those related to PSC, choledocholithiasis, and autoimmune (IgG4) cholangiopathy (Table 1).
  | Table 1 Causes of benign biliary strictures Abbreviations: SLE, systemic lupus erythematosus; ANCA, antineutrophil cytoplasmic antibody. |
The clinical presentation of these BBSs may be varied, depending upon their etiology, location within the biliary tree, and degree of ductal narrowing. Accordingly, patients may be asymptomatic, have biochemical derangements in liver enzymes, or present with deep jaundice complicated by life-threatening cholangitis. Treatment methods and outcomes also vary, as described in the following sections.
Diagnosis
Identification of a suspected BBS requires correlation of a patient’s clinical history, imaging studies, including CT and/or MRI, and endoscopic findings. Histological assessment with cytology or histopathology is usually required to exclude malignancy. Some cases may be diagnostically challenging, requiring a multidisciplinary approach and/or a prolonged period of clinical surveillance for exclusion of underlying occult malignancy.
Cross-sectional abdominal imaging can localize pathology, as well as provide a roadmap to plan therapeutic ERCP. MRCP and/or CT are often used for first-line imaging in patients with biliary obstruction. MRCP provides noninvasive, detailed images of the biliary tree, along with the location, length, and character of BSs prior to ERCP. MRCP features of BBS are characterized by regular, symmetrical, and short-segment narrowing. In contrast, malignant strictures are usually irregular, asymmetrical and of longer length, especially those ≥14 mm.6 Table 2 describes the most commonly used anatomical classification of BBS.
  | Table 2 Bismuth classification for benign biliary strictures |
ERCP and/or endoscopic ultrasound-guided fine-needle aspiration or biopsy are used to establish a histological diagnosis. ERCP-guided methods include brush cytology or transpapillary forceps biopsy. Both have high specificity but low sensitivity in diagnosing BS. A meta-analysis showed that sensitivity and specificity for diagnosis of malignant BS using brush cytology was 45% and 99%, respectively. and using transpapillary forceps biopsy 48.1% and 99.2%, respectively.7 Combining both modalities modestly increased sensitivity (59.4%), with a specificity of 100%.7
To improve diagnostic yield, particularly for indeterminate strictures, adjunctive technologies, such as endoscopic ultrasound-guided fine-needle aspiration, cholangioscopy with biopsy, FISH, intraductal ultrasound, and confocal laser endomicroscopy, have been used. For benign-appearing strictures, clinical follow-up of at least 6 months with a benign course may help to confirm the diagnosis. This is supported by a prospective single-center follow-up study involving 104 patients with indeterminate BSs, which showed detection of biliary cancer was more common during the first 6 months of follow-up.8 For patients with PSC, long-term patient follow-up is recommended, due to the risk of developing future biliary malignancy.
Management
Endoscopic
ERCP is the first-line management option for most patients with BBS. Endoscopic access to the major papilla is a prerequisite. Endoscopic therapy for BBS is safe, effective, repeatable, and less invasive than other treatment options, such as percutaneous or surgical modalities.9 Endoscopic methods to treat BBS include stricture dilatation using an over-the-wire balloon or bougie, followed by insertion of one or more plastic stents or a fully covered self-expandable metal stent (FCSEMS; Table 3). Plastic stents are changed periodically at intervals of 6–12 months to promote biliary drainage and stricture resolution. Recent data support the use of the FCSEMS for treatment of BBS. Reported advantages include high technical and clinical success, ease of insertion, and need of fewer endoscopic procedures for stricture resolution compared with multiple plastic stents.10
In a large prospective multicenter study of 177 patients with BBS who received FCSEMS, stricture resolution was achieved in 135 (76.3%) patients. Endoscopic stent removal was achieved in all patients (n=131) scheduled for stent removal, of which 124 (94.7%) had no serious removal-related adverse events. 11 In another study where FCSEMSs were placed for 6 months in patients with CP-associated BBS refractory to prior placement of a 10 Fr plastic stent, stricture resolution was achieved in 70.6% (12 of 17). No stricture recurrence occurred in the eight patients who completed 2-year follow-up.12
Preparation
Prophylactic administration of intravenous antibiotics covering the Gram-negative bacteria Enterococcus and Pseudomonas are recommended for patients with hilar strictures, liver transplantation, and PSC, due to the potential for complex or multiple strictures complicating these conditions. However, for other patients, prophylactic antibiotics do not appear to prevent ERCP-related cholangitis.13,14 Incomplete biliary drainage is associated with an increased risk of bacteremia and cholangitis.15 Other factors associated with ERCP-related cholangitis in PSC include longer procedural duration and intraductal manipulation, eg, brush cytology, forceps biopsy, balloon dilatation, and cholangioscopy.
Endoscopic access
Therapeutic ERCP requires successful deep biliary cannulation with a wire. A biliary sphincterotomy facilitates placement of stents and assists endoscopic access for future ERCP, but does not appear to reduce the risk of post-ERCP pancreatitis after plastic or metal-stent insertion. Adjunctive techniques including precut papillotomy, double or single guide wire over a pancreatic stent may assist selective biliary cannulation in difficult cases. Hydrophilic 0.035-inch (0.889 mm) guide wires are most commonly used; however, smaller-diameter wires (0.018, 0.021, or 0.025 inches) with or without an angulated tip may improve success of traversing a tight or angulated stricture. When conventional guide-wire methods fail, such techniques as retraction on an inflated extraction balloon to straighten the BBS or cholangioscopy-assisted guide-wire placement may assist.16 Forceful advancement of the wire should always be avoided, as this risks creation of a false tract or perforation of the bile duct.
Dilatation
For severe fibrotic strictures, initial balloon or bougie dilatation may be required, followed by placement of one or more plastic stents or an FCSEMS. Very tight strictures sometimes may only be crossed by a balloon dilator. All dilators are passed over a guide wire traversing the stricture, visualized under fluoroscopy. The size of the dilator is guided by the width of the bile duct adjacent to the stricture. We recommend dilatation of the stricture for 30–60 seconds, or if using a balloon, until the stricture waist disappears. Forceful dilatation should be avoided, given the higher risk of ductal perforation, particularly in the early postoperative period (eg, within 4 weeks of liver transplantation) and/or while the patient is still on high-dose immunosuppression.17
Stricture recurrence after dilatation may be reduced by placement of a biliary stent.9,18 A systematic review of 19 studies showed treatment of anastomotic strictures after liver transplantation with plastic stents for longer periods predicted lower recurrence (OR 0.95, P=0.002), with overall stricture resolution in 86%.19 For CP-associated BBS, 90% stricture resolution was achieved with dilatation and placement of multiple 10 Fr plastic stents with regular stent change for 12 months. A systematic review of 25 studies found CP-related BBS treated by FCSEMS achieved greater resolution at 12 months than multiple plastic stents (77% vs 33%, respectively).20 For PSC-related strictures, dilatation alone usually achieves good long-term outcomes, even for dominant strictures.21
Stenting
Plastic stents
Extrahepatic BBS has traditionally been treated by placement of multiple plastic stents side by side across a stricture following dilatation. Long-term outcomes using this method may be equivalent or superior to those of surgical management, but with lower morbidity.22 A systematic review of 47 trials including 1,116 patients with extrahepatic BBS showed that placing multiple plastic stents had higher clinical success (94.3% vs 59.6%) and fewer adverse events (20.3% vs 36.0%) compared with placement of a single plastic stent, respectively.22
Treatment of BBS with plastic stents typically involves 3 monthly stent exchanges, with placement of an increasing number and/or diameter of stents for up to 12 months.23 Alternatively, the maximal number of stents can be inserted at the index ERCP, allowing reduced frequency of ERCP and stent exchange.24 Both approaches offer similar efficacy with regard to stricture resolution. Where multiple stents are used, duration of placement does not appear to affect incidence of symptomatic stent occlusion, and is similar for stents exchanged within 6 months compared to stents changed after longer periods.25
Metal stents
FCSEMSs are suitable for the treatment of BBS, as their silicone covering prevents tissue ingrowth and stent embedment into the duct wall. Conversely, uncovered SEMSs are unsuitable for treatment of BBS, because reactive tissue ingrowth into the bare-wire lattice prevents their later removal. A stent-in-stent technique whereby an FCSEMS is placed temporarily within an embedded partially or uncovered SEMS is a potential salvage method of retrieval.26
Although SEMSs are more expensive than plastic stents, they have significantly wider diameters (10 vs 3.3 mm, respectively), and are technically easier to insert than placing multiple plastic stents.27 A randomized trial comparing FCSEMSs and multiple plastic stents for the treatment of post-liver-transplantation BBS showed higher stricture resolution (81%–92% vs 76% – 90%), shorter stent placement time (3.8 vs 10.1 months), fewer endoscopic procedures (median 2.0 vs 4.5), fewer adverse events (10% vs 50%), and less cost for the FCSEMS group.28 Similar results were also reported in a separate recent randomized trial.29
FCSEMSs are unsuitable for treatment of hilar-located BBS, as a covered stent spanning the bifurcation may prevent biliary drainage from the opposite hepatic lobe.30 Cholecystitis is another potential complication of placing an FCSEMS in patients with an intact gallbladder, especially if the stent covers the cystic duct.27,31 The optimal FCSEMS indwelling duration is unknown, although recent evidence suggests placement of 6 months for post-liver-transplantation strictures and longer for BBS due to CP or cholecystectomy.11 A long FCSEMS indwelling time may increase the risk of cholangitis from stent occlusion or migration, and may hinder stent removal, as some embedding may occur from mucosal hyperplasia developing at the ends of the stent.32,33
FCSEMSs are also at risk of stent migration, which may reduce treatment efficacy and increase risk of adverse events. Insertion of a double-pigtail plastic stent within an FCSEMS may help to anchor it, and has been shown to reduce migration and prolong stent indwelling.34 Lastly, a recent comparative study of 43 patients found FCSEMSs with an anchored flap design may have superior antimigration effects compared with those with a traditional flared proximal-end design.35
Percutaneous
PTBD is useful for cases of failed ERCP and surgically altered anatomy preventing access to the major papilla, such as Roux-en-Y hepaticojejunostomy, gastric-outlet obstruction from duodenal compression, or a prior duodenal stent. A PTBD approach is less invasive and lower-risk compared to surgery.36
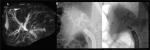
PTBD may facilitate rendezvous ERCP or be used as a primary means of stricture management. In a prospective study, percutaneous catheter dilatation of single extrahepatic BSs with progressively larger catheters up to 18–20 Fr resulted in stricture resolution in 64% of patients with post-liver-transplantation strictures and 86% of patients with BBS from other causes. 37 Percutaneous transhepatic balloon dilatation (Figure 1) and/or placement of removable covered metal stents are also treatment options for BBS.38
  | Figure 1 Percutaneous transhepatic balloon dilatation of a proximal common bile-duct stricture. |
Surgical
Surgery may be required for patients with refractory BBS or those who are noncompliant with endoscopic therapy. For example, a prospective study of patients with CP found those with pancreatic head calcifications were 17-times more likely to have failure of response to endoscopic stenting.39 Surgical treatment may provide better long-term outcomes for patients with persisting CP-associated BBS after more than three endoscopic procedures.40 Post-liver-transplantation nonanastomotic BSs also have lower treatment success following endoscopic drainage than those with anastomotic strictures.41
As with endoscopic and percutaneous methods, the goal of operative management of BBS is establishment of bile flow to relieve jaundice and to prevent cholangitis, choledocholithiasis, and recurrent stricture. Surgical alternatives to repair of BBS include excision of strictures with end-to-end repair, Roux-en-Y hepaticojejunostomy, choledochojejunostomy, and choledoduodenostomy. The choice of repair depends on such variables as extent and location of BBS.
End-to-end anastomosis may be performed if the stricture is short, extrahepatic, and the ends can be opposed without tension. However, this approach is seldom used, given the inevitable loss of ductal length associated with fibrosis, as well as a high risk of postoperative stricture recurrence. Choledochoduodenostomy and Frey’s procedures are described for treatment of distal BSs in the setting of CP. For the majority of cases, a Roux-en-Y hepaticojejunostomy is the best choice of repair. With this technique, a Roux loop made of healthy, tension-free jejunum distal to the ligament of Treitz is passed to the hilum of the liver and anastomosed in an end-to-side fashion to the proximal bile duct. The procedure is safe and durable, with a rate of success of 80%–99% in the hands of experienced surgeons.
New techniques
Novel techniques, including magnetic compression anastomosis, intraductal radiofrequency ablation, and biodegradable stents, may be useful for selected BBS cases refractory to endoscopic or percutaneous methods. In a study of magnetic compression anastomosis, biliary recanalization was achieved in 89.7% (35 of 39) of patients with BBS due to surgical or traumatic etiologies. The average time from magnet approximation to removal was 57.4 days (range 13–182 days). Adverse events included one case of cholangitis and two cases of restenosis, which responded to endoscopic therapy.42
In a small study of nine patients with refractory BBS, intraductal bipolar radiofrequency ablation followed by balloon dilatation resulted in immediate stricture improvement in all patients. 43 Four patients had no recurrence of stricture after mean follow-up of 12.6 months. In one series of ten patients with refractory BBS, stricture resolution was achieved in all patients treated by a percutaneously placed biodegradable stent. No stent was visible at 6-month follow-up.44 In a series of 13 patients with BBS treated by endoscopically placed biodegradable stents, stricture resolution was 83% at 21-month follow-up.45 These methods are promising, but require further efficacy and safety evaluations prior to adoption into mainstream endoscopic practice.
Common etiologies
Chronic pancreatitis
Repeat inflammation and scarring of the pancreatic head in the setting of CP may result in formation of distal BSs (Figure 2). Endoscopic therapy is the recommended first-line treatment for CP-related CBD strictures, as it is less invasive than surgery. Nonetheless, CP-related strictures are more refractory to endoscopic treatment than other BBSs, especially if pancreatic calcifications are present.46 Placement of multiple plastic biliary stents has traditionally been used to treat CP-related BBS, although FCSEMS use is increasing because of their larger diameter, ease of placement, and need for fewer ERCP procedures.27,47
  | Figure 2 (A, B) Examples of distal common bile-duct strictures associated with chronic pancreatitis. Note: Both strictures are relatively smooth with mild upstream biliary dilatation. |
Systematic review data from 25 studies found endoscopic therapy to treat CP-associated BBS resulted in clinical success of 77% with covered SEMSs vs 33% with plastic stents at 12-month follow-up.20 The median number of ERCP procedures required to achieve clinical success was lower for SEMSs than plastic stents (1.5 vs 3.9, respectively; P=0.002).20 In another study of 60 patients with CP-related BBSs, patients were randomized to receive either a single 10 mm-diameter covered SEMS or three initial 10 Fr plastic stents, followed by placement of three more 10 Fr stents after 3 months. All stents were removed after 6 months. The 2-year stricture-free rate was 92% in patients receiving SEMSs and 90% in patients receiving plastic stents (P=0.405).27 Overall, the data support the use of covered SEMSs as an effective therapy for the management of CP-related BBS, and these may be considered for first-line use over plastic stents. A small percentage of patients may not respond to endoscopic therapies, and will eventually require surgical biliary drainage.
Primary sclerosing cholangitis
PSC may result in formation of both BBSs and malignant BSs, an important but sometimes difficult-to-diagnose distinction. PSC-associated BBS results from fibrotic inflammation and may be multifocal, intrahepatic, or extrahepatic in location. Traditional brush cytology of strictures has modest sensitivity (43%) with high specificity (97%) for cholangiocarcinoma.48 FISH and confocal laser endomicroscopy may increase the sensitivity of cholangiocarcinoma diagnosis in PSC, particularly if cytology is atypical.30 In a meta-analysis, the sensitivity and specificity of FISH for diagnosis of cholangiocarcinoma in PSC was 68% and 70%, respectively.49 Direct cholangioscopic visualization of strictures aids targeted biopsies and passage of otherwise-inaccessible strictures. A prospective study assessing cholangioscopy in 47 patients with PSC found adequate sample quality in 95% of miniforceps biopsies, with sensitivity, specificity, accuracy, and negative predictive value of 33%, 100%, 96%, and 95%, respectively.50
Endoscopic intervention is recommended in PSC for symptomatic patients with dominant BSs, as relief of biliary obstruction preserves hepatic function and may improve long-term survival.51,52 MRCP is recommended prior to ERCP to diagnose, locate, and characterize the dominant stricture. Routine prophylactic antibiotics are recommended before ERCP in patients with PSC to reduce the risk of cholangitis.52
Endoscopic therapy for PSC-related BBS involves either balloon or bougie dilatation with or without placement of a temporary plastic stent. In a multicenter randomized study of 65 patients with PSC and dominant strictures, the cumulative recurrence-free rate was similar for balloon dilatation and temporary stent placement (maximum 2 weeks, respectively, 0.30 vs 0.34 at 24 months; P=1). Adverse events, such as pancreatitis and cholangitis, were significantly more frequent in the stent group than the dilatation group (45% vs 6.7%, respectively; P=0.001), suggesting that balloon-dilatation monotherapy is the preferred initial therapy in patients with PSC and dominant strictures.53
Liver transplantation
BS after liver transplantation occurs at an incidence of 4%–43%, and may be classified as anastomotic or nonanastomotic.30 ABSs occur at the anastomotic site, typically as a single focal stricture and more frequently associated with living-donor livers than deceased-donor livers.3 Endoscopic therapy is effective and safe for ABS and the first-line treatment. Stricture dilatation followed by placement of multiple plastic biliary stents for ABS can achieve a high stricture resolution rate of 66.7%–100%, without the need for surgical intervention or retransplantation.3,54–56 Late-onset ABSs (≥6 months after transplantation) are likely to require more endoscopic interventions than those presenting in the early posttransplant period.57
Covered SEMSs are increasingly used to treat ABS. A multicenter, prospective, uncontrolled study of 22 patients with ABS showed temporary placement of a SEMS for 2 months achieved long-term stricture resolution in 52%.58 A prospective randomized trial comparing FCSEMS to multiple plastic stents for ABS found a comparable stricture-resolution rate, but fewer endoscopic procedures were required using FCSEMS (2 vs 4.5, respectively; P=0.0001).28 Similar results were found in another randomized controlled study of 162 patients, where the stricture-resolution rate in patients receiving FCSEMSs vs multiple plastic stents was 96.5% and 83%, respectively.59
NABSs are defined as those occurring ≥5 mm proximally to the anastomosis and are associated with ischemic events. NABSs are characterized by multiple extrahepatic and/or intrahepatic ABSs with recurrent sludge or stone formation.30 Late-onset NABS, defined as those presenting ≥1 year after liver transplantation, more commonly occur in the peripheral biliary tree. NABSs are more resistant to endoscopic therapy than ABSs, requiring more episodes of stricture dilatation and longer periods of stenting, with higher rates of stricture recurrence. Success rates following endoscopic therapy for NABS range from 40% to 82%.60,61
Surgical injury
LC is the most common cause of surgical bile-duct injury-related BBS, with an incidence of 0.5%.1 Traditional surgical repair, such as hepaticojejunostomy, was the preferred treatment of this type of postoperative BBS; however, endoscopic dilatation followed by placement of multiple plastic stents is an accepted alterative, with both techniques resulting in similar clinical success.
For example, in a retrospective comparison study of 66 patients treated by endoscopic stenting and 35 patients treated by surgical therapy for postoperative BBS, long-term success rates were similar, with stricture recurrence occurring in 17% in both groups.62 In another retrospective study of 42 patients with postcholecystectomy BBSs, excellent or good long-term outcomes were achieved in 77.3% (17 of 22) patients treated surgically and 80% (16 of 20) patients treated endoscopically.63
IgG4-sclerosing cholangitis
IgG4-associated cholangiopathy is an autoimmune inflammatory disease often associated with autoimmune pancreatitis and other systemic diseases. Patients may present with painless obstructive jaundice and intra- or extrahepatic strictures, which may mimic such conditions as PSC or cholangiocarcinoma (Figure 3). Corticosteroids are the first-line treatment of IgG4 cholangiopathy. In a prospective study of 23 patients with IgG4 cholangiopathy, a 100% response rate was reported after 6 weeks of prednisolone.64 In another study of 29 patients with symptomatic IgG4 cholangiopathy, 19 responded to steroids alone, 8 responded to steroids and biliary stenting, and 2 required operative therapy. These data suggest that in most cases, biliary stenting may be unnecessary, but may be useful if there is significant biliary obstruction or cholangitis, prior to corticosteroid therapy.
Biliary–enteric anastomotic stricture
ERCP is challenging in patients with surgically altered anatomy, such as Roux-en-Y hepaticojejunostomy, gastric bypass, or following Whipple’s procedures. Reasons include length of the afferent limb, acute angulation of anastomosis, and adhesions limiting bowel mobility. Use of colonoscopy or balloon enteroscopy may improve endoscopic access to the major papilla in such patients.65,66 Lack of an elevator on these scopes does limit cannulation ability, particularly when the papilla cannot be viewed not en face. Where available, the short-type double-balloon enteroscope is preferred, as its working length of 152 cm is compatible with most ERCP catheters.30
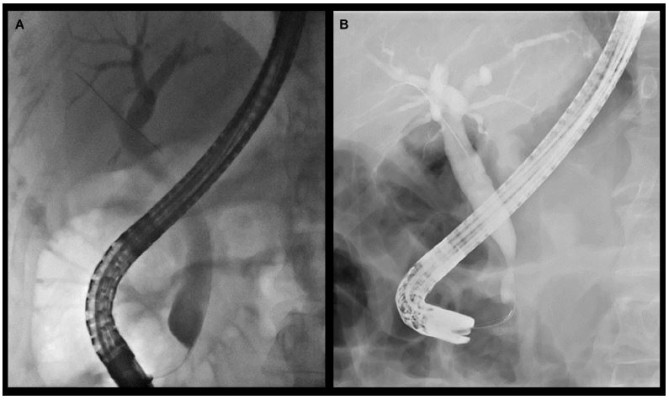
A meta-analysis of 15 studies showed overall success rates of 80.9% for single-balloon enteroscopy to reach the biliary anastomosis of papilla, 69.4% for obtaining a cholangiogram, and 61.7% for achieving successful biliary intervention.67 Adverse events occurred in 6.5% of procedures, including pancreatitis (2.2%), perforation (0.8%), and major bleeding (0.4%). In another systematic review that included 945 enteroscopy-assisted ERCP procedures, cannulation was achieved in 92% of patients with anastomosis, overall success was 74%, and adverse events occurred in 3.4%.68 Balloon dilatation is effective for most biliary enteric anastomotic strictures (Figure 4), as shown in a study of 34 patients where balloon dilatation resulted in clinical success in 66% of patients.36
Conclusion
BBSs may arise from a variety of etiologies. Symptomatic patients may present with jaundice and/or cholangitis, which are indications for treatment. Endoscopic therapy by ERCP is the first-line treatment for BBS, given its relative clinical efficacy, safety, and cost-effectiveness compared with other modalities, such as percutaneous cholangiography or surgery. Typically, this involves stricture dilatation using a balloon or bougie catheter, followed by placement of one or more plastic stents side by side. Recent evidence also supports the use of FCSEMSs to treat BBS as an alternative to multiple plastic stents.
Abbreviations
ABS, anastomotic biliary stricture; BS, biliary stricture; BBS, benign biliary stricture; CBD, common bile duct; CP, chronic pancreatitis; CT, computed tomography; ERCP, endoscopic retrograde cholangiopancreatography; FCSEMS, fully covered self-expanding metal stent; FISH, fluorescent in situ hybridization; LC, laparoscopic cholecystectomy; MRI, magnetic resonance imaging; MRCP, magnetic resonance cholangiopancreatography; NABS, nonanastomotic biliary stricture; PSC, primary sclerosing cholangitis; PTBD, percutaneous transhepatic biliary drainage; SEMS, self-expanding metal stent.
Disclosure
The authors report no conflicts of interest in this work.
References
Vitale GC, Tran TC, Davis BR, Vitale M, Vitale D, Larson G. Endoscopic management of postcholecystectomy bile duct strictures. J Am Coll Surg. 2008;206(5):918–923; discussion 924–925. | ||
Gómez CM, Dumonceau JM, Marcolongo M, et al. Endoscopic management of biliary complications after adult living-donor versus deceased-donor liver transplantation. Transplantation. 2009;88(11):1280–1285. | ||
Chan CH, Donnellan F, Byrne MF, et al. Response to endoscopic therapy for biliary anastomotic strictures in deceased versus living donor liver transplantation. Hepatobiliary Pancreat Dis Int. 2013;12(5):488–493. | ||
Lévy P, Barthet M, Mollard BR, Amouretti M, Marion-Audibert AM, Dyard F. Estimation of the prevalence and incidence of chronic pancreatitis and its complications. Gastroentérol Clin Biol. 2006;30(6–7):838–844. | ||
Wang LW, Li ZS, Li SD, Jin ZD, Zou DW, Chen F. Prevalence and clinical features of chronic pancreatitis in China: a retrospective multicenter analysis over 10 years. Pancreas. 2009;38(3):248–254. | ||
Suthar M, Purohit S, Bhargav V, Goyal P. Role of MRCP in differentiation of benign and malignant causes of biliary obstruction. J Clin Diagn Res. 2015;9(11):Tc08–Tc12. | ||
Navaneethan U, Njei B, Lourdusamy V, Konjeti R, Vargo JJ, Parsi MA. Comparative effectiveness of biliary brush cytology and intraductal biopsy for detection of malignant biliary strictures: a systematic review and meta-analysis. Gastrointest Endosc. 2015;81(1):168–176. | ||
Navaneethan U, Singh T, Gutierrez NG, et al. Predictors for detection of cancer in patients with indeterminate biliary stricture and atypical cells on endoscopic retrograde brush cytology. J Dig Dis. 2014;15(5):268–275. | ||
Kuroda Y, Tsuyuguchi T, Sakai Y, et al. Long-term follow-up evaluation for more than 10 years after endoscopic treatment for postoperative bile duct strictures. Surg Endosc. 2010;24(4):834–840. | ||
Walter D, Laleman W, Jansen JM, et al. A fully covered self-expandable metal stent with antimigration features for benign biliary strictures: a prospective, multicenter cohort study. Gastrointest Endosc. 2015;81(5):1197–1203. | ||
Devière J, Nageshwar Reddy D, Püspök A, et al. Successful management of benign biliary strictures with fully covered self-expanding metal stents. Gastroenterology. 2014;147(2):385–395; quiz e15. | ||
Perri V, Boškoski I, Tringali A, et al. Fully covered self-expandable metal stents in biliary strictures caused by chronic pancreatitis not responding to plastic stenting: a prospective study with 2 years of follow-up. Gastrointest Endosc. 2012;75(6):1271– 277. | ||
Harris A, Chan AC, Torres-Viera C, Hammett R, Carr-Locke D. Meta-analysis of antibiotic prophylaxis in endoscopic retrograde cholangiopancreatography (ERCP). Endoscopy. 1999;31(9):718–724. | ||
Bai Y, Gao F, Gao J, Zou DW, Li ZS. Prophylactic antibiotics cannot prevent endoscopic retrograde cholangiopancreatography induced cholangitis: a meta-analysis. Pancreas. 2009;38(2):126–130. | ||
Ishigaki T, Sasaki T, Serikawa M, et al. Evaluation of antibiotic use to prevent post-endoscopic retrograde cholangiopancreatography pancreatitis and cholangitis. Hepatogastroenterology. 2015;62(138):417–424. | ||
Woo YS, Lee JK, Noh DH, Park JK, Lee KH, Lee KT. SpyGlass cholangioscopy-assisted guidewire placement for post-LDLT biliary strictures: a case series. Surg Endosc. 2016;30(9):3897–3903. | ||
Zoepf T, Maldonado-Lopez EJ, Hilgard P, et al. Balloon dilatation vs. balloon dilatation plus bile duct endoprostheses for treatment of anastomotic biliary strictures after liver transplantation. Liver Transpl. 2006;12(1):88–94. | ||
Macías-Gómez C, Dumonceau JM. Endoscopic management of biliary complications after liver transplantation: an evidence-based review. World J Gastrointest Endosc. 2015;7(6):606–616. | ||
Peng C, Ma C, Xu G, Shen S, Lv Y, Zou X. The efficacy and safety of endoscopic balloon dilation combined with stenting in patients with biliary anastomotic strictures after orthotopic liver transplantation. Cell Biochem Biophys. 2015;72(2):385–397. | ||
Siiki A, Helminen M, Sand J, Laukkarinen J. Covered self-expanding metal stents may be preferable to plastic stents in the treatment of chronic pancreatitis-related biliary strictures: a systematic review comparing 2 methods of stent therapy in benign biliary strictures. J Clin Gastroenterol. 2014;48(7):635–643. | ||
Gotthardt DN, Rudolph G, Klöters-Plachky P, Kulaksiz H, Stiehl A. Endoscopic dilation of dominant stenoses in primary sclerosing cholangitis: outcome after long-term treatment. Gastrointest Endosc. 2010;71(3):527–534. | ||
van Boeckel PG, Vleggaar FP, Siersema PD. Plastic or metal stents for benign extrahepatic biliary strictures: a systematic review. BMC Gastroenterol. 2009;9(1):96. | ||
Parlak E, Dişibeyaz S, Ödemiş B, et al. Endoscopic treatment of patients with bile duct stricture after cholecystectomy: factors predicting recurrence in the long term. Dig Dis Sci. 2015;60(6):1778–1786. | ||
Brunet M, Blouin Y, Mosimann F. Biliary strictures after cholecystectomy: long term results of a novative endoscopic treatment. Hepatogastroenterology. 2014;61(136):2203–2208. | ||
Lawrence C, Romagnuolo J, Payne KM, Hawes RH, Cotton PB. Low symptomatic premature stent occlusion of multiple plastic stents for benign biliary strictures: comparing standard and prolonged stent change intervals. Gastrointest Endosc. 2010;72(3):558–563. | ||
Hirdes MM, Siersema PD, Houben MH, Weusten BL, Vleggaar FP. Stent-in- stent technique for removal of embedded esophageal self-expanding metal stents. Am J Gastroenterol. 2011;106(2):286–293. | ||
Haapamäki C, Kylänpää L, Udd M, et al. Randomized multicenter study of multiple plastic stents vs. covered self-expandable metallic stent in the treatment of biliary stricture in chronic pancreatitis. Endoscopy. 2015;47(7):605–610. | ||
Kaffes A, Griffin S, Vaughan R, et al. A randomized trial of a fully covered self-expandable metallic stent versus plastic stents in anastomotic biliary strictures after liver transplantation. Therap Adv Gastroenterol. 2014;7(2):64–71. | ||
Coté GA, Slivka A, Tarnasky P, et al. Effect of covered metallic stents compared with plastic stents on benign biliary stricture resolution: a randomized clinical trial. JAMA. 2016;315(12):1250–1257. | ||
Hu B, Sun B, Cai Q, et al. Asia-Pacific consensus guidelines for endoscopic management of benign biliary strictures. Gastrointest Endosc. 2017;86(1):44–58. | ||
Irani S, Baron TH, Akbar A, et al. Endoscopic treatment of benign biliary strictures using covered self-expandable metal stents (CSEMS). Dig Dis Sci. 2014;59(1):152–160. | ||
Saxena P, Diehl DL, Kumbhari V, et al. A US multicenter study of safety and efficacy of fully covered self-expandable metallic stents in benign extrahepatic biliary strictures. Dig Dis Sci. 2015;60(11):3442–3448. | ||
Tarantino I, Mangiavillano B, Di Mitri R, et al. Fully covered self-expandable metallic stents in benign biliary strictures: a multicenter study on efficacy and safety. Endoscopy. 2012;44(10):923–927. | ||
Park JK, Moon JH, Choi HJ, et al. Anchoring of a fully covered Self-Expandable metal stent with a 5F Double-Pigtail plastic stent to prevent migration in the management of benign biliary strictures. Am J gastroenterol. 2011;106:1761. | ||
Park DH, Lee SS, Lee TH, et al. Anchoring flap versus flared end, fully covered self-expandable metal stents to prevent migration in patients with benign biliary strictures: a multicenter, prospective, comparative pilot study (with videos). Gastrointest Endosc. 2011;73(1):64–70. | ||
Lee AY, Gregorius J, Kerlan RK, Gordon RL, Fidelman N. Percutaneous transhepatic balloon dilation of biliary-enteric anastomotic strictures after surgical repair of iatrogenic bile duct injuries. PLoS One. 2012;7(10):e46478. | ||
Ludwig JM, Webber GR, Knechtle SJ, Spivey JR, Xing M, Kim HS. Percutaneous management of benign biliary strictures with Large-Bore catheters: comparison between patients with and without orthotopic liver transplantation. J Vasc Interv Radiol. 2016;27(2):219–225. | ||
Gwon DI, Ko GY, Ko HK, Yoon HK, Sung KB. Percutaneous transhepatic treatment using retrievable covered stents in patients with benign biliary strictures: mid-term outcomes in 68 patients. Dig Dis Sci. 2013;58(11):3270–3279. | ||
Kahl S, Zimmermann S, Genz I, et al. Risk factors for failure of endoscopic stenting of biliary strictures in chronic pancreatitis: a prospective follow-up study. Am J Gastroenterol. 2003;98(11):2448–2453. | ||
Regimbeau JM, Fuks D, Bartoli E, et al. A comparative study of surgery and endoscopy for the treatment of bile duct stricture in patients with chronic pancreatitis. Surg Endosc. 2012;26(10):2902–2908. | ||
Tabibian JH, Asham EH, Goldstein L, et al. Endoscopic treatment with multiple stents for post-liver-transplantation nonanastomotic biliary strictures. Gastrointest Endosc. 2009;69(7):1236–1243. | ||
Jang SI, Lee KH, Yoon HJ, Lee DK. Treatment of completely obstructed benign biliary strictures with magnetic compression anastomosis: follow-up results after recanalization. Gastrointest Endosc. 2017;85(5):1057–1066. | ||
Hu B, Gao DJ, Wu J, Wang TT, Yang XM, Ye X. Intraductal radiofrequency ablation for refractory benign biliary stricture: pilot feasibility study. Dig Endosc. 2014;26(4):581–585. | ||
Mauri G, Michelozzi C, Melchiorre F, et al. Biodegradable biliary stent implantation in the treatment of benign bilioplastic-refractory biliary strictures: preliminary experience. Eur Radiol. 2013;23(12):3304–3310. | ||
Siiki A, Sand J, Laukkarinen J. A systematic review of biodegradable biliary stents: promising biocompatibility without stent removal. Eur J Gastroenterol Hepatol. 2018;30(8):813–818. | ||
Familiari P, Boškoski I, Bove V, Costamagna G. ERCP for biliary strictures associated with chronic pancreatitis. Gastrointest Endosc Clin N Am. 2013;23(4):833–845. | ||
Perri V, Boškoski I, Tringali A, et al. Fully covered self-expandable metal stents in biliary strictures caused by chronic pancreatitis not responding to plastic stenting: a prospective study with 2 years of follow-up. Gastrointest Endosc. 2012;75(6):1271–1277. | ||
Trikudanathan G, Navaneethan U, Njei B, Vargo JJ, Parsi MA. Diagnostic yield of bile duct brushings for cholangiocarcinoma in primary sclerosing cholangitis: a systematic review and meta-analysis. Gastrointest Endosc. 2014;79(5):783–789. | ||
Navaneethan U, Njei B, Venkatesh PG, Vargo JJ, Parsi MA. Fluorescence in situ hybridization for diagnosis of cholangiocarcinoma in primary sclerosing cholangitis: a systematic review and meta-analysis. Gastrointest Endosc. 2014;79(6):943–950. | ||
Arnelo U, von Seth E, Bergquist A. Prospective evaluation of the clinical utility of single-operator peroral cholangioscopy in patients with primary sclerosing cholangitis. Endoscopy. 2015;47(8):696–702. | ||
Thosani N, Banerjee S. Endoscopic retrograde cholangiopancreatography for primary sclerosing cholangitis. Clin Liver Dis. 2014; 8(4):899–911. | ||
Aabakken L, Karlsen TH, Albert J, et al. Role of endoscopy in primary sclerosing cholangitis: European Society of Gastrointestinal Endoscopy (ESGE) and European Association for the Study of the Liver (EASL) clinical guideline. Endoscopy. 2017;49(6):588–608. | ||
Ponsioen CY, Arnelo U, Bergquist A, et al. No superiority of stents vs balloon dilatation for dominant strictures in patients with primary sclerosing cholangitis. Gastroenterology. 2018;155(3):752–759. | ||
Poley JW, Lekkerkerker MN, Metselaar HJ, Kuipers EJ, Bruno MJ. Clinical outcome of progressive stenting in patients with anastomotic strictures after orthotopic liver transplantation. Endoscopy. 2013;45(7):567–570. | ||
Kurita A, Kodama Y, Minami R, et al. Endoscopic stent placement above the intact sphincter of oddi for biliary strictures after living donor liver transplantation. J Gastroenterol. 2013;48(9):1097–1104. | ||
Hsieh TH, Mekeel KL, Crowell MD, et al. Endoscopic treatment of anastomotic biliary strictures after living donor liver transplantation: outcomes after maximal stent therapy. Gastrointest Endosc. 2013;77(1):47–54. | ||
Verdonk RC, Buis CI, Porte RJ, et al. Anastomotic biliary strictures after liver transplantation: causes and consequences. Liver Transpl. 2006;12(5):726–735. | ||
Chaput U, Scatton O, Bichard P, et al. Temporary placement of partially covered self-expandable metal stents for anastomotic biliary strictures after liver transplantation: a prospective, multicenter study. Gastrointest Endosc. 2010;72(6):1167–1174. | ||
Martins FP, de Paulo GA, Contini ML, Ferrari AP. Metal versus plastic stents for anastomotic biliary strictures after liver transplantation: a randomized controlled trial. Gastrointest Endosc. 2018;87(1):131.e1–e13. | ||
Chang JH, Lee IS, Choi JY, et al. Biliary stricture after adult right-lobe living-donor liver transplantation with duct-to-duct anastomosis: long-term outcome and its related factors after endoscopic treatment. Gut Liver. 2010;4(2):226–233. | ||
Ryu CH, Lee SK. Biliary strictures after liver transplantation. Gut Liver. 2011;5(2):133–142. | ||
Davids PH, Tanka AK, Rauws EA, et al. Benign biliary strictures surgery or endoscopy? Ann Surg. 1993;217(3):237–243. | ||
Tocchi A, Mazzoni G, Liotta G, et al. Management of benign biliary strictures: biliary enteric anastomosis vs endoscopic stenting. Arch Surg. 2000;135(2):153–157. | ||
Sandanayake NS, Church NI, Chapman MH, et al. Presentation and management of post-treatment relapse in autoimmune pancreatitis/immunoglobulin G4-associated cholangitis. Clin Gastroenterol Hepatol. 2009;7(10):1089–1096. | ||
Ishii K, Itoi T, Tonozuka R, et al. Balloon enteroscopy-assisted ERCP in patients with Roux-en-Y gastrectomy and intact papillae (with videos). Gastrointest Endosc. 2016;83(2):377–386. | ||
Itokawa F, Itoi T, Ishii K, Sofuni A, Moriyasu F. Single- and double-balloon enteroscopy-assisted endoscopic retrograde cholangiopancreatography in patients with Roux-en-Y plus hepaticojejunostomy anastomosis and Whipple resection. Dig Endosc. 2014;26(Suppl 2):136–143. | ||
Inamdar S, Slattery E, Sejpal DV, et al. Systematic review and meta-analysis of single-balloon enteroscopy-assisted ERCP in patients with surgically altered GI anatomy. Gastrointest Endosc. 2015;82(1):9–19. | ||
Skinner M, Popa D, Neumann H, Wilcox C, Mönkemüller K. ERCP with the overtube-assisted enteroscopy technique: a systematic review. Endoscopy. 2014;46(7):560–572. |
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.