Back to Journals » Clinical Audit » Volume 15
Audit of Documentation of Chest Drain Insertion Procedures Before and After Introduction of a Chest Drain Pro forma
Authors Ahmed M, Malik S, Ng AYK , Tariq SM
Received 22 November 2022
Accepted for publication 12 April 2023
Published 21 April 2023 Volume 2023:15 Pages 1—5
DOI https://doi.org/10.2147/CA.S398594
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Zoka Milan
Mohammed Ahmed,1 Sabeen Malik,2 Anthony Yong Kheng Ng,3 Syed Mohammad Tariq2
1Department of Respiratory Medicine, Southampton General Hospital, Southampton, Hampshire, UK; 2Department of Respiratory Medicine, Luton and Dunstable University Hospital, Luton, Bedfordshire, UK; 3Department of Respiratory Medicine, Addenbrooke’s University Hospital, Cambridge, Cambridgeshire, UK
Correspondence: Syed Mohammad Tariq, Luton & Dunstable University Hospital, Lewsey Road, Luton, Bedfordshire, LU4 0DZ, United Kingdom, Tel +44 7886025415, Fax +44 1582497237, Email [email protected]
Aim: Chest drains are indicated for pleural effusions and pneumothoraces. Documentation of chest drain insertion in patients’ notes can vary and may be sub-standard. We did a retrospective audit of documentation of chest drain insertions and repeated it after the introduction of a chest drain pro forma.
Patients and Methods: All chest drain insertions over a two-year period (2017– 2019) in our hospital were audited. Indwelling pleural catheter insertions were excluded. We re-audited chest drains inserted in the respiratory ward for 3 months (January–March 2020) after the introduction of a chest drain pro forma to assess improvements in documentation.
Results: In the first audit, 134 patients had chest drains [85(63%) male; age 18– 91 years]; 16 of these were emergency procedures. Documentation of chest drain insertion procedures was poor. In 12(9%), the procedure was not recorded at all. One or more pre-procedural safety checks (indication, review of radiology, coagulation parameters) were documented in 23(17.2%) procedures. In 11(8.2%) the department/unit where the procedure was performed was not documented. In 30(22.4%) the time of the procedure was not entered. The grade and speciality of doctor performing the procedure was missing in 18(13.4%) and 13(9.7%) entries, respectively. Patient consent was available for 90(67.2%) procedures (61 verbal, 29 written). Adherence to aseptic technique was mentioned in 66(49.2%), and the dose of local anaesthetic was included in 82(46.3%) entries. Re-audit following the introduction of a pro forma in respiratory ward (n=29) showed improvements in documentation. There was a significant improvement in the documentation of pre-procedural checks (59.8% vs 19.4%), and a positive trend in documentation of consent and the use of local anaesthetic.
Conclusion: Documentation of chest drain insertion procedures can vary and may be incomplete. Routine use of a pro forma improves documentation of chest drain insertion procedures and should enhance overall patient safety.
Keywords: documentation, chest drain, consent, patient safety, pre-procedural checks, procedure
Introduction
Chest drains are an important but invasive intervention, which can lead to potentially serious complications. Hence, chest drain insertion and its aftercare require appropriate training and experience to improve overall safety and efficacy of the procedure. A UK-wide audit highlighted non-negligible rates of complications from chest drains, and made several recommendations to improve safety.1 These recommendations include important pre-procedural safety checks, avoidance of chest drain insertion out-of-hours, and optimal documentation. The recommendations were further elaborated recently.2 These guidelines provide the basis for adequate documentation of chest drain insertion procedures, with emphasis on pre-procedural safety checks (review of chest radiology and coagulation profile), routine use of chest ultrasound for pleural fluid, written informed consent, use of aseptic technique, and details of drugs (analgesia, local anaesthetic) given.
In a recent study, improvements in clinical documentation were achieved for endoscopic procedures using an endoscopy checklist.3 Apart from improving patient safety, well-designed, person-centered endoscopy checklists also assist in auditing clinical performance and in more accurate coding and billing for the services provided.4
Luton and Dunstable University Hospital is a 650-bed facility providing secondary-level healthcare to a population of over 400,000. The acute services include all major medical and surgical specialties. On average, there are around 50 unselected acute medical admissions daily to adult medical wards, and further 20 acute admissions to the care of elderly wards. Chest drain insertion procedures are usually performed in the Accident & Emergency Unit, the Emergency Admissions Unit, and the Respiratory Medical Ward. Patients are routinely transferred to the Respiratory Medical Ward after drain insertion for on-going care, subject to bed availability. Both Seldinger (wire-guided) and surgical chest drains are available for use. However, aside from senior respiratory specialists, competency on insertion of surgical drains is limited as majority of chest drain placements involve Seldinger kits.
We ran a baseline audit of the documentation of chest drain insertion procedures in our hospital over a two-year period and then re-audited the documentation after the introduction of a chest drain pro forma in our respiratory medical ward, to assess whether the use of the pro forma improves documentation. Prior to the introduction of this pro forma, chest drain insertion procedures were documented by the operator as hand-written entries into the patients’ paper notes, and there was no formal training on optimal documentation.
In 2016, Hasan and Barnes reported significant variability in documentation of pleural procedures.5 They audited documentation of six general parameters [consent, operator details, indication, type of procedure, complications, and risk assessment—International Normalized Ratio (INR) and platelets], and six pleural-specific parameters (site of abnormality, ultrasound findings, medications administered, aspirate amount and character, tests requested, and post-procedure management). It was a small audit with data from 30 procedures at baseline and 30 procedures after introduction of a new pro forma. There was poor documentation in the baseline audit with none of the 30 procedures showing complete documentation of all 12 pre-determined parameters, whereas 66% of the procedures achieved full documentation after the introduction of the pro forma.5 It also had a positive impact on the quality of electronic patient discharge summaries. Unlike our audit focusing on chest drain insertion procedures, this audit included a range of pleural interventions – thoracic ultrasound, pleural aspiration, chest drain insertion, talc pleurodesis, and indwelling pleural catheter insertion.5
Materials and Methods
Following approval by the hospital’s Clinical Quality Department, a data collection form was developed (Appendix 1), based on the British Thoracic Society guidelines on chest drains.2 Patient Records Unit provided a list of all patients given a chest drain between 01 May 2017 and 01 May 2019. Indwelling pleural catheter insertion procedures were excluded as they are performed by three well-trained senior respiratory physicians in the endoscopy unit on a “day-case” basis. Data was transferred to an electronic (Microsoft ExcelTM) file. Some demographic details were omitted to anonymize patients, and hospital numbers were used as the sole identifier. Results of this audit led to the development of a chest drain pro forma which was formally approved as a “Chest Drain Checklist” (Appendix 2) and introduced for use in the respiratory medical ward from 01 January 2020. After the delivery of a one-off training session to the nurses, and junior and middle-grade doctors, the ward-based team was asked to routinely use this pro forma for all chest drain insertions and file it in patients’ notes. We re-audited the documentation of chest drain procedures for 3 months (01 January-31 March 2020) after the introduction of the pro forma. The re-audit was curtailed as the use of the pro forma was suspended from 01 April 2020 following the start of the first wave of COVID-19 pandemic in the UK. Results of the re-audit were compared with the first audit using chi-square analysis to assess the impact of the pro forma on documentation of chest drain insertion procedures. A p value of <0.05 was taken as statistically significant.
Ethical approval for this project was not required as it did not involve any additional intervention, with all patients receiving usual care.
Results
In the first audit period, after excluding indwelling pleural catheters (n=9), 134 chest drains were inserted in our hospital during the 2 years from 01 May 2017. In the re-audit over 3 months after the introduction of chest drain pro forma, 29 patients in the respiratory ward had a chest drain. Table 1 gives patient details and indications for a chest drain. For the second audit, we collected data only from patients who were given a chest drain in the respiratory ward, and no data was taken from any chest drains inserted elsewhere in the hospital. In the first audit 12(9%) cases had no documentation of the procedure in the notes; these cases were included in the analysis. The mean age was similar, but there were significantly more male patients in the first audit. Common indications were pneumothorax, pleural effusion, medical talc pleurodesis, and empyema. Relatively more patients with a pleural effusion had chest drains in the second audit, whereas medical pleurodesis was given more often in the first audit (Table 1). There were no cases of traumatic haemo-pneumothorax in the re-audit. In the initial audit 43(32.1%) drains were inserted in non-respiratory wards, 37(27.6%) in the emergency department, 33(24.6%) in the respiratory ward, and 11(8.2%) in the radiology department under ultrasound guidance, whilst in 21 patients (15.6%) the department where the procedure was performed was not documented. In the second audit 7(24.1%) patients had their drains inserted in a non-respiratory department (6 in the Emergency Department, and 1 in the Radiology Department). Only one patient in the re-audit had a chest drain inserted out-of-hours, compared with 37(27.6%) drains inserted out-of-hours (outside 08:00 to 18:00 hours, or over weekends) in the first audit (p<0.01). In 74(55.2%) cases in the first audit the time of procedure was not documented, compared with 3(10.3%) cases in the second audit (p<0.01). Chest drain procedures were performed more often by respiratory doctors in the second audit, but the difference was not statistically significant (Table 2). In the first audit, the specialty of the doctor was missing in 12(9%) entries. The grade of the doctor performing the procedure was available in 104 (85.2%) cases (middle grade and specialty trainee 64; junior trainee 29; consultant 22).
 |
Table 1 Patients, and Indications for a Chest Drain |
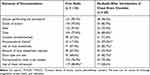 |
Table 2 Comparison of the First and Second Audit |
In the baseline audit, written or verbal consent was not documented in 44 (26.2%) entries. Verbal consent was taken from 61, and written consent from 29 patients. Post-procedure instructions including controlled drainage, a repeat chest x-ray, and analgesia were written in 91 (74.6%) cases. These instructions, however, were considered incomplete in 5 of these 91 entries, with one or more key elements missing. There were marginal improvements in the documentation of consent, use of local anaesthetic and post-procedure chest x-ray requests after the introduction of the pro forma (Table 2). A higher proportion of chest drains was inserted under ultrasound guidance in the first audit [119 of 134(88.8%) v 17 of 29(58.6%), p < 0.01] (Table 2).
Discussion
There was no documentation at all on 12(9%) chest drain insertion procedures in the first audit, whereas all 29 chest drain insertions were accounted for through the 3 months of re-audit in the respiratory ward after the roll-out of the chest drain pro forma. It was also reassuring that the use of the chest drain pro forma improved the documentation of important pre-procedural checks (indication for chest drain insertion, review of chest radiology, and coagulation screen check). Aside from performing and documenting pre-procedural checks, the use of chest ultrasound for pleural fluid, good drain insertion technique, secure anchoring and dressing of the chest drain, and on-going optimal care till the time it is removed, are all crucial for patient safety.1,2
The differences between the two audits in indications for a chest drain, and the time the drain was inserted, can be explained by the fact that the first audit included patients across the whole hospital over a period of 2 years, whereas the second audit covered a period of 3 months only and was limited to the respiratory ward. Traumatic haemo-pneumothorax patients are managed in surgical wards in our hospital. Many patients with empyema also go to surgical wards or to the High Dependency or Intensive Care Unit if they are critically ill.
More frequent use of ultrasound guidance for chest drain insertion in the first audit compared with the re-audit can be attributed to more chest drains inserted in the radiology department (11 vs 1) in the first audit, and a slightly higher proportion of pneumothorax patients given a chest drain in the second audit, as chest ultrasound is not indicated for pneumothoraces (Table 1).
In general, the use of checklists and pro forma in medical and surgical procedures improve documentation and overall safety.4–6 Checklists also help in auditing performance, and analyzing rare untoward/critical events and learning from them.
There is an old adage in health care that “not documented means not done.”7 Nonetheless, in the first audit, there were 12(9%) patients with no documentation of the chest drain insertion procedure at all, but these procedures were performed as per the subsequent entries in the case notes and in electronic patient discharge letters. In the re-audit, after the introduction of the chest drain pro forma, every chest drain insertion was accounted for. However, the level of documentation was variable. Further improvements in documentation of these procedures may be achieved by including a training session on documentation of chest drains as part of training on common procedural skills, which is a mandatory simulation training module for internal medicine trainees. This module is run three times a year in our hospital, and covers several bedside procedures including lumbar puncture, central venous line insertion, nasogastric tube insertion, chest drains, paracentesis, and urinary catheters. Electronic data entry of chest drains, with certain key fields programmed as mandatory, such as indication, review of radiology and coagulation status, consent, and the dose of local anaesthetic given, may also improve documentation and overall safety of these procedures. Nonetheless, despite increasing in popularity, several issues were recently raised regarding the quality, standardization, and user-friendliness of electronic documentation of health records within inpatient setting.8 Hence, any electronic documentation software for chest drain insertion procedures would require due care in designing it to ensure that it is easy to use and fit for purpose.
In 2016, poor documentation of parameters related to pleural procedures was reported in a published abstract, especially the recording of consent, complications, and post-procedure management,5 but the authors did not provide figures for individual parameters. In our baseline audit, consent was recorded in 90 (67.2%) patients given a chest drain (Table 2). However, written consent, as recommended by the BTS,1,2 was recorded in only 29 (21.6%) patients. We looked at the documentation of immediate complications only in our audits. There was immediate severe pain recorded in one patient in the first audit, which was later attributed to iatrogenic injury to the rib superior to the drain insertion site. One or more post-procedure management instructions were available in 91(74.6%) patients (Table 2), but in five of these entries, the instructions were deemed incomplete.
In our hospital, most chest drains are inserted in the Accident & Emergency Department (A&E), the Emergency Admissions Unit (EAU), and the respiratory ward. Hence, we are currently trying to extend the use of the chest drain pro forma to A&E and the EAU.
In conclusion, our baseline audit of documentation of chest-drain insertion procedures highlighted major shortcomings. There were significant improvements in documentation of these procedures in the re-audit after the introduction of a chest drain pro forma in the respiratory ward, especially in parameters crucial for patient safety (indication, and review of radiology and coagulation screen). Further improvements in documentation of chest drains may be achieved by better training of junior doctors, and possibly, by using an electronic version of the pro forma.
Acknowledgments
We are grateful to the hospital’s Clinical Quality Department for their support in setting up and conducting these audits.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Hooper C, Maskell N. BTS audit team. British Thoracic Society National Audit: pleural procedures audit 2010. Thorax. 2011;66(7):636–637. doi:10.1136/thoraxjnl-2011-200077
2. British Thoracic Society. British Thoracic Society Clinical Statement on Pleural Procedures; 2018. Available from: https://www.brit-thoracic.org.uk/media/455880/bts-clinical-statement-on-pleural-procedures-consultation-jun-2022.pdf.
3. Kelly V, Baar-Daley KM. Improving clinical documentation compliance pre-gastrointestinal endoscopy procedures through the use of an endoscopy checklist. Gastroenterol Nurs. 2022;45(5):328–334. doi:10.1097/SGA.0000000000000656
4. Dubois H, Schmidt P, Creutzfeldt J, Bergenmar M. Person-centred endoscopy safety checklist: development, implementation, and evaluation. World J Gastroenterol. 2017;23(48):8605–8614. doi:10.3748/wjg.v23.i48.8605
5. Hasan N, Barnes S. Improving the documentation of pleural procedures: the impact of a new standardized pleural procedure pro forma. Clin Med. 2016;16(Suppl 3):S14. doi:10.7861/clinmedicine.16-3-s14
6. Boyd JM, Wu G, Stelfox HT. The impact of checklists on inpatient safety outcomes: a systematic review of randomized controlled trials. J Hosp Med. 2017;12:675–682. doi:10.12788/jhm.2788
7. Mandell N. Not documented – not done. Nursing. 1994;24(8):62–63. doi:10.1097/00152193-199408000-00029
8. Varela LO, Wiebe N, Niven DJ, et al. Evaluation of interventions to improve electronic health record documentation within inpatient setting: a protocol for a systematic review. Syst Rev. 2019;8(1):54. doi:10.1186/s13643-019-091702
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
