Back to Journals » Clinical Interventions in Aging » Volume 17
Barriers and Enablers to the Use of Web-Based Applications for Older Adults and Their Caregivers Post-Hip Fracture Surgery: A Descriptive Qualitative Study
Authors Backman C , Papp S, Harley A, Houle S , Mamo Y, Poitras S, Shah S, Berdusco R, Beaulé PE , French-Merkley V
Received 3 August 2022
Accepted for publication 22 October 2022
Published 16 November 2022 Volume 2022:17 Pages 1635—1645
DOI https://doi.org/10.2147/CIA.S384822
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Maddalena Illario
Chantal Backman,1– 3 Steve Papp,4,5 Anne Harley,5,6 Sandra Houle,7 Yeabsira Mamo,1 Stephane Poitras,7 Soha Shah,5,6 Randa Berdusco,4,5 Paul E Beaulé,4,5 Veronique French-Merkley5,6
1School of Nursing, Faculty of Health Sciences, University of Ottawa, Ottawa, Canada; 2Ottawa Hospital Research Institute, Ottawa, Canada; 3Bruyère Research Institute, Ottawa, Canada; 4Department of Orthopaedics, The Ottawa Hospital, Ottawa, Canada; 5Faculty of Medicine, University of Ottawa, Ottawa, Canada; 6Geriatric Rehabilitation, Bruyère Continuing Care, Ottawa, Canada; 7Rehabilitation Sciences, Faculty of Health Sciences, University of Ottawa, Ottawa, Ontario, Canada
Correspondence: Chantal Backman, 451, Smyth Road, RGN 3239, Ottawa, ON, K1H 8M5, Canada, Tel +1 613-562-5800 ext. 8418, Email [email protected]
Purpose: The purpose of this study was to describe the barriers and enablers to the use of web-based applications designed to help manage the personalized needs of older adults and their caregivers post-hip fracture surgery while transitioning from hospital to geriatric rehabilitation to home.
Methods: This was a descriptive qualitative study consisting of semi-structured interviews informed by the Theoretical Domains Framework. The study took place between March 2021 and April 2022 on an orthopaedic unit in a large academic health sciences centre and in a geriatric rehabilitation service in Ontario, Canada. The transcripts were analyzed using a systematic 6-step approach.
Results: Interviews were conducted with older adults (n = 10) and with caregivers (n = 8) post-hip fracture surgery. A total of 21 barriers and 24 enablers were identified. The top two barriers were a need for basic computer skills (n = 11, 61.1%) and a preference for direct verbal communication (n = 10, 55.6%). The top two enablers were having no concerns with using web-based applications (n = 12, 66.7%) and having ease of access to information (n = 10, 55.6%).
Conclusion: We described the key barriers and enablers to the use of web-based applications from the perspectives of older adults and their caregivers. These factors will inform further developments of web-based applications aimed at improving the care transition from hospital to geriatric rehabilitation to home post-hip fracture surgery.
Keywords: hip fracture, digital health intervention, web-based application, TDF, older adults
Background
Experiencing a hip fracture is often an alarming and life-altering event in the lives of older adults and their families. Hip fractures are associated with high mortality and morbidity rates, as well as reduced activity level, persistent fear of falling, and increased isolation.1,2 Following hip fracture surgery, many care interventions across multiple health care settings are initiated.1,3 These can include screening for delirium, deep vein thrombosis, pressure wounds and osteoporosis, as well as rehabilitation interventions (ie physiotherapy, occupational therapy) geared toward regaining pre-fracture function.1
Given the complex set of interventions post-hip fracture, it is of little surprise that patients and their families report feeling insecure and uncertain of what they can expect after a hip fracture.4,5 The exchange and integration of information can be especially difficult for patients given the shock of the accident, the surgical procedure, and the fast-paced interactions with team members in hospital and rehabilitation centers.5 Furthermore, older adults with a hip fracture may have a diagnosis of cognitive impairment resulting in a reduction in how they process and retain the information.6 Verbal instructions, especially, are likely not retained correctly.7 Caregivers are often key to supporting hip fracture patients during the transition from hospital to geriatric rehabilitation to home.8 Yet, caregivers may also feel overwhelmed, and unsure of how to provide support after a hip fracture.5 However, both patients and caregivers report a strong desire to take charge of their situation and to be actively involved in their recovery.4 Providing opportunities for engagement in managing one’s care, and empowering hip fracture patients and their caregivers through better access to relevant health care information such as patient education, discharge information, and reminders for required follow-ups have been identified as priorities for this population.5
Digital health interventions have the potential to optimize the quality of communication and accessibility of information for stakeholders in health care settings, thereby empowering patients and their caregivers in the management of their care.9,10 Digital health interventions are defined by the World Health Organization as “a discrete functionality of digital technology that is applied to achieve health objectives” (p.iii).9 According to a recent scoping review of digital health interventions, they are most often utilized for the transmission of health information, receiving real-time support from care providers, personal health tracking, remote healthcare services, and peer support.11 Digital health interventions, specifically web-based applications, have been used successfully to facilitate and optimize interdisciplinary care for a variety of patients including those with cardiac disease,12,13 diabetes,14,15 and other chronic conditions.16,17 Specifically for hip fracture patients, web-based applications can improve education and information comprehension, quality of life, psychological wellness and support the return to pre-fracture fitness levels.18,19
Despite the potential benefits of web-based applications, factors related to capability, access, motivation, and other individual circumstances of patients and their caregivers can impact the successful use of these interventions.20 Low uptake of technology interventions, specifically by older adults who have experienced a hip fracture may be related to decreased self-efficacy, lack of familiarity with technology, or acceptability of such interventions.21 Yet, the feasibility of web-based applications with older adults has been previously demonstrated,22,23 especially by using a holistic, integrative approaches that include the active participation of patient networks including caregivers and care providers.20
The purpose of this study was to describe the barriers and enablers to the use of web-based applications designed to help manage the personalized needs of older adults and their caregivers post-hip fracture surgery while transitioning from hospital to geriatric rehabilitation to home. This work will help inform further development of a web-based application, MyPath to Home.24
Methods
Study Design and Setting
This was a descriptive qualitative study consisting of semi-structured interviews guided by the Theoretical Domains Framework (TDF).25 This study took place between March 2021 and April 2022 in an orthopaedic unit in a large academic health sciences centre and a geriatric rehabilitation service in Ontario, Canada. Research Ethics Board (REB) approvals were obtained prior to the start of the study. This study complied with the principles of the Declaration of Helsinki.
Theoretical Framework
We chose to explore implementation research and identified the TDF as a robust and interactive framework, useful for behaviour change research.25 The TDF includes 14 theoretical domains synthesizing 33 behaviour change theories.26–28 The TDF and its specific domains have been validated for use in implementation and behaviour change studies.29
For our study, we described the behaviour in terms of the target, action, context, time actor (TACT-A) principle30 as follows: target (older adults and their caregivers post-hip fracture surgery), action (use of web-based applications to help manage their personalized needs), context (hospital, geriatric rehabilitation, and home), time (entire episode of care), and actor (hip fracture patients and caregivers). We developed similar but separate interview guides for geriatric hip fracture patients and for caregivers.
Eligibility Criteria
We used a convenience sampling technique to recruit hip fracture patients and caregivers. Patients were eligible to participate based on the following criteria: (a) post-hip fracture surgery, (b) > 65 years of age, (c) able to consent to participate. Patients with aphasia, significant cognitive impairment or receiving palliative care were excluded.
Caregivers were eligible if they were: (a) caring for a patient who had a hip fracture surgery, (b) >18 or older.
Recruitment and Data Collection
A designated person from the clinical care areas helped with the recruitment of the study participants. Individuals who expressed an interest in participating were asked to contact a trained research assistant who then further explained the study. After written or verbal informed consent was obtained (as approved by REB), audio recorded 30-minute semi-structured interviews following an interview guide took place either in person, by videoconference or by phone.
Data Analysis
Descriptive statistics were used to summarize the characteristics of the participants. Interviews were transcribed verbatim, and interviews were analyzed using a 6-step approach.31 First, two research assistants (YM, SH) independently coded the transcripts according to the relevant domains of the TDF. Any discrepancies were resolved through discussion until consensus was met. Second, specific belief statements were generated for the coded segments of text. Third, similar belief statements were grouped together. Fourth, themes were generated inductively from the grouped belief statements (defined as a similar statement mentioned by two or more individuals). Fifth, each theme was classified as either a barrier or an enabler to using web-based applications. Sixth, themes were examined and the most frequent barriers and enablers specific to patients or to caregivers (reported by greater than 50%), as well as conflicting barriers and enablers, were identified. Frequency scores were calculated for the number of participants describing each barrier and enabler. Qualitative data analysis software (NVivo, QSR International Pty Ltd. Version 12) was used for data management.
Results
Patients and Caregivers’ Demographics
A total of 18 participants, including 10 patients and 8 caregivers were recruited based on the inclusion criteria previously described. Most patients were female (n=7) and were between the age of 75 and 84 (n=6). With regards to caregivers, an equal amount of male (n=4) and female (n=4) caregivers participated. Caregivers were aged between 45 and 84 years old, with the majority between 45–54 (n=3) or 65–74 (n=3) years of age. Caregivers were most often children (n=6) of the patient; however, spouses (n=2) were also included. Further details are provided in Table 1.
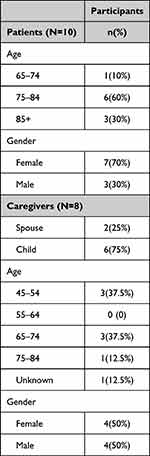 |
Table 1 Demographic Information (Patients and Caregivers) |
Patients’ and Caregivers’ Barriers
A total of 21 barriers were identified. The top barriers, which were identified by more than 50% of the participants, were a need for basic computer skills (n=11, 61.1%), and a preference for direct verbal communication (n=10, 55.6%). These barriers were expressed by both patients and caregivers.
The most frequent barriers voiced by patients, identified by more than 50% of the patients, were the preference for direct verbal communication (n=8, 80%), the need for basic computer skills (n=7, 70%), a lack of confidence with the use of web-based applications (n=6, 60%), the inability to use web-based applications due to age (n=6, 60%), and not finding the use of web-based applications important (n=6, 60%). No specific barriers were identified by more than 50% of the caregivers. Details of the complete list of barriers as well as example quotes are provided in Table 2.
 |
Table 2 Barriers to the Use of Web-Based Applications |
Patients’ and Caregivers’ Enablers
A total of 24 enablers were identified. The top enablers, identified by over 50% of the participants, were having no concerns with using web-based applications (n=12, 66.7%) and having ease of access to information (n=10, 55.6%). These enablers were also expressed by both patients and caregivers.
The most frequent patients’ enabler was no specific concerns or worries with using web-based applications (n=6, 60%). While no barriers were identified by more than 50% of the caregivers, a few enablers were identified, the most frequent being the caregivers’ intention to use web-based applications (n=8, 100%). Other frequent enablers included confidence with the use of web-based applications (n=7, 87.5%), the straightforward process to use web-based applications (n=7, 87.5%), the importance of using web-based applications (n=7, 87.5%), no concerns with the use of web-based applications (n=6, 75%), anticipating benefits of ease of access to information (n=6, 75%), and not anticipating any negative aspects to the use of web-based applications (n=6, 75%). Details of the enablers are provided in Table 3.
 |
Table 3 Enablers to the Use of Web-Based Applications |
Conflicting Themes
Several themes (n=5) were identified as both a barrier and an enabler. Some participants expressed a lack of confidence with the use of web-based applications (barrier) (n=6 patients, n=1 caregiver), while others were confident in using them (enabler) (n=4 patients, n=7 caregivers). Some participants found web-based applications not important to use (barrier) (n=7 patients) whereas others felt that they were important (enabler) (n=3 patients, n=7 caregivers). Some participants described having competing tasks or time constraints to using web-based applications (n=2 patients, n=2 caregivers) while others had no competing tasks or time constraints (enabler) (n=4 patients, n=3 caregivers). A few participants found that using web-based applications is not a straightforward process (barrier) (n=3 patients) whereas most found the process straightforward (enabler) (n=5 patients, n=7 caregivers). Some participants described having no intention to use web-based applications (barrier) (n=3 patients), while others have the intention to use them (enabler) (n=5 patients, n=8 caregivers).
Discussion
We identified 21 barriers and 24 enablers to the use of web-based applications for older adults and their caregivers post-hip fracture surgery. Our findings indicate that both patients and caregivers voiced similar concerns with the use of web-based applications including the need for basic computer skills (n=11, 61.1%), and a preference for direct verbal communication (n=10, 55.6%). They also shared top enablers such as having no concerns with using web-based applications (n=12, 66.7%) and having ease of access to information (n=10, 55.6%).
When considering patients and their caregivers separately, we found that patients reported more barriers and less enablers to the use of web-based applications, whereas caregivers more frequently reported enablers rather than barriers. Given, the higher age range of participant patients (ie, all patients (n=10) were over the age of 65 as per the eligibility criteria) compared to caregivers (ie, caregivers (n=3) were under the age of 55), this finding is congruent with studies’ results showing increasing barriers to technology with age.32 However, although the caregivers in our study were generally younger than patients, four were over the age of 65 which may explain why they voiced similar top barriers.
With regards to patients specifically, the most frequently reported barrier was the preference for direct verbal communication (n=8, 80%). The preference for face-to-face communication has been reported by patients in similar studies examining the use of digital health interventions by older adults.20,21,33 However, studies examining the effectiveness of different modes of communication in healthcare settings, have found that verbal instructions are often remembered incorrectly, if at all, by patients.7 Indeed, participants in our study (n=3 patients, n=4 caregivers) identified the opportunity for written instructions in the web-based application as an incentive to use, and described web-based applications as having the potential to improve overall communication with their healthcare providers (n=1 patient, n=4 caregivers).
Overall, patients more frequently expressed belief statements indicating low motivation for using web-based applications than caregivers, such as not finding web-based applications important to use (n=7, 38.9%), and having no intention of using a web-based application (n=3, 16.7%). Morris et al21 found that acceptability and uptake of digital technology by older adults with hip fractures were negatively impacted by low self-efficacy and lack of familiarity with technology. Indeed, three of the most important barriers for patients were the need for basic computer skills (n=7, 70%), a lack of confidence with the use of web-based applications (n=6, 60%), and the belief that one is unable to use web-based applications due to age (n=6, 60%). All these barriers fell within the TDF domains of skills and beliefs about capabilities, which was congruent with studies reporting low health literacy, low self-efficacy and a belief that age plays a major factor in being unable to use technology as being significant barriers for older adults.18,20,34–36
Stereotypes that depict all older adults as unable to use technology negatively impact the social participation of older adults and fail to pick up on nuances between individuals that can be addressed to improve digital participation.36 Although many older adults have lower baseline computer skill levels, many factors such as low confidence and anxiety surrounding technology can be addressed successfully through training and caregiver support.36
Supportive caregivers have been identified as key to successful transitions from acute care, to rehabilitation, to home,8 and specifically for using digital health interventions.37 Similarly, in this study, patients and caregivers described having social support to use web-based applications (n=7, 38.9%) and having a positive social influence to using web-based applications (n=6, 33.3%). Other studies have also shown that support from caregivers is crucial.38–40
The results of this study will inform further development of MyPath to Home,24 a web-based application to support older adults and their caregivers as they manage their personalized needs during their transition from the hospital, to rehabilitation, to home. Specifically, the barriers and enablers analysis will inform the intervention strategy. We will select the evidence-based behaviour change techniques (BCTs)27 that align with the barriers and enablers identified in this study. For example, some of these BCTs to tackle the two top barriers will include training on basic computer skills and the use of incentives for patients and caregivers to access a combination of direct verbal communication from providers with supplemental web-based (including video and written) information. These BCTs will be incorporated in the next iteration of MyPath to Home24 intervention for evaluation in a future research study.
Strengths and Limitations
Overall, this study has several strengths and limitations. It was guided by the TDF framework which was used for data collection and analysis. Our recruitment was slow due to the COVID outbreaks experienced on the study units. Although our sample size was relatively small, our study included both the patients and caregivers’ perspectives. It is possible that those who refused to participate were even more unfamiliar with web-based applications. Further studies should also be conducted to understand the barriers and enablers from the providers’ perspectives and how these web-based applications may affect their work processes.
Conclusion
This study identified the key barriers and enablers to the use of web-based applications from the perspectives of older adults and their caregivers. This research will directly inform how web-based applications can be incorporated into everyday clinical practice to help improve care transition experience, preparedness for discharge, and coping after discharge for older adults and their caregivers post-hip fracture surgery. It can also improve system efficiencies (such as readmissions, and sub-optimal care leading to complications), optimizing the transitions between health care sectors. By addressing the barriers and leveraging the enablers identified, we may see the benefits of tailoring web-based applications to meet the needs of patients and their caregivers as well as improve the uptake of these digital health interventions.
Data Sharing Statement
No additional data are available.
Ethics Approval and Consent to Participate
Approval was obtained from the Ottawa Health Science Network Research Ethics Board (#20180469-01H), the Bruyère Continuing Care Research Ethics Board (#M16-18-03) and the University of Ottawa Health Sciences and Sciences Research Ethics Board (#H-08-18-1061).
Acknowledgments
We would like to thank all the patients and caregivers who participated in our study.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was supported by operational funding from the University of Ottawa.
Disclosure
Dr Veronique French-Merkley reports grants from Ontario Ministry of Health, during the conduct of the study. The authors report no conflicts of interest in this work.
References
1. Health Quality Ontario. Hip fracture: care for people with fragility fractures. Health Quality Ontario; 2022. Available from: https://www.hqontario.ca/evidence-to-improve-care/quality-standards/view-all-quality-standards/hip-fracture.
2. Zidén L, Scherman MH, Wenestam CG. The break remains – elderly people’s experiences of a hip fracture 1 year after discharge. Disabil Rehabil. 2010;32(2):103–113. doi:10.3109/09638280903009263
3. Pitzul KB, Wodchis WP, Carter MW, Kreder HJ, Voth J, Jaglal SB. Post-acute pathways among hip fracture patients: a system-level analysis. BMC Health Serv Res. 2016;16:275. doi:10.1186/s12913-016-1524-1
4. Jensen CM, Smith AC, Overgaard S, Wiil UK, Clemensen J. ”If only had I known”: a qualitative study investigating a treatment of patients with a hip fracture with short time stay in hospital. Int J Qual Stud Health Well-Being. 2017;12(1):1307061. doi:10.1080/17482631.2017.1307061
5. Jensen CM, Overgaard S, Wiil UK, Smith AC, Clemensen J. Bridging the gap: a user-driven study on new ways to support self-care and empowerment for patients with hip fracture. SAGE Open Med. 2018;6:2050312118799121. doi:10.1177/2050312118799121
6. Seitz DP, Adunuri N, Gill SS, Rochon PA. Prevalence of dementia and cognitive impairment among older adults with hip fractures. J Am Med Dir Assoc. 2011;12(8):556–564. doi:10.1016/j.jamda.2010.12.001
7. Rao M, Fogarty P. What did the doctor say? J Obstetr Gynecol. 2009;27(5):479–480. doi:10.1080/01443610701405853
8. Elliott J, Forbes D, Chesworth BM, Ceci C, Stolee P. Information sharing with rural family caregivers during care transitions of hip fracture patients. Int J Integr Care. 2014;14:e018. doi:10.5334/ijic.1195
9. World Health Organization. WHO Guideline: Recommendations on Digital Interventions for Health System Strengthening. Geneva: World Health Organization; 2019. Licence: CC BY-NC-SA 3.0 IGO.
10. Coulter A, Ellins J. Effectiveness of strategies for informing, educating, and involving patients. BMJ. 2007;335(7609):24–27. doi:10.1136/bmj.39246.581169.80
11. Zhang J, Yang M, Ge Y, Ivers R, Webster R, Tian M. The role of digital health for post-surgery care of older patients with hip fracture: a scoping review. Int J Med Inform. 2022;160:104709. doi:10.1016/j.ijmedinf.2022.104709
12. Ramachandran HJ, Jiang Y, Teo JYC, Yeo TJ, Wang W. Technology acceptance of home-based cardiac telerehabilitation programs in patients with coronary heart disease: systematic scoping review. J Med Internet Res. 2022;24(1):e34657. doi:10.2196/34657
13. Hale TM, Jethwani K, Kandola MS, Saldana F, Kvedar JC. A remote medication monitoring system for chronic heart failure patients to reduce readmissions: a two-arm randomized pilot study. J Med Internet Res. 2016;18(4):e91. doi:10.2196/jmir.5256
14. Lee PA, Greenfield G, Pappas Y. Patients’ perception of using telehealth for type 2 diabetes management: a phenomenological study. BMC Health Serv Res. 2018;18(1):549. doi:10.1186/s12913-018-3353-x
15. Cafazzo JA, Casselman M, Hamming N, Katzman DK, Palmert MR. Design of an mHealth app for the self-management of adolescent type 1 diabetes: a pilot study. J Med Internet Res. 2012;14(3):e70. doi:10.2196/jmir.2058
16. Tenforde AS, Hefner JE, Kodish-Wachs JE, Iaccarino MA, Paganoni S. Telehealth in physical medicine and rehabilitation: a narrative review. PM R. 2017;9(5S):S51–S58. doi:10.1016/j.pmrj.2017.02.013
17. Chehade MJ, Yadav L, Jayatilaka A, Gill TK, Palmer E. Personal digital health hubs for multiple conditions. Bull World Health Organ. 2020;98(8):569–575. doi:10.2471/BLT.19.249136
18. Jensen CM, Overgaard S, Wiil UK, Clemensen J. Can tele-health support self-care and empowerment? A qualitative study of hip fracture patients’ experiences with testing an “app”. SAGE Open Nurs. 2019;5:2377960819825752. doi:10.1177/2377960819825752
19. Mora-Traverso M, Prieto-Moreno R, Molina-Garcia P, et al. Effects of the @ctivehip telerehabilitation program on the quality of life, psychological factors and fitness level of patients with hip fracture [published online ahead of print, 2022 Jan 21]. J Telemed Telecare. 2022;1357633X211073256. doi:10.1177/1357633X211073256
20. Yadav L, Gill TK, Taylor A, De Young J, Chehade MJ. Identifying opportunities, and motivation to enhance capabilities, influencing the development of a personalized digital health hub model of care for hip fractures: mixed methods exploratory study. J Med Internet Res. 2021;23(10):e26886. doi:10.2196/26886
21. Morris C, Van den Berg M, Barr C, George S, Crotty M. Demographic characteristics and functional levels of patients with fragility fractures who accept tele-rehabilitation as an alternative to face-to-face home rehabilitation. Home Health Care Manag Pract. 2021;33(3):171–176. doi:10.1177/1084822320983314
22. Crotty M, Killington M, van den Berg M, Morris C, Taylor A, Carati C. Telerehabilitation for older people using off-the-shelf applications: acceptability and feasibility. J Telemed Telecare. 2014;20(7):370–376. doi:10.1177/1357633X14552382
23. Shulver W, Killington M, Morris C, Crotty M. ‘Well, if the kids can do it, I can do it’: older rehabilitation patients’ experiences of telerehabilitation. Health Expect. 2017;20(1):120–129. doi:10.1111/hex.12443
24. Backman C, Harley A, Kuziemsky C, Mercer J, Peyton L. MyPath to home web-based application for the geriatric rehabilitation program at bruyère continuing care: user-centered design and feasibility testing study. JMIR Form Res. 2020;4(9):e18169. doi:10.2196/18169
25. Michie S, Johnston M, Abraham C, et al. Making psychological theory useful for implementing evidence based practice: a consensus approach. Qual Saf Health Care. 2005;14(1):26–33. doi:10.1136/qshc.2004.011155
26. Atkins L, Francis J, Islam R, et al. A guide to using the Theoretical Domains Framework of behaviour change to investigate implementation problems. Implement Sci. 2017;12(1):77. doi:10.1186/s13012-017-0605-9
27. Michie S, Atkins L, West R. The Behaviour Change Wheel. A Guide to Designing Interventions.
28. Francis JJ, Stockton C, Eccles MP, et al. Evidence-based selection of theories for designing behaviour change interventions: using methods based on theoretical construct domains to understand clinicians’ blood transfusion behaviour. Br J Health Psychol. 2009;14(Pt 4):625–646. doi:10.1348/135910708X397025
29. Cane J, O’Connor D, Michie S. Validation of the theoretical domains framework for use in behaviour change and implementation research. Implement Sci. 2012;7:37. doi:10.1186/1748-5908-7-37
30. Francis JJ, Presseau J. Healthcare practitioner behaviour. In: Llewellyn C, Ayers S, McManus C, et al., editors. Cambridge Handbook of Psychology, Health and Medicine.
31. Squires JE, Graham N, Coughlin M, et al. Barriers and enablers to organ donation after circulatory determination of death: a qualitative study exploring the beliefs of frontline intensive care unit professionals and organ donor coordinators. Transplant Direct. 2018;4(7):e368. doi:10.1097/TXD.0000000000000805
32. Lee B, Chen Y, Hewitt L. Age differences in constraints encountered by seniors in their use of computers and the internet. Comput Human Behav. 2011;27(3):1231–1237. doi:10.1016/j.chb.2011.01.003
33. Reed ME, Huang J, Graetz I, et al. Patient characteristics associated with choosing a telemedicine visit vs office visit with the same primary care clinicians. JAMA Netw Open. 2020;3(6):e205873. doi:10.1001/jamanetworkopen.2020.5873
34. Jørgensen BB, Gregersen M, Pallesen SH, Damsgaard EM. A group-based real-time videoconferencing telerehabilitation programme in recently discharged geriatric patients: a feasibility study. Eur Geriatr Med. 2021;12(4):801–808. doi:10.1007/s41999-020-00444-6
35. Yadav L, Gill TK, Taylor A, deYoung J, Visvanathan R, Chehade MJ. ”Context, content, and system” supporting digital health hub (DHH)-enabled models of care (MoCs) for fragility Hip fractures: perspectives of diverse multidisciplinary stakeholders in South Australia from qualitative in-depth interviews. Arch Osteoporos. 2021;16(1):167. doi:10.1007/s11657-021-01031-3
36. Barrie H, La Rose T, Detlor B, Julien H, Serenko A. “Because I’m Old”: the role of ageism in older adults’ experiences of digital literacy training in public libraries. J Technol Hum Serv. 2021;39(4):379–404. doi:10.1080/15228835.2021.1962477
37. Ortiz-Piña M, Molina-Garcia P, Femia P, et al. Effects of tele-rehabilitation compared with home-based in-person rehabilitation for older adult’s function after hip fracture. Int J Environ Res Public Health. 2021;18(10):5493. doi:10.3390/ijerph18105493
38. Ariza-Vega P, Castillo-Pérez H, Ortiz-Piña M, Ziden L, Palomino-Vidal J, Ashe MC. The journey of recovery: caregivers’ perspectives from a hip fracture telerehabilitation clinical trial. Phys Ther. 2021;101(3):pzaa220. doi:10.1093/ptj/pzaa220
39. Geerds MAJ, Nijmeijer WS, Hegeman JH, Vollenbroek-Hutten MMR. Mobile app for monitoring 3-month postoperative functional outcome after hip fracture: usability study. JMIR Hum Factors. 2020;7(3):e16989. doi:10.2196/16989
40. Li CT, Hung GK, Fong KN, Gonzalez PC, Wah SH, Tsang HW. Effects of home-based occupational therapy telerehabilitation via smartphone for outpatients after hip fracture surgery: a feasibility randomised controlled study. J Telemed Telecare. 2022;28(4):239–247. doi:10.1177/1357633X20932434
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
