Back to Journals » Therapeutics and Clinical Risk Management » Volume 14
Balancing intubation time with postoperative risk in cardiac surgery patients – a retrospective cohort analysis
Authors Kotfis K , Szylińska A , Listewnik M , Lechowicz K , Kosiorowska M, Drożdżal S, Brykczyński M , Rotter I , Żukowski M
Received 4 August 2018
Accepted for publication 15 September 2018
Published 5 November 2018 Volume 2018:14 Pages 2203—2212
DOI https://doi.org/10.2147/TCRM.S182333
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Garry Walsh
Katarzyna Kotfis,1 Aleksandra Szylińska,2 Mariusz Listewnik,3 Kacper Lechowicz,1 Monika Kosiorowska,3 Sylwester Drożdżal,1 Mirosław Brykczyński,3 Iwona Rotter,2 Maciej Żukowski1
1Department of Anesthesiology, Intensive Therapy and Acute Intoxications, Pomeranian Medical University, Szczecin, Poland; 2Department of Medical Rehabilitation and Clinical Physiotherapy, Pomeranian Medical University, Szczecin, Poland; 3Department of Cardiac Surgery, Pomeranian Medical University, Szczecin, Poland
Introduction: Intubation time in patients undergoing cardiac surgery may be associated with increased mortality and morbidity. Premature extubation can have serious adverse physiological consequences. The aim of this study was to determine the influence of intubation time on morbidity and mortality in patients undergoing cardiac surgery.
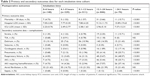
Methods: We performed a retrospective analysis of data on 1,904 patients undergoing isolated coronary artery bypass grafting (CABG) and stratified them by duration of intubation time after surgery – 0–6, 6–9, 9–12, 12–24 and over 24 hours. Postoperative complications risk analysis was performed using multivariate logistic regression analysis for patients extubated ≤12 and >12 hours.
Results: Intubation percentages in each time cohort were as follows: 0–6 hours – 7.8%, 6–9 hours – 17.3%, 9–12 hours – 26.8%, 12–24 hours – 44.4% and >24 hours – 3.7%. Patients extubated ≤12 hours after CABG were younger, mostly males, more often smokers, with lower preoperative risk. They had lower 30-day mortality (2.02% vs 4.59%, P=0.002), shorter hospital stay (7.68±4.49 vs 9.65±12.63 days, P<0.001) and shorter intensive care unit stay (2.39 vs 3.30 days, P<0.001). Multivariate analysis showed that intubation exceeding 12 hours after CABG increases the risk of postoperative delirium (OR 1.548, 95% CI 1.161–2.064, P=0.003) and risk of postoperative hemofiltration (OR 1.302, 95% CI 1.023–1.657, P=0.032).
Conclusion: Results indicate that risk of postoperative complications does not increase until intubation time exceeds 12 hours. Shorter intubation time is seen in younger, men and smokers. Intubation time >12 hours is a risk factor for postoperative delirium and hemofiltration after cardiac surgery.
Keywords: intubation, cardiac surgery, CABG, mortality, complications, delirium
Introduction
Prolonged intubation time in patients undergoing cardiac surgery can be associated with increased mortality and morbidity.1–3 Studies have shown that patients extubated earlier after the operation have shorter ICU and hospital length of stay (LOS).4,5 The guidelines of the Society of Thoracic Surgeons (STS) indicate a 6-hour time point as a definition of “early extubation” and intubation longer than 24 hours as “prolonged intubation”.6 The advocated early extubation time, ie, within 6 hours after the procedure as compared to conventional extubation practices, has been associated with a reduced rate of infections, renal failure, stroke and mortality.7–9 However, the time between 6 and 24 hours has not been adequately studied. Dichotomization of patients into two sub-groups divided by a single time point may miss some of the important information regarding the intermediate time intervals. Advances in surgical and anesthetic techniques bring an on-going interest in early extubation in order to reduce the negative outcomes associated with delayed extubation, as well as any additional costs.10
Despite the advocated early 6-hour extubation time, many patients do not fulfill criteria for extubation at this time. One of the reasons is the cardiopulmonary bypass (CPB), responsible for inducing a generalized inflammatory response (complement and neutrophil activation, pro-inflammatory mediator release) that may result in the post-CPB syndrome characterized by an increase in alveolar–arterial oxygen partial pressure gradients (AaDO2), decreased lung compliance and increased extravascular lung water.11,12 Premature extubation can have serious adverse physiological consequences, including atelectasis, respiratory distress, hypercarbia and hypoxemia.13
Studies have reported numerous interventions and perioperative protocols aimed at meeting the 6-hour time point that were implemented in the cardiac ICUs as an effort to reduce the intubation time.14,15 The heterogeneity of patient populations undergoing cardiac surgery may have limited the success of previously suggested protocols and risk prediction models.16–19 The inflection point at which the complications rate rises has not been adequately determined. To verify the validity of previously identified predictors in a homogenous group of relatively low-risk patients, we performed this study with an aim to determine the influence of intubation duration on postoperative morbidity and mortality in patients undergoing isolated coronary artery bypass grafting (CABG) under general anesthesia.
Methods
Study design and patient selection
We performed a retrospective analysis of data from a prospectively collected institutional database including all operations performed at the Department of Cardiac Surgery of a tertiary university hospital with entries between January 1, 2014 and December 31, 2016. We included all patients undergoing isolated CABG, excluding any patients undergoing a valvular procedure performed in addition to CABG and all CABG without the use of cardio-pulmonary bypass (off-pump CABG [OPCAB]). Among 3,065 records in the database that included all cardiac surgery patients, we extracted data on 1,904 patients undergoing isolated CABG. Data on concomitant diseases and demographic information (age, gender, body mass index [BMI], history of smoking and admission type) were extracted from the medical documentation. The following co-morbidities were recorded: heart failure according to New York Heart Association (NYHA) and ejection fraction, arterial hypertension, myocardial infarction, atrial fibrillation, extracardiac arteriopathy, internal carotid artery stenosis, COPD, renal failure, stroke and transient ischemic attack. Perioperative risk was calculated using the EuroScore Logistics 2 scale. Laboratory results were part of routine perioperative blood sampling. Induction of general anesthesia was performed intravenously with fentanyl and etomidate, and a muscle relaxant (pancuronium) to allow tracheal intubation. Maintenance of general anesthesia was inhalational, using sevoflurane with additional doses of fentanyl and a muscle relaxant. After the surgery patients were transferred to a postoperative cardiac ICU, still intubated and mechanically ventilated, sedated to achieve adequate sedation depth (Richmond Agitation Sedation Scale [RASS] between −1 and +1) with adequate pain control, using intravenous morphine infusion and a non-opioid analgesic. The initial mode for mechanical ventilation was synchronized intermittent mechanical ventilation with continuous positive airway pressure when the patient regained their respiratory drive and the weaning process was initiated. Patients were extubated when they met pre-defined criteria: normal body temperature, Glasgow Coma Scale 14–15 points, no focal neurological deficit, pain under control, drainage <100 mL/h, hemodynamic stability (noradrenaline or adrenaline <0.05 μg/kg/min), absence of significant arrhythmias, PaO2 >60 mmHg, PaCO2 <45 mmHg, SpO2 >95% with FiO2 <0.45, no respiratory distress and normal respiratory rate. Patients were extubated to passive oxygen therapy (facial mask with O2 at 5–7 L/min). An arterial blood gas was obtained 30 minutes after extubation to ensure patient safety.
Ethical concerns
The study was performed in accordance with the Declaration of Helsinki due to its retrospective character a waiver was granted from the Bioethical Committee of the Pomeranian Medical University in Szczecin, Poland, decision no KB-0012/254/06/18. The data entered into the prospectively collected database required written informed consent for surgery, anesthesia and data collection at the time of hospital admission from each patient, as part of routine preoperative assessment, therefore patient consent to review their medical documentation was waived by the Bioethical Committee. To ensure patient data safety only de-identified data was used for analysis.
Intubation time cohorts
The intubation time (in hours, rounded to tenths) was calculated for each patient as a difference between the time when patient left the operating room to be transferred to the cardiac ICU and the time of extubation after the surgery and. We used five pre-defined time intervals of postoperative intubation: 0–6, 6–9, 9–12, 12–24 and over 24 hours. The time stratification approach indicated a threshold of 12-hours at which the risk of 30-day mortality increased, for which a complications risk analysis was performed.
Primary and secondary outcomes
The primary outcome was death within 30 days after the operation, regardless of the cause and ICU LOS (days) and hospital LOS (days). Secondary outcomes included postoperative complications – neurological (stroke, transient ischemic attack, delirium, seizures), respiratory (pneumonia, respiratory failure), renal (acute kidney injury, hemofiltration), cardiovascular (heart failure, cardiogenic shock, atrial fibrillation), and infectious (sepsis).
Statistical analyses
We performed descriptive analysis using the Student’s t-test for continuous variables, presented as means with SD according to distribution. The chi-squared test was used for categorical variables, which were presented as proportions. A mortality-matched analysis was performed for pre-defined time points (0–6, 6–9, 9–12, 12–24, and >24 hours), which showed a statistically significant mortality increase in patients intubated for longer than 12 hours and the whole cohort was further sub-divided into ≤12 hours and >12 hours. The P-value of <0.05 was regarded as statistically significant. Univariate logistic regression analysis was used for sub-groups ≤12 hours and >12 hours for each variable and presented as ORs with 95% CI. Risk factors that were significant in univariate analysis and presented with narrow CI and a P-value of <0.05 were manually entered for multivariate logistic regression analysis. All statistical analyses was performed using licensed software Statistica 12 (StatSoft, Inc., Tulsa, OK, USA), license no JPZP602C295824AR-V.
Results
Results for all time cohorts
The average intubation time after CABG was 14.93±8.63 hours. The intubation percentages in each time cohort were (Figure 1): 0–6 hours – 7.8% (148/1,904), 6–9 hours – 17.3% (329/1,904), 9–12 hours – 26.8% (511/1,904), 12–24 hours – 44.4% (846/1,904) and >24 hours – 3.7% (70/1,904). The majority of the patients were extubated within 12 hours – 52.5%. All data on patients with a stratification according to pre-defined time points are shown in Table 1. Age increase was seen across all five cohorts (P<0.001). Patients extubated earlier had higher BMI (P=0.032) were mostly men (P<0.001), more often smokers (P=0.003), with a lower operative risk (based on EuroScore logistic 2, P<0.001). The admission type did not differ between study cohorts. When accounting for concomitant diseases, patients extubated earlier had less heart failure (NYHA III and IV, P<0.001), less low ejection fraction <30% (P=0.023), less internal carotid artery stenosis (P=0.048), less chronic renal failure (P<0.001) and extracardiac arteriopathy (P=0.002) than patients with longer intubation times.
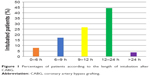  | Figure 1 Percentages of patients according to the length of intubation after CABG. |
Both primary and secondary outcomes data showed significant differences across all time cohorts (Table 2), with lower mortality (P<0.001) and shorter ICU (P<0.001) and hospital stay (P<0.001) for patients extubated earlier.
The differences in mortality across all five time cohorts for post-CABG intubation (Table 3) showed that the OR for mortality increases in patients intubated for longer than 12 hours (OR 2.831, 95% CI 1.216–6.594, P=0.016) and further increases if intubation time exceeded 24 hours (OR 8.514, 95% CI 3.283–22.079, P<0.001).
  | Table 3 Differences in 30-day mortality for different intubation time-points |
Results for patients with intubation times ≤12 and >12 hours
Patients extubated within 12 hours after intubation (52.4%, 998/1,904) were younger, mostly males (83.4% vs 72.4%, P<0.001), more often active smokers with lower preoperative risk as shown in Table 4. There were no differences regarding the BMI or the admission type between the two subgroups. When analyzing the comorbid conditions, only heart failure (NYHA III/IV) internal carotid artery stenosis and acute renal failure was more frequent in patients extubated >12 hours; preoperative hemoglobin was lower and serum creatinine was higher in these patients. The length of CPB and aortic cross-clamping time did not differ between ≤12-hour and >12-hour intubation times. The rate of reoperation (P<0.001) and intraoperative hemofiltration (P<0.001) was significantly higher in patients extubated after 12 hours. Patients intubated for longer than 12 hours had higher creatinine level at day 1 and required transfusion of more packed red blood cells, although the volume of postoperative drainage did not differ significantly between the two groups.
Patients intubated for longer than 12 hours had higher 30-day mortality (2.02% vs 4.59%, P=0.002), longer hospital LOS (9.65 vs 7.68 days, P<0.001) and longer ICU LOS (3.30 vs 2.39 days, P<0.001), but more patients had stroke (P<0.001), postoperative delirium (P<0.001), cardiogenic shock (P=0.003), pneumonia (P<0.001) and respiratory failure (P<0.001), acute kidney failure (P<0.001) and hemofiltration (P<0.001), as depicted in Table 5.
Univariate and multivariate analyses
Univariate analysis showed multiple factors to be associated with intubation exceeding 12 hours (Table 6), yet the multivariate analysis showed that intubation exceeding 12 hours after CABG did not increase the risk of 30-day mortality or length of ICU or hospital stay, but was associated only with increases in the occurrence of postoperative delirium (OR 1.580, 95% CI 1.188–2.102, P=0.003) and postoperative hemofiltration due to acute kidney injury (OR 1.302, 95% CI 1.023–1.657, P=0.032).
Discussion
The length of intubation and mechanical ventilation after cardiac surgery is a balance between the necessity to extubate the patient early to allow spontaneous breathing and regaining of respiratory independence and the risk of extubating too early and causing atelectasis and secondary respiratory failure and re-intubation.
The results of our pragmatic analysis indicate that the risk of postoperative complications does not increase until the intubation time exceeds 12 hours. The majority of the patients were extubated within 12 hours (52.5%) and only 3.7% remained intubated after 24 hours. Shorter intubation time was seen in younger patients, men, with higher BMI and more often in smokers. The multivariate analysis showed that intubation exceeding 12 hours after CABG does not increase the risk of 30-day mortality or length of ICU or hospital stay, but increases the occurrence of postoperative delirium and postoperative hemofiltration due to acute kidney injury.
Not surprisingly, shorter intubation time is seen in younger patients. Many studies reported that age is a significant predictor of delayed extubation with older patients having longer intubation times.20–23 In a study by Shahbazi and Kazerooni, age was the only predictive factor for delayed extubation.23 Suematsu et al has shown that age above 70 years was a predictor for delayed extubation time.22 In a study by Cislaghi et al, age above 65 years was associated with prolonged mechanical ventilation in patients undergoing cardiac surgery.20,21
Shorter intubation times in patients who are overweight or obese comply with the obesity paradox, with increasing BMI being a protective factor associated with improved outcome after cardiac surgery.24–26 According to Stamou et al, the hospital outcome and survival were better for overweight patients undergoing cardiac surgery when compared with patients with normal BMI.24 A cohort study and meta-analysis performed by Mariscalco et al showed that obesity was associated with lower risks for cardiac surgery patients, excluding reverse causation.25
This is the first study to show that intubation time is shorter in patients who are active smokers. Intuitively, smoking should be associated with worse postoperative outcome, being a risk factor for complications after cardiac surgery. It has been reported that cessation of smoking over 1 month prior to cardiac surgery may gradually improve ciliary function and macrophage phagocytic function, decrease the amount of sputum, resulting in the reduction of postoperative pulmonary complications in a few weeks.27,28 The relationship between smoking and extubation time in cardiac surgery was reported by Ji et al.29 Persistent smokers had a higher incidence of pulmonary complications following CABG when compared with non-smokers. Smoking cessation more than 1 month before surgery was expected to reduce early major morbidities following CABG surgery.29 Contrary to our findings, the smoking group in the study by Ji et al had a significantly higher incidence of postoperative pulmonary complications (7.1% vs 4.5%, P=0.0010) and significantly longer duration of mechanical ventilation (9.8±2.6 hour vs 9.4±2.4 hour, P<0.0001) when compared with the non-smoking group.29
Association with sex was also seen in many previous studies, indicating that men perform better after cardiac surgery.20 Studies have shown that female sex may be a non-modifiable risk factor for prolonged intubation after cardiac surgery.30
The rate of postoperative complications increases with the length of intubation time. According to Heringlake et al, postoperative intubation time prolongation was associated with AKI in cardiac surgical patients.31 Our results indicated that intubation exceeding 12 hours may be associated with AKI requiring hemofiltration (usually due to decreased diuresis and/or fluid overload). Oliver et al hypothesized that perioperative hemofiltration and steroids may attenuate the inflammatory response during CPB, but only hemofiltration reduced time to tracheal extubation for adults after CABG.32
This is the first study to show directly that the intubation time over 12 hours increases the risk of postoperative delirium, a well-recognized complication of cardiac surgery.33 Previous studies have shown that delirium was associated with prolonged ventilation time after cardiac surgery, but used a >24 hours intubation time-frame.34–36 Jannati et al reported that the ventilator time was associated with delirium during the first 24 hours after cardiac surgery.34 Kazmierski et al identified prolonged intubation as a risk factor for delirium, yet again this involved intubation >24 hours.35 Kobayashi et al indicated that intubation duration of 88.3±212.5 hours vs 37.2±92 hours (P=0.0296) was associated with delirium after CABG in patients aged over 75 years.36
Studies performed in the 1990s have shown that intubation exceeding 24 hours (prolonged intubation) is associated with increased mortality and morbidity after cardiac surgery.1,37,38 On the other side of the spectrum lies the shorter, 6-hour intubation time, associated with reduced risk of adverse postoperative events and decreased treatment cost.1,39 The intermediate period between 6 and 24 hours has not been adequately studied and it is still unclear, what is the ideal time above which the patient deteriorates and their outcome worsens. The 6-hour STS target seems arbitrary. Current guidelines of intubation times should be revisited allowing for more liberal length of postoperative intubation, less aggressive ventilation weaning and extubation after CABG. According to Camp et al, a 9-hour threshold was advocated.39 Crawford et al have shown that insignificant differences were observed in those extubated in 6–9 hours vs 0–6 hours nor in 9–12 hours vs 0–9 hours; an identical trend was observed for secondary outcomes of PLOS and reintubation.14 According to Crawford et al, a 12-hour benchmark for maximum duration of intubation may be advisable as the new target in the vulnerable population.14
The major limitation of this study is its retrospective character, although data were collected prospectively and not all data were available in the dataset. The multitude of factors that contribute to the duration of intubation after cardiac surgery makes this analysis difficult and prone to bias. The definite strength of our study is a very large number of patients included and the pragmatic evaluation of risk factors for intubation time points in patients undergoing one of the most common surgical interventions worldwide.
Conclusion
The results of this real-life analysis of intubation practices after CABG indicate that earlier extubation occurs in younger patients, males, and surprisingly in smokers. Intubation exceeding 12 hours does not increase the risk of 30-day mortality or hospital and ICU LOS, but is associated with the risk of postoperative delirium and AKI requiring hemofiltration. This study is another voice in the discussion about the new extubation metric that should guide both cardiac anesthetists and surgeons to stratify the risk of prolonged intubation after cardiac surgery and to allocate the resources.
Acknowledgment
The authors would like to thank the patients who provided the data for this study and nurses, physicians and physiotherapists who were involved in patient care at the Department of Cardiac Surgery and the Department of Anesthesiology, Intensive Therapy and Acute Intoxications at the Pomeranian Medical University in Szczecin, Poland.
Author contributions
KK provided the concept and design of the study, selection of the study group, collection of material, development and interpretation of research results, wrote the manuscript, collected literature, provided substantive supervision. AS was involved in the design of the study, performed statistical analysis, analyzed the results, was involved in revised the manuscript. ML designed the study, collected the data, analyzed the results, and provided critical revision of the manuscript. MK, KL, SD analyzed the results, collected literature and provided critical revision of the manuscript. MB, IR, and MŻ provided critical revision of the manuscript. All authors contributed to data analysis, drafting and revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflict of interest in this work.
References
Guller U, Anstrom KJ, Holman WL, Allman RM, Sansom M, Peterson ED. Outcomes of early extubation after bypass surgery in the elderly. Ann Thorac Surg. 2004;77(3):781–788. | ||
Zhu F, Lee A, Chee YE. Fast-track cardiac care for adult cardiac surgical patients. Cochrane Database Syst Rev. 2012;10:CD003587. | ||
Walthall H, Robson D, Ray S. Do any preoperative variables affect extubation time after coronary artery bypass graft surgery? Heart Lung. 2001;30(3):216–224. | ||
Trouillet JL, Combes A, Vaissier E, et al. Prolonged mechanical ventilation after cardiac surgery: outcome and predictors. J Thorac Cardiovasc Surg. 2009;138(4):948–953. | ||
Canver CC, Chanda J. Intraoperative and postoperative risk factors for respiratory failure after coronary bypass. Ann Thorac Surg. 2003;75(3):853–857. | ||
The Society of Thoracic Surgeons. STS National Database. Available from: https://www.sts.org/national-database. Accessed July 1, 2018. | ||
Khandelwal N, Dale CR, Benkeser DC, Joffe AM, Yanez ND, Treggiari MM. Variation in tracheal reintubations among patients undergoing cardiac surgery across Washington state hospitals. J Cardiothorac Vasc Anesth. 2015;29(3):551–559. | ||
Wong WT, Lai VK, Chee YE, Lee A. Fast-track cardiac care for adult cardiac surgical patients. Cochrane Database Syst Rev. 2016;9:CD003587. | ||
Chamchad D, Horrow JC, Nachamchik L, et al. The impact of immediate extubation in the operating room after cardiac surgery on intensive care and hospital lengths of stay. J Cardiothorac Vasc Anesth. 2010;24(5):780–784. | ||
Moran JL, Peisach AR, Solomon PJ, Martin J. Cost calculation and prediction in adult intensive care: a ground-up utilization study. Anaesth Intensive Care. 2004;32(6):787–797. | ||
Wan S, Leclerc JL, Vincent JL. Inflammatory response to cardiopulmonary bypass: mechanisms involved and possible therapeutic strategies. Chest. 1997;112(3):676–692. | ||
Laffey JG, Boylan JF, Cheng DC. The systemic inflammatory response to cardiac surgery: implications for the anesthesiologist. Anesthesiology. 2002;97(1):215–252. | ||
Grawe E, Wojciechowski PJ, Hurford WE. Balancing early extubation and rates of reintubation in cardiac surgical patients: where does the fulcrum lie? J Cardiothorac Vasc Anesth. 2015;29(3):549–550. | ||
Crawford TC, Magruder JT, Grimm JC, et al. Early extubation: a proposed new metric. Semin Thorac Cardiovasc Surg. 2016;28(2):290–299. Epub 2016 Apr 26. | ||
Richey M, Mann A, He J, et al. Implementation of an early extubation protocol in cardiac surgical patients decreased ventilator time but not intensive care unit or hospital length of stay. J Cardiothorac Vasc Anesth. 2018;32(2):739–744. | ||
Murthy SC, Arroliga AC, Walts PA, et al. Ventilatory dependency after cardiovascular surgery. J Thorac Cardiovasc Surg. 2007;134(2):484–490. | ||
Reddy SL, Grayson AD, Griffiths EM, Pullan DM, Rashid A. Logistic risk model for prolonged ventilation after adult cardiac surgery. Ann Thorac Surg. 2007;84(2):528–536. | ||
Serrano N, García C, Villegas J, et al. Prolonged intubation rates after coronary artery bypass surgery and ICU risk stratification score. Chest. 2005;128(2):595–601. | ||
Knapik P, Ciesla D, Borowik D, Czempik P, Knapik T. Prolonged ventilation post cardiac surgery – tips and pitfalls of the prediction game. J Cardiothorac Surg. 2011;6(1):158. | ||
Cislaghi F, Condemi AM, Corona A. Predictors of prolonged mechanical ventilation in a cohort of 3,269 CABG patients. Minerva Anestesiol. 2007;73(12):615–621. | ||
Cislaghi F, Condemi AM, Corona A. Predictors of prolonged mechanical ventilation in a cohort of 5123 cardiac surgical patients. Eur J Anaesthesiol. 2009;26(5):396–403. | ||
Suematsu Y, Sato H, Ohtsuka T, Kotsuka Y, Araki S, Takamoto S. Predictive risk factors for delayed extubation in patients undergoing coronary artery bypass grafting. Heart Vessels. 2000;15(5):214–220. | ||
Shahbazi S, Kazerooni M. Predictive factors for delayed extubation in the intensive care unit after coronary artery bypass grafting; a southern Iranian experience. Iran J Med Sci. 2012;37(4):238–241. | ||
Stamou SC, Nussbaum M, Stiegel RM, et al. Effect of body mass index on outcomes after cardiac surgery: is there an obesity paradox? Ann Thorac Surg. 2011;91(1):42–47. | ||
Mariscalco G, Wozniak MJ, Dawson AG, et al. Body mass index and mortality among adults undergoing cardiac surgery: a nationwide study with a systematic review and meta-analysis. Circulation. 2017;135(9):850–863. | ||
Allama A, Ibrahim I, Abdallah A, et al. Effect of body mass index on early clinical outcomes after cardiac surgery. Asian Cardiovasc Thorac Ann. 2014;22(6):667–673. | ||
Papathanasiou A, Milionis H, Toumpoulis I, et al. Smoking cessation is associated with reduced long-term mortality and the need for repeat interventions after coronary artery bypass grafting. Eur J Cardiovasc Prev Rehabil. 2007;14(3):448–450. | ||
Smith PM, Burgess E. Smoking cessation initiated during hospital stay for patients with coronary artery disease: a randomized controlled trial. CMAJ. 2009;180(13):1297–1303. | ||
Ji Q, Zhao H, Mei Y, Shi Y, Ma R, Ding W. Impact of smoking on early clinical outcomes in patients undergoing coronary artery bypass grafting surgery. J Cardiothorac Surg. 2015;10(1):16. | ||
Imanipour M, Bassampoor SS, Nikbakht Nasrabadi A. Intraoperative variables associated with extubation time in patients undergoing coronary artery bypass graft surgery. Jpn J Nurs Sci. 2008;5(1):23–30. | ||
Heringlake M, Nowak Y, Schön J, et al. Postoperative intubation time is associated with acute kidney injury in cardiac surgical patients. Crit Care. 2014;18(5):547. | ||
Oliver WC, Nuttall GA, Orszulak TA, et al. Hemofiltration but not steroids results in earlier tracheal extubation following cardiopulmonary bypass: a prospective, randomized double-blind trial. Anesthesiology. 2004;101(2):327–339. | ||
Kotfis K, Szylińska A, Listewnik M, et al. Early delirium after cardiac surgery: an analysis of incidence and risk factors in elderly (≥65 years) and very elderly (≥80 years) patients. Clin Interv Aging. 2018;13:1061–1070. | ||
Jannati Y, Bagheri-Nesami M, Sohrabi M, Yazdani-Cherati J, Mazdarani S. Factors associated with post-surgical delirium in patients undergoing open heart surgery. Oman Med J. 2014;29(5):340–345. | ||
Kazmierski J, Kowman M, Banach M, et al. Incidence and predictors of delirium after cardiac surgery: results from The IPDACS Study. J Psychosom Res. 2010;69(2):179–185. | ||
Kobayashi T, Hamano K, Mikamo A, et al. Perioperative features of coronary artery bypass grafting in patients aged 75 years or older. Jpn J Thorac Cardiovasc Surg. 2002;50(4):152–157. | ||
Lee JH, Graber R, Popple CG, et al. Safety and efficacy of early extubation of elderly coronary artery bypass surgery patients. J Cardiothorac Vasc Anesth. 1998;12(4):381–384. | ||
Cheng DC. Pro: early extubation after cardiac surgery decreases intensive care unit stay and cost. J Cardiothorac Vasc Anesth. 1995;9(4):460–464. | ||
Camp SL, Stamou SC, Stiegel RM, et al. Can timing of tracheal extubation predict improved outcomes after cardiac surgery? HSR Proc Intensive Care Cardiovasc Anesth. 2009;1(2):39–47. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.