Back to Journals » Neuropsychiatric Disease and Treatment » Volume 15
Associations Of Personality Traits With The Capacity-Performance Discrepancy Of Functional Outcome In Patients With Schizophrenia
Authors Uchino T, Nemoto T , Yamaguchi T, Katagiri N, Tsujino N, Murakami Y, Tanaka K, Mizuno M
Received 7 June 2019
Accepted for publication 13 September 2019
Published 3 October 2019 Volume 2019:15 Pages 2869—2877
DOI https://doi.org/10.2147/NDT.S218738
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Taro Kishi
Takashi Uchino,1,2 Takahiro Nemoto,1 Taiju Yamaguchi,1 Naoyuki Katagiri,1 Naohisa Tsujino,1 Yoshitaka Murakami,3 Kuniaki Tanaka,2 Masafumi Mizuno1
1Department of Neuropsychiatry, Toho University Graduate School of Medicine, Tokyo 143-8540, Japan; 2Tokyo Adachi Hospital, Tokyo 121-0064, Japan; 3Department of Medical Statistics, Toho University School of Medicine, Tokyo 143-8540, Japan
Correspondence: Takahiro Nemoto
Department of Neuropsychiatry, Toho University Graduate School of Medicine, 5-21-16 Omori-Nishi, Ota-ku, Tokyo 143-8540, Japan
Tel +81 3 37624151
Fax +81 3 54715774
Email [email protected]
Objective: Functional capacity, which indicates one’s ability to perform everyday living tasks, contributes to real-world functional performance in patients with schizophrenia. However, functional capacity is sometimes not comparable with functional performance in clinical settings. We hypothesized that specific personality traits are related to this capacity-performance discrepancy of functional outcome.
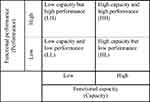
Methods: The measures in this study were the UCSD Performance-based Skills Assessment Brief (UPSA-B) for functional capacity, the Social Functioning Scale (SFS) for functional performance, and the Temperament and Character Inventory-140 (TCI-140) for personality traits. A total of 94 stable outpatients with schizophrenia were divided into four groups based on combinations of their UPSA-B and SFS cut-off points, as follows: a high capacity and high performance (HH) group, a high capacity but low performance (HL) group, a low capacity but high performance (LH) group, and a low capacity and low performance (LL) group.
Results: There were no significant differences in demographics among the four groups. The LH group showed a significantly lower harm avoidance level than the LL group. The HL group showed a significantly lower persistence level than the HH group.
Conclusion: Lower harm avoidance may enhance functional performance, and lower persistence can limit functional performance, regardless of the primary levels of functional capacity in patients with schizophrenia. Novel and individualized psychosocial treatments considering the individual’s personality traits seem to be helpful for maximizing their functional performance in the community.
Keywords: functional capacity, performance-based assessment, real-world functioning, social functioning, Temperament and Character Inventory
Introduction
Clinical recovery among patients with schizophrenia requires not only the long-term reduction or, ideally, the removal of psychopathological symptoms, but also an improvement in real-world functional performance in daily living.1,2 Functional performance is defined as functioning to fulfill one’s role in the interactions of an individual with one’s environment.3 This environment includes varied situations such as work, school, family life, friends, and independent living. Among patients with schizophrenia, the decline in functional performance is severe, and the proportion of patients who achieve a clinical recovery is quite low.4 In fact, many patients with schizophrenia struggle to work and live by themselves, leading to an extremely high level of disability among those suffering from schizophrenia even when compared with the level of disability experienced by individuals suffering from physical diseases.5,6 Therefore, investigating the functional performance of patients with schizophrenia so as to achieve their clinical recovery is an urgent problem. Potential predictors of functional performance have been investigated, and the control of psychotic symptoms alone has been reportedly insufficient for its improvement. Cognitive function can predict subsequent functional performance with an effect size that is greater than the medium range.7–9 However, the effects of enhancements in cognitive function on functional performance in community can be substantially diminished by several intervening variables, including personal and social factors.10,11 Considering this fact, functional capacity has been attracting attention as a co-primary measure that may act as a mediator between cognitive function and functional performance.12
Functional capacity refers to an individual’s capacity to perform key tasks of daily living. To assess functional capacity, participants simulate real-world activities, such as holding social conversations, preparing meals, or taking public transportation, through the use of props and role-playing in the clinic or laboratory.13 A good functional capacity does not mean that a person does perform daily living tasks well in the community, but it means that the person was able to perform the tasks when given the opportunity.12 Numerous studies have shown that a reduced functional capacity relates to insufficient functional performance.14–16 A recent study using network analysis has also confirmed that functional capacity provides a connection between cognitive function and functional performance, and the study’s findings support the fact that improving functional capacity is critical for therapeutic interventions in patients with schizophrenia.17
However, functional capacity is not occasionally compatible with functional performance, especially in clinical settings. As mentioned above, functional capacity indicates one’s “capacity” (what one can do), not one’s “performance” (what one actually does). Only a few studies have focused on “capacity-performance discrepancy,” and investigated factors related to a lower functional performance than expected by a high functional capacity (ie, a high capacity but a low performance). Gupta et al18 reported that more time spent in a hospital, restricted living situations such as a group home, and severe depressive symptoms were predictors of the capacity-performance discrepancy. Other studies19,20 focusing on intrapersonal factors suggested that self-efficacy or meta-cognition could mediate the size of the discrepancy between capacity and performance. These factors can be considered as “limiters,” since they inhibit the translation of a high functional capacity into appropriate functional performance. These “limiters” can generate a high capacity–low performance discrepancy. On the other hand, clinical experience suggests the existence of “enhancers,” which can improve or maintain high functional performance beyond a low functional capacity. These “enhancers” can generate a low capacity–high performance discrepancy. In clinical settings, some patients with schizophrenia exhibit a higher functional performance than predicted by their low functional capacity. They adapt to their community life smoothly beyond their capacity, and clinicians often wonder at their ability to do so. In our previous study,21 we revealed and supported this fact. Namely, a certain proportion of patients with schizophrenia in the community showed a low capacity–high performance discrepancy. Furthermore, we suggested that reduced tendency of social anxiety could enhance their performance despite low capacity. In social anxiety disorder, symptoms have been proposed to be related to personality traits.22,23 Some temperament factors could also contribute to social anxiety.24 In patients with schizophrenia, high prevalence of social anxiety and associations of social anxiety with personality traits have been reported.25,26
Personality traits affect human behavior and determine adjustments to environment in real-world settings.27 The personality traits of patients with schizophrenia have been remarked upon, and abnormalities in these traits, compared with those of healthy controls, have been identified in meta-analyses.28,29 The psychobiological model, which is a major theory of personality traits proposed by Cloninger et al,30 has been widely used in studies on schizophrenia. Recently, personality traits have come to be considered as one of the most important factors in the pathogenesis of schizophrenia because they influence both cognitive function and psychopathology.31–34 Furthermore, evidence that specific personality traits are correlated with a variety of social and clinical variables, such as coping style, vocational functioning, quality of life, and interpersonal relations, has been accumulated.35–38 However, the role of personality traits toward functional performance in community is still obscure.
We hypothesized that specific personality traits can be “limiters” or “enhancers” that influence the capacity–performance discrepancy (ie, generate a high capacity–low performance discrepancy or a low capacity–high performance discrepancy). This hypothesis was based on the previous studies and clinical experiences that the intrapersonal factors could generate the capacity-performance discrepancy regardless of the environmental factors and that each individual with different personality traits perform differently in real-world even when they are in the same environment.19,20,27 In the current study, we examined the characteristics of a group of patients with schizophrenia who exhibit low functional performance despite a high functional capacity and a group of patients with schizophrenia who exhibit high functional performance despite a low functional capacity. Based on our previous findings,21 we recruited different participants who had longer duration of illness than the previous study, because decline of functional performance in patients with chronic schizophrenia is an urgent problem in clinical settings.6,39 Furthermore, the present study adopted a performance-based measure to accurately assess functional capacity,15 although we had used a self-report measure by patients in our previous study.21 Most importantly, we investigated the associations of personality traits with the capacity–performance discrepancy of functional outcome in patients with schizophrenia which have not been examined yet.
Methods
Participants
Ninety-four stable outpatients with schizophrenia were recruited at the Toho University Omori Medical Center and Tokyo Adachi Hospital, Tokyo, Japan. Each diagnosis was confirmed according to the Diagnostic and Statistical Manual of Mental Disorders 5th Edition (DSM-5) by more than two well-experienced psychiatrists. The participants were receiving outpatient treatment continuously and did not have a history of psychiatric hospitalization within three months of their assessments. The inclusion criteria were patients who were living in the community and were between 16 and 60 years of age. To lessen the effects of environmental factors on functional performance18 and to focus on individual-related factors, patients who were in supervised living situations, such as board and care facilities, were excluded. Other exclusion criteria were patients with alcohol or substance abuse and those with mental retardation or severe physical illnesses.
All the participants provided written informed consent prior to their inclusion in the study. If the participant was under 20 years old, written informed consent was also obtained from the participant’s parent. The Institutional Review Board of the Toho University School of Medicine approved the protocol for the study (A17007). This study was performed in accordance with the latest version of the Declaration of Helsinki.
Measures
Functional performance was evaluated using the Social Functioning Scale (SFS),40,41 which is a comprehensive assessment of seven areas of functioning that are crucial for people with schizophrenia to be able to live in the community. The SFS can be used as a self-reported or informant interview. In the current study, we used it as a self-reported questionnaire and assessed the total score on the SFS. Functional capacity was evaluated using the UCSD Performance-based Skills Assessment Brief (UPSA-B)42,43 which involves role-playing tasks related to two subscales: finance and communication. Psychopathology was evaluated using the Positive and Negative Syndrome Scale (PANSS)44,45 and neurocognition was evaluated using the Brief Assessment of Cognition in Schizophrenia (BACS).46,47
Personality traits were evaluated using the Temperament and Character Inventory 140 (TCI-140)30,48,49 which is a 140-question self-reported instrument. The TCI-140 assesses personality traits in seven dimensions, four for temperament and three for character. The temperament dimensions are 1) novelty seeking, 2) harm avoidance, 3) reward dependence, and 4) persistence. The character dimensions are 5) self-directedness, 6) cooperativeness, and 7) self-transcendence.
Capacity-Performance Discrepancy Of Functional Outcome
Because standard cut-off points in the SFS and UPSA-B have not been established,50 we adopted the median scores of the total participants as cut-off points to determine if the participants ranked high or low in capacity/performance, respectively. Using these parameters, we divided the participants into four groups: a high capacity and high performance (HH) group, a high capacity but low performance (HL) group, a low capacity but high performance (LH) group, and a low capacity and low performance (LL) group (Figure 1).
Statistics
We performed a one-way analysis of variance (ANOVA) and chi-squared test to compare differences in demographics and clinical variables among the four groups. If these tests revealed significant differences among these groups, we performed a post hoc analysis using the Bonferroni correction. To investigate the characteristics of participants with capacity-performance discrepancy, we focused on the differences between the HH and HL groups (ie, the high capacity–low performance discrepancy) and those between the LH and LL groups (ie, the low capacity–high performance discrepancy). Statistical differences were determined using two-tailed tests and a significance level of p <0.05.
Results
Demographics And Capacity-Performance Discrepancy Of Participants
Of the 94 patients who were recruited, 53 were male (56.4%) and 41 were female (43.6%). The mean age of the participants was 41.1 (SD=10.2) years, and the mean age of onset was 26.0 (SD=7.8) years. The mean duration of illness was 15.1 (SD=10.4) years. The mean length of education was 13.5 (SD=2.1) years. The average number of hospitalizations was 1.6 (SD=1.8) times. The mean dose of antipsychotics was 475.3 (SD=387.7) mg/day, chlorpromazine equivalent. The median scores of UPSA-B and SFS were 73 and 113, respectively.
Of the 94 participants in total, 26 participants landed above or equal to the median scores of the UPSA-B and SFS (ie, high capacity and high performance: HH group), 27 participants landed above or equal to the median score of the UPSA-B and below the median score of the SFS (ie, high capacity but low performance: HL group), 22 participants landed below the median score of the UPSA-B and above or equal to the median score of the SFS (ie, low capacity but high performance: LH group), and 19 participants landed below the median scores of the UPSA-B and SFS (ie, low capacity and low performance: LL group). Comparisons among the 4 groups are presented in Table 1. There were no significant differences in demographics among the 4 groups.
 |
Table 1 Differences In Background And Clinical Variables Among The Four Groups |
Differences In Personality Traits
Several significant differences in personality traits were observed. The LH group had a significantly lower Harm Avoidance (HA) score than the LL group (mean HA scores: 60.0 vs 65.0), but no significant difference was seen between the HH and HL groups. The HL group had a significantly lower Persistence (PS) score than the HH group (mean PS scores: 52.9 vs 61.4), but no significant difference was seen between the LH and LL groups.
Differences In Other Clinical Variables
Regarding other clinical variables, the HH and LH groups had lower PANSS negative and general psychopathology scores than the HL and LL groups, respectively (mean PANSS negative scores between the HH and HL groups: 18.9 vs 21.4, those between the LH and LL groups: 19.4 vs 24.5; mean PANSS general psychopathology scores between the HH and HL groups: 40.2 vs 45.7, those between the LH and LL groups: 42.8 vs 47.7). The LH group had a lower PANSS positive score than the LL group (mean PANSS positive scores between the LH and LL groups: 17.4 vs 20.7). Significant differences in BACS were observed among the four groups. In a post hoc analysis, no differences were observed between the HH and HL groups or between the LH and LL groups, but significant differences were observed between the HL and LL groups or between the HH and LH groups (mean BACS score between HL and LL groups: −3.3 vs −5.7, those between the HH and LH groups: −2.3 vs −4.1).
Discussion
Capacity–Performance Discrepancy Of Functional Outcome In Real-World Settings
The current results revealed the presence of different characteristics in patients with high functional performance despite a low functional capacity and also in patients with low functional performance despite a high functional capacity. These findings support our previous study21 and the fact that clinicians sometimes encounter patients whose actual performance is not compatible with their capacity in a clinical setting and that the long-term clinical course for patients with schizophrenia can vary widely. Furthermore, the current results suggested several potential “limiters” and “enhancers” that might be related to these discrepancies. To the best of our knowledge, the associations of the capacity-performance discrepancy with personality traits as potential “limiters” or “enhancers” of functional performance that act regardless of the primary levels of functional capacity have not been previously studied.
Personality Traits Related To Capacity–Performance Discrepancy
Regarding the seven dimensions of personality traits, the LH group had a lower HA score than the LL group, but no difference was seen between the HH and HL groups. HA is viewed as an inheritable bias in the inhibition or cessation of behavior, such as pessimistic worrying in anticipation of future problems, passive avoidant behavior such as fear of uncertainty and shyness of strangers, and rapid fatigability.30 Given previous work in healthy subjects,51 avoidant behavior can be associated with stress vulnerability, adjustment, and personal functioning. Jetha et al35 reported that shyness, which is a conceptually linked dimensional sub-scale of the HA, is predictive of social functioning in patients with schizophrenia. They also reported that shyness is independent from the psychopathology of schizophrenia. The present result suggests that a more unworried and extroverted temperament, as reflected by a lower HA score, may facilitate the behavior and role of patients in the community beyond their low capacity. Namely, it may contribute to an improvement or the maintenance of functional performance even though the patients have an insufficient functional capacity, which usually is a strong predictor for low functional performance. In our previous study, a tendency of low social anxiety was associated with high performance despite low capacity in social functioning in schizophrenia.21 In light of the current results, a lower HA score could be considered as an “enhancer” capable of generating a low capacity–high performance discrepancy.
The HL group had a lower PS level than the HH group, but no difference was seen between the LL and LH groups. PS reflects an inheritable bias in the maintenance of behavior despite frustration, fatigue, and intermittent reinforcement.30 People with a low PS seem to be hesitant, easy discouraged, lazy, and underachieving. According to a previous long-term birth cohort study in people with psychosis,52 PS could predict both social and occupational outcomes. Furthermore, a high PS personality style, which is characterized by ambition, resistance to frustration, and a performance-orientated nature, was important for good overall functioning. In light of the current results, the temperament of individuals with lower PS scores, who tend to give up easily, may interfere with successful behavior in the community, even though such individuals may have a high capacity for performance. Namely, a low PS may inhibit the translation of a high functional capacity into appropriate functional performance. Therefore, a lower PS score could be considered as a “limiter” capable of generating a high capacity–low performance discrepancy.
Other Clinical Variables In The Current Study
With regard to cognitive function, no differences were observed between the HH and HL groups or between the LH and LL groups, but significant differences were observed between the HL and LL groups or between the HH and LH groups. These data indicated that the level of cognitive function could be related more strongly with functional capacity than functional performance. This fact supports previous studies which show that functional capacity could be a mediator between cognitive function and functional performance.12 The current results also revealed that the HH and LH groups had a milder psychopathology than the HL and LL groups. A previous study53 suggested that a milder psychopathology may be related to a higher functional performance. In particular, negative symptoms have been reported to be strong predictors of functional performance.54,55 In our previous study, negative symptoms were a characteristic of patients with low performance despite high capacity.21 The presently reported results were roughly consistent with those of previous studies.
Limitations
The current study had several limitations. The SFS was assessed as a self-reported measure by the patients in the current study. Although the reliability of self-reported measures for patients with schizophrenia is generally a concern, a previous study revealed that the agreement between SFS scores scored by patients and informants was “almost perfect” (the intraclass correlation coefficient was 0.87).41 Furthermore, the VALERO Study,56 which aimed to select the optimal measures of functional performance, also suggested that the SFS is one of the most effective measures of functional performance. Another limitation of the current study is the fact that this was a cross-sectional study. However, personality traits are relatively stable throughout the course of schizophrenia even from the putative prodromal stage, such as the at-risk mental state for psychosis (ARMS),57,58,59 and people with a high genetic risk of schizophrenia are also found to possess abnormal personality traits similar to those of patients with schizophrenia.60,61 Recently, personality traits, especially HA, have been suggested to be potential endophenotypes of schizophrenia.57,60,62 Furthermore, the evidence for personality measures as endophenotypes is at least equivalent to that for cognitive measures.63 Although we cannot explain the causality and intervening effects between personality traits and functional performance, in line with the theory of personality traits as endophenotypes, personality traits may be predictive of functional performance as a phenotype. Confounding factors are also one of the limitations. Many contributors to functional capacity and performance, such as demographics, psychopathology, cognitive function, and personality traits, have been investigated and could be confounding each other.16,17,26,35,37 Although we could not reveal the confounding, this study showed the potential effect of personality traits on functional discrepancy. In this study, we divided the participants into 4 groups by the median scores of UPSA and SFS considering the statistical power because we focused on both the HL group and the LH group, although it could be a drawback from the viewpoint of statistical analyses.
Future Perspectives And Conclusion
This study suggested the roles of personality traits as potential “limiters” and “enhancers” in relation to the capacity-performance discrepancy. In the future, we need to conduct longitudinal studies that will also include the putative prodromal stage such as an ARMS and that will consider the causality and confounding. In the current study, we concluded that a lower HA could be viewed as an “enhancer” capable of improving functional performance despite a low functional capacity, while a lower PS appeared to act as a “limiter” reducing functional performance despite a high functional capacity. Conventional psychosocial rehabilitations and cognitive training have targeted improvements in functional performance, but their effects are sometimes limited.64 Therefore, we should investigate the mechanisms of functional performance and functional capacity in the community. Novel and individualized psychosocial treatments considering the concepts of “enhancers” and “limiters”, such as personality traits, might be helpful for maximizing their functional performance, which has thus far been recognized as a difficult task. We believe that the current findings will meaningfully contribute to the development of clinical recovery methods for patients with schizophrenia.
Acknowledgment
This work was partly funded by Public Grant from Japan Society for the Promotion of Science (JSPS) KAKENHI Grant Number JP25461787 to T.N.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Liberman RP, Kopelowicz A. Recovery from schizophrenia: a concept in search of research. Psychiatr Serv. 2005;56(6):735–742. doi:10.1176/appi.ps.56.6.735
2. Slade M, Amering M, Oades L. Recovery: an international perspective. Epidemiol Psichiatr Soc. 2008;17(2):128–137. Available from: http://www.ncbi.nlm.nih.gov/pubmed/18589629.
3. Weissman MM, The assessment of social adjustment. A review of techniques. Arch Gen Psychiatry. 1975;32(3):357–365. doi:10.1001/archpsyc.1975.01760210091006
4. Jääskeläinen E, Juola P, Hirvonen N, et al. A systematic review and meta-analysis of recovery in schizophrenia. Schizophr Bull. 2013;39(6):1296–1306. doi:10.1093/schbul/sbs130
5. World Health Organization. World Report on Disability 2011. World Health Organisation and the World Bank; 2011:
6. Whiteford HA, Degenhardt L, Rehm J, et al. Global burden of disease attributable to mental and substance use disorders: findings from the Global Burden of Disease Study 2010. Lancet. 2013;382(9904):1575–1586. doi:10.1016/S0140-6736(13)61611-6
7. Green MF, Kern RS, Braff DL, Mintz J, Neurocognitive deficits and functional outcome in schizophrenia: are we measuring the “right stuff”? Schizophr Bull. 2000;26(1):119–136. doi:10.1093/oxfordjournals.schbul.a033430
8. Green MF, Kern RS, Heaton RK. Longitudinal studies of cognition and functional outcome in schizophrenia: implications for MATRICS. Schizophr Res. 2004;72(1):41–51. doi:10.1016/j.schres.2004.09.009
9. Tominaga T, Tomotake M, Takeda T, et al. Relationship between social and cognitive functions in people with schizophrenia. Neuropsychiatr Dis Treat. 2018;14:2215–2224. doi:10.2147/NDT.S171207
10. Brekke J, Kay DD, Lee KS, Green MF. Biosocial pathways to functional outcome in schizophrenia. Schizophr Res. 2005;80(2–3):213–225. doi:10.1016/j.schres.2005.07.008
11. Bowie CR, Reichenberg A, Patterson TL, Heaton RK, Harvey PD. Determinants of real-world functional performance in schizophrenia subjects: correlations with cognition, functional capacity, and symptoms. Am J Psychiatry. 2006;163(3):418–425. doi:10.1176/appi.ajp.163.3.418
12. Green MF, Nuechterlein KH, Kern RS, et al. Functional co-primary measures for clinical trials in schizophrenia: results from the MATRICS Psychometric and Standardization Study. Am J Psychiatry. 2008;165(2):221–228. doi:10.1176/appi.ajp.2007.07010089
13. McKibbin CL, Brekke JS, Sires D, Jeste DV, Patterson TL. Direct assessment of functional abilities: relevance to persons with schizophrenia. Schizophr Res. 2004;72(1):53–67. doi:10.1016/j.schres.2004.09.011
14. Bowie CR, Leung WW, Reichenberg A, et al. Predicting schizophrenia patients’ real-world behavior with specific neuropsychological and functional capacity measures. Biol Psychiatry. 2008;63(5):505–511. doi:10.1016/j.biopsych.2007.05.022
15. Mausbach BT, Bowie CR, Harvey PD, et al. Usefulness of the UCSD performance-based skills assessment (UPSA) for predicting residential independence in patients with chronic schizophrenia. J Psychiatr Res. 2008;42(4):320–327. doi:10.1016/j.jpsychires.2006.12.008
16. Strassnig MT, Raykov T, O’Gorman C, et al. Determinants of different aspects of everyday outcome in schizophrenia: the roles of negative symptoms, cognition, and functional capacity. Schizophr Res. 2015;165(1):76–82. doi:10.1016/j.schres.2015.03.033
17. Galderisi S, Rucci P, Kirkpatrick B, et al. Interplay among psychopathologic variables, personal resources, context-related factors, and real-life functioning in individuals with schizophrenia a network analysis. JAMA Psychiatry. 2018;75(4):396–404. doi:10.1001/jamapsychiatry.2017.4607
18. Gupta M, Bassett E, Iftene F, Bowie CR. Functional outcomes in schizophrenia: understanding the competence-performance discrepancy. J Psychiatr Res. 2012;46(2):205–211. doi:10.1016/j.jpsychires.2011.09.002
19. Davies G, Fowler D, Greenwood K. Metacognition as a mediating variable between neurocognition and functional outcome in first episode psychosis. Schizophr Bull. 2017;43(4):824–832. doi:10.1093/schbul/sbw128
20. Cardenas V, Abel S, Bowie CR, et al. When functional capacity and real-world functioning converge: the role of self-efficacy. Schizophr Bull. 2013;39(4):908–916. doi:10.1093/schbul/sbs004
21. Nemoto T, Uchino T, Aikawa S, et al. Social anxiety and negative symptoms as the characteristics of patients with schizophrenia who show competence-performance discrepancy in social functioning. Psychiatry Clin Neurosci. 2019;73:394–399. doi:10.1111/pcn.12848
22. Rapee RM, Spence SH. The etiology of social phobia: empirical evidence and an initial model. Clin Psychol Rev. 2004;24(7):737–767. doi:10.1016/j.cpr.2004.06.004
23. Brandes M, Bienvenu OJ. Personality and anxiety disorders. Curr Psychiatry Rep. 2006;8(4):263–269. Available from: http://www.ncbi.nlm.nih.gov/pubmed/16879789.
24. Kampman O, Viikki M, Leinonen E. Anxiety disorders and temperament-an update review. Curr Psychiatry Rep. 2017;19(5):27. doi:10.1007/s11920-017-0779-5
25. McEnery C, Lim MH, Tremain H, Knowles A, Alvarez-Jimenez M. Prevalence rate of social anxiety disorder in individuals with a psychotic disorder: a systematic review and meta-analysis. Schizophr Res. 2019. doi:10.1016/j.schres.2019.01.045
26. Vrbova K, Prasko J, Ociskova M, Holubova M. Comorbidity of schizophrenia and social phobia - impact on quality of life, hope, and personality traits: a cross sectional study. Neuropsychiatr Dis Treat. 2017;13:2073–2083. doi:10.2147/NDT.S141749
27. Roberts BW. Back to the future: personality and assessment and personality development. J Res Pers. 2009;43(2):137–145. doi:10.1016/j.jrp.2008.12.015
28. Ohi K, Hashimoto R, Yasuda Y, et al. Personality traits and schizophrenia: evidence from a case-control study and meta-analysis. Psychiatry Res. 2012;198(1):7–11. doi:10.1016/j.psychres.2011.12.018
29. Ohi K, Shimada T, Nitta Y, et al. The Five-Factor Model personality traits in schizophrenia: a meta-analysis. Psychiatry Res. 2016;240:34–41. doi:10.1016/j.psychres.2016.04.004
30. Cloninger CR, Svrakic DM, Przybeck TR, A psychobiological model of temperament and character. Arch Gen Psychiatry. 1993;50(12):975–990. doi:10.1001/archpsyc.1993.01820240059008
31. Compton MT, Bakeman R, Alolayan Y, et al. Personality domains, duration of untreated psychosis, functioning, and symptom severity in first-episode psychosis. Schizophr Res. 2015;168(1–2):113–119. doi:10.1016/j.schres.2015.06.028
32. Gurrera RJ, McCarley RW, Salisbury D. Cognitive task performance and symptoms contribute to personality abnormalities in first hospitalized schizophrenia. J Psychiatr Res. 2014;55(1):68–76. doi:10.1016/j.jpsychires.2014.03.022
33. Hori H, Fujii T, Yamamoto N, et al. Temperament and character in remitted and symptomatic patients with schizophrenia: modulation by the COMT Val158Met genotype. J Psychiatr Res. 2014;56:82–89. doi:10.1016/j.jpsychires.2014.05.006
34. Guillem F, Pampoulova T, Rinaldi M, Stip E. Temperament and executive dysfunctions in schizophrenia. Schizophr Res. 2008;104(1–3):175–184. doi:10.1016/j.schres.2008.06.002
35. Jetha MK, Goldberg JO, Schmidt LA. Temperament and its relation to social functioning in schizophrenia. Int J Soc Psychiatry. 2013;59(3):254–263. doi:10.1177/0020764011433639
36. Lysaker PH, Wilt MA, Plascak-Hallberg CD, Brenner CA, Clements CA. Personality dimensions in schizophrenia: associations with symptoms and coping. J Nerv Ment Dis. 2003;191(2):80–86. doi:10.1097/01.NMD.0000050936.81128.5B
37. Lysaker PH, Davis LW. Social function in schizophrenia and schizoaffective disorder: associations with personality, symptoms and neurocognition. Health Qual Life Outcomes. 2004;2:15. doi:10.1186/1477-7525-2-15
38. Kentros MK, Terkelsen K, Hull J, Smith TE, Goodman M. The relationship between personality and quality of life in persons with schizoaffective disorder and schizophrenia. Qual Life Res. 1997;6(2):118–122. http://www.ncbi.nlm.nih.gov/pubmed/9161111.
39. Kahn RS, Sommer IE, Murray RM, et al. Schizophrenia. Nat Rev Dis Prim. 2015;1:15067. doi:10.1038/nrdp.2015.67
40. Birchwood M, Smith J, Cochrane R, Wetton S, Copestake S. The Social Functioning Scale. The development and validation of a new scale of social adjustment for use in family intervention programmes with schizophrenic patients. Br J Psychiatry. 1990;157:853–859. doi:10.1192/bjp.157.6.853
41. Nemoto T, Fujii C, Miura Y, et al. Reliability and validity of the Social Functioning Scale Japanese version (SFS-J). JPN Bull Soc Psychiat. 2008;17:188–195.
42. Mausbach BT, Harvey PD, Goldman SR, Jeste DV, Patterson TL. Development of a brief scale of everyday functioning in persons with serious mental illness. Schizophr Bull. 2007;33(6):1364–1372. doi:10.1093/schbul/sbm014
43. Sumiyoshi C, Takaki M, Okahisa Y, Patterson TL, Harvey PD, Sumiyoshi T. Utility of the UCSD performance-based skills assessment-brief Japanese version: discriminative ability and relation to neurocognition. Schizophr Res Cogn. 2014;1(3):137–143. doi:10.1016/j.scog.2014.08.002
44. Igarashi Y, Hayashi N, Yamashina M, et al. Interrater reliability of the Japanese version of the Positive and Negative Syndrome Scale and the appraisal of its training effect. Psychiatry Clin Neurosci. 1998;52(5):467–470. doi:10.1046/j.1440-1819.1998.00425.x
45. Kay SR, Fiszbein A, Opler LA, The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull. 1987;13(2):261–276. doi:10.1093/schbul/13.2.261
46. Kaneda Y, Sumiyoshi T, Keefe R, Ishimoto Y, Numata S, Ohmori T. Brief assessment of cognition in schizophrenia: validation of the Japanese version. Psychiatry Clin Neurosci. 2007;61(6):602–609. doi:10.1111/j.1440-1819.2007.01725.x
47. Keefe RSE, Harvey PD, Goldberg TE, et al. Norms and standardization of the Brief Assessment of Cognition in Schizophrenia (BACS). Schizophr Res. 2008;102(1–3):108–115. doi:10.1016/j.schres.2008.03.024
48. Kijima N, Tanaka E, Suzuki N, Higuchi H, Kitamura T. Reliability and validity of the Japanese version of the Temperament and Character Inventory. Psychol Rep. 2000;86(3 Pt 1):1050–1058. doi:10.2466/pr0.2000.86.3.1050
49. Vespa A, Ottaviani M, Fossati A, et al. Validation of the Italian translation of the Revised Temperament and Character Inventory - TCI-140 - in adult participants and in participants with medical diseases. Compr Psychiatry. 2015;59:129–134. doi:10.1016/j.comppsych.2014.12.006
50. Becattini-Oliveira AC, de Dutra DF, Spenciere de Oliveira Campos B, de Araujo VC, Charchat-Fichman H. A systematic review of a functional assessment tool: UCSD performance-based skill assessment (UPSA). Psychiatry Res. 2018;267:12–18. doi:10.1016/j.psychres.2018.05.005
51. Ravaja N, Keltikangas-Järvinen L, Kettunen J. Cloninger’s temperament dimensions and threat, stress, and performance appraisals during different challenges among young adults. J Pers. 2006;74(1):287–310. doi:10.1111/j.1467-6494.2005.00376.x
52. Poustka L, Murray GK, Jääskeläinen E, et al. The influence of temperament on symptoms and functional outcome in people with psychosis in the Northern Finland 1966 Birth Cohort. Eur Psychiatry. 2010;25(1):26–32. doi:10.1016/j.eurpsy.2009.09.006
53. Olsson AK, Hjärthag F, Helldin L. Predicting real-world functional milestones in schizophrenia. Psychiatry Res. 2016;242:1–6. doi:10.1016/j.psychres.2016.05.015
54. Kalin M, Kaplan S, Gould F, Pinkham AE, Penn DL, Harvey PD. Social cognition, social competence, negative symptoms and social outcomes: inter-relationships in people with schizophrenia. J Psychiatr Res. 2015;68:254–260. doi:10.1016/j.jpsychires.2015.07.008
55. Ventura J, Hellemann GS, Thames AD, Koellner V, Nuechterlein KH. Symptoms as mediators of the relationship between neurocognition and functional outcome in schizophrenia: a meta-analysis. Schizophr Res. 2009;113(2–3):189–199. doi:10.1016/j.schres.2009.03.035
56. Leifker FR, Patterson TL, Heaton RK, Harvey PD. Validating measures of real-world outcome: the results of the VALERO expert survey and RAND panel. Schizophr Bull. 2011;37(2):334–343. doi:10.1093/schbul/sbp044
57. Fresán A, León-Ortiz P, Robles-García R, et al. Personality features in ultra-high risk for psychosis: A comparative study with schizophrenia and control subjects using the Temperament and Character Inventory-Revised (TCI-R). J Psychiatr Res. 2015;61:168–173. doi:10.1016/j.jpsychires.2014.12.013
58. Song YY, Kang JI, Kim SJ, Lee MK, Lee E, An SK. Temperament and character in individuals at ultra-high risk for psychosis and with first-episode schizophrenia: associations with psychopathology, psychosocial functioning, and aspects of psychological health. Compr Psychiatry. 2013;54(8):1161–1168. doi:10.1016/j.comppsych.2013.05.015
59. Lönnqvist J-E, Verkasalo M, Haukka J, et al. Premorbid personality factors in schizophrenia and bipolar disorder: results from a large cohort study of male conscripts. J Abnorm Psychol. 2009;118(2):418–423. doi:10.1037/a0015127
60. Bora E, Veznedaroglu B. Temperament and character dimensions of the relatives of schizophrenia patients and controls: the relationship between schizotypal features and personality. Eur Psychiatry. 2007;22(1):27–31. doi:10.1016/j.eurpsy.2006.07.002
61. Glatt SJ, Stone WS, Faraone SV, Seidman LJ, Tsuang MT. Psychopathology, personality traits and social development of young first-degree relatives of patients with schizophrenia. Br J Psychiatry. 2006;189:337–345. doi:10.1192/bjp.bp.105.016998
62. Smith MJ, Cloninger CR, Harms MP, Csernansky JG. Temperament and character as schizophrenia-related endophenotypes in non-psychotic siblings. Schizophr Res. 2008;104(1–3):198–205. doi:10.1016/j.schres.2008.06.025
63. McCarthy NS, Badcock JC, Clark ML, et al. Assessment of cognition and personality as potential endophenotypes in the Western Australian family study of schizophrenia. Schizophr Bull. 2018;44(4):908–921. doi:10.1093/schbul/sbx141
64. Almerie MQ, Okba Al Marhi M, Jawoosh M, et al. Social skills programmes for schizophrenia. Cochrane Database Syst Rev. 2015;(6):CD009006. doi:10.1002/14651858.CD009006.pub2
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.