Back to Journals » Risk Management and Healthcare Policy » Volume 11
Associations between structures and resources of primary care at the district level and health outcomes: a case study of diabetes mellitus care in Thailand
Authors Komwong D, Sriratanaban J
Received 13 June 2018
Accepted for publication 5 September 2018
Published 26 October 2018 Volume 2018:11 Pages 199—208
DOI https://doi.org/10.2147/RMHP.S177125
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Kent Rondeau
Daoroong Komwong,1,2 Jiruth Sriratanaban1,3
1Department of Preventive and Social Medicine, Faculty of Medicine, Chulalongkorn University, Bangkok, Thailand; 2Sirindhorn College of Public Health, Praboromarajchanok Institute of Health Workforce Development, Chon Buri, Thailand; 3Thailand Research Center for Health Services System, Faculty of Medicine, Chulalongkorn University, Bangkok, Thailand
Background: The structural factors of primary care potentially influence its performance and quality. This study investigated the association between structural factors, including available primary care resources and health outcomes, by using diabetes-related ambulatory care sensitive conditions hospitalizations under the Universal Coverage Scheme in Thailand.
Methods: A 2-year panel study used secondary data compiled at the district level. Administrative claim data from 838 districts during the 2014–2015 fiscal years from the National Health Security Office were used to analyze overall diabetes mellitus (DM) hospitalizations and its three subgroups: hospitalizations for uncontrolled diabetes, short-term complications, and long-term complications. Primary care structural data were obtained from the Ministry of Public Health. Generalized estimating equations were used to estimate the influence of structural factors on the age-standardized DM hospitalization ratio.
Results: A higher overall DM and uncontrolled diabetes hospitalization ratio was related to an increasing concentration of outpatient utilization (using the Herfindahl–Hirschman Index) (overall DM; beta [standard error, SE]=0.003 [0.001], 95% CI 0.000, 0.006) and decreasing physician density and bed supply (overall DM; beta [SE]=−1.350 [0.674], 95% CI –2.671, –0.028), beta [SE]=−0.023 [0.011], 95% CI −0.045, –0.001, respectively). Hospitalizations for short-term complications increased with a decrease in health care facility density, whereas hospitalizations for long-term complications increased as that density increased. Rurality was strongly associated with higher hospitalization ratios for all DM hospitalizations except short-term complications.
Conclusions: This study identified structural factors associated with health outcomes, many of which can be changed through reorganization at the district level.
Keywords: primary care, structural characteristics, health human resources, ambulatory care sensitive conditions, diabetes mellitus
Erratum for this paper has been published
Introduction
Primary care serves as a cornerstone of a functional health system. Improvement of primary care systems could lead to better population health outcomes, equity in health care and the optimization of resource utilization.1,2 Previous studies have reported an association between improved quality of primary care and reduced mortality rate, reduced health care costs, and improved health outcomes, particularly among patients with chronic conditions.3–5 The improvement depends on patient- and physician-related factors,6 particularly structural and organizational characteristics, including the health care system, the practice context, and the organization of the practice, such as health and human resources, infrastructure, and organizational structure and dynamics.7 These structural and organizational characteristics have a meaningful impact on the performance and quality of primary care. A greater number of primary care resources are associated with improved hospital performance through lower hospitalization rates for chronic disease.8 An adequate physician supply9 and high continuity of care have strong positive effects on reducing avoidable hospitalizations.10
In Thailand, extensive geographical coverage of a primary care system is recognized as one of the essential components of universal health coverage.11 Health delivery systems are dominated by the public sector, and most public health care facilities fall under the Ministry of Public Health (MOPH). Other public health care facilities fall under other ministries and local government, but these represent a very small proportion. The district health office oversees all health centers in the district and coordinates with the district hospital to manage the district health system. At the primary care level, public health centers offer basic health services at the sub-district level, as do municipal health centers in urban areas. The main staff of public health centers are registered nurses, public health officers (4 years of training), and other health professionals (2 years of training). Approximately 5% of public health centers have at least one physician, and most of them are generalist physicians (6 years of training).12 One recent national reform in the newest constitution of Thailand in 2017 is to better equip family physicians in the primary care system.13 To lead this reform effort, it can be expected that more resources will be provided to strengthen primary care. However, it is unclear whether and how the primary care structure, including the available resources, can be used to guide resource allocation and structural organization to improve population health outcomes in Thailand.
In this study, diabetes care outcomes were determined by using hospitalizations for ambulatory care sensitive conditions (ACSCs), which have been used as a proxy indicator of primary care quality and accessibility. Hospitalizations for ACSCs can be prevented through timely, accessible, and high-quality primary care or outpatient care.14,15
Diabetes mellitus (DM) was selected as the tracer for population health outcomes since the rapid increase of an aging population has resulted in an increasing burden of noncommunicable diseases in Thailand.16,17 The diabetes care process is complex and is delivered across care providers and practice settings. Because hospitalized patients with well-controlled DM are referred for treatment at their primary care centers, it is a major challenge for a primary care system to provide integrated and continuing care for better chronic health outcomes. It is reasonable to believe that diabetes care outcomes reflect the organizational structures, resource allocation, and management of primary care. Therefore, an objective of this study is to investigate the association between the structural factors of primary care and population health outcomes at the district level through DM hospitalizations.
Methods
Study design and population
A 2-year panel study was conducted using secondary data from public health care facilities, including the hospitals and primary care centers of 838 districts, 76 provinces, and 12 regions of Thailand. All public health care facilities were organized by the Office of the Permanent Secretary (OPS) and the MOPH, excluding Bangkok province and Pattaya city due to a special local government organization that is an independent authority. The study population included the Universal Coverage Scheme (UCS), the largest scheme among the three public health insurance schemes of Thailand’s universal health care coverage, which covers 75% of the Thai population. All DM patients under the UCS were used for the analysis in this study.
Outcome variables
The outcomes of interest included overall DM hospitalizations and its three subgroups, ie, hospitalizations for uncontrolled diabetes, short-term complications, and long-term complications. Hospitalization for short-term complications is defined as including diabetic ketoacidosis, hyperosmolarity, and coma. Hospitalization for long-term complications includes renal, eye, neurological, and circulatory disorders. Hospitalization for uncontrolled diabetes includes discharges with a principal diagnosis without mention of short-term or long-term complications.18 Data on hospitalizations were obtained from the administrative claims database of the National Health Security Office (NHSO) during the fiscal years 2014–2015 (October 1, 2013, to September 30, 2015). The number of DM hospitalizations was calculated at the district level by aggregating patient levels using ICD-10 codes identified by the Agency for Healthcare Research and Quality.18 The crude hospitalization rate was calculated by the number of discharges with the ICD-10 principal diagnosis code divided by the number of the population under the UCS aged 15 years and older. The age-standardized hospitalization ratio was computed by dividing the observed number by the expected number of hospitalizations. The expected number is the number of hospitalizations that would be expected in the same patients in three age groups: 15–35, 36–60, and over 60 years.
Primary care structural variables
All primary care structural variables were aggregated from individual health care facilities to the district level of analysis. The key structural variables included in this study were concentration of outpatient utilization, density of health care facilities, bed supply, financial status, quality improvement status, health human resources, and location of the districts.
The data used in this study were collected from various sources during the two fiscal years. Public health care facilities data, including the type of facility (regional, general, or district hospital or health care center), district and province codes, number of active beds, and outpatient utilization, were obtained from the Bureau of Policy and Strategy of the MOPH. Data for health human resources supply, including physicians, family medicine physicians, nurses, pharmacists, and other health professionals (public health technical officers, public health officers, dental assistants, and pharmacy technicians), were obtained from the Personnel Administrative Division of the MOPH. In addition, the financial status data were obtained from the Health Insurance Group of the OPS, MOPH, and the quality improvement status was obtained from the Healthcare Accreditation Institute (public organization). The locations and the systems of local government bodies were collected from the Department of Local Administration of the Ministry of the Interior.
The concentration of outpatient utilization within each district was measured by the Herfindahl–Hirschman Index (HHI). The HHI value, which was calculated by summing the square of the proportion of the outpatient utilization of each health care facility (market shares) to the total outpatient utilization in the district, presents a view of how the outpatient utilization of a district is distributed. A higher HHI value reflects more outpatient utilization among a few dominant health care facilities, whereas a lower HHI value indicates that there is no dominant health care facility and that outpatient utilization is more evenly distributed across the district. Based on the HHI value, the districts were categorized into three groups: unconcentrated (HHI<1,500), moderately concentrated (HHI 1,500–2,500), and highly concentrated (HHI>2,500).19 Health care facility density was expressed by dividing the number of all public health facilities by 100 km2. Bed supply included all active beds in public hospitals organized by the OPS, MOPH. Health human resources supply was calculated as density per 10,000 people under the UCS aged 15 years and over. Financial status was assessed by using the quarterly MOPH financial risk scoring. The assessment was based on six items: current ratio <1.5 (1 point), quick ratio <1.0 (1 point), cash ratio <0.8 (1 point), net working capital <0 (1 point), net income (including depreciation)<0 (1 point), and average net income 4–6 months (1 point) or 0–3 months (2 points). The districts that scored 7 for more than or equal to 6 of 12 quarters (over the previous two fiscal years and the current fiscal year) were indicated by MOPH to be experiencing a financial crisis. Achieving the sustainable accreditation program was identified by whether a hospital within a district was granted a 3-year accreditation by the Healthcare Accreditation Institute (public organization) for at least 6 months within a fiscal year. The location of the district was identified by the local government system to indicate whether the district was rural or urban. Local administrative authorities were divided into three municipal levels: city (more than 50,000 inhabitants), town (more than 10,000 inhabitants), and subdistrict municipalities. Districts located outside cities and towns were defined as rural.
Control variables
This study selected population and DM patient characteristics as control variables. These characteristics may be potential confounders of the relationship.6,14 The population characteristics variables are the proportion of the population aged more than 60 years to the total population aged 15 years and older and DM prevalence (number of DM patients to total population aged 15 years and older). The patient characteristic variables are the proportion of DM patients aged more than 60 years to total DM patients, the proportion of DM patients who graduated at a lower level than secondary school to total DM patients, the duration of DM, and the severity of comorbidity as measured by the Charlson Comorbidity Index (CCI).20 Based on the CCI score, the severity of comorbidity in DM patients was categorized into three groups: mild (scores 1–2), moderate (scores 3–4), and severe (scores ≥5).21
Statistical analysis
Descriptive statistics were used to summarize the structure of primary care, population characteristics, DM patient characteristics, and DM hospitalizations. Normally distributed variables were reported as the mean (SD), and non-normally distributed variables were reported as the median (Q1–Q3). Due to the longitudinal nature of the 2-year panel data, a generalized estimating equation method was used to estimate the association between structural factors of primary care and age-standardized DM hospitalization ratio (observed vs the expected number of DM hospitalizations). According to the continuous outcome, the Gaussian family and identity link function were selected, and the exchangeable working correlation matrix was chosen. Covariate variables of population and DM patient characteristics were included to adjust the model for analysis. A significance level of P<0.05 was considered significant throughout the study.
Results
Primary care structure and distribution
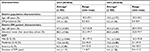
In 838 districts, there were 10,446 primary care centers and hospitals, of which the concentration varied across the areas. Half of all the districts had a high concentration of outpatient utilization based on an HHI value greater than 2,500 each year. There were approximately three public providers per 100 km2, and two-thirds of all districts had between 30 and 90 beds. The percentage of districts experiencing a financial crisis declined from 12.6% in 2014 to 8.5% in 2015. More than 80% of the districts were located in rural areas (Table 1). The average number of physicians per 10,000 population was 4.3 and 3.9 in 2014 and 2015, respectively. The percentage of districts with at least one family medical practice increased from 30.7% in 2014 to 34.6% in 2015 (Table 2).
District population and DM patient characteristics
The population over 60 years of age made up approximately 20% of the total UCS population. The prevalence of DM among the UCS population aged 15 years and older increased from 3.9 in 2014 to 4.5 in 2015, whereas DM patients aged more than 60 declined slightly, from 47.2% in 2014 to 45.4% in 2015. More than 80% of the patients had a level of education lower than secondary school. The average duration of DM was 4 years, and approximately 75% of the patients had a CCI score between 0 and 2 yearly (Table 3).
Hospitalizations for diabetes-related ambulatory care sensitive conditions
The number of overall DM admissions was 57,417 and 65,944 in 2014 and 2015, respectively. Nationwide, the crude overall DM hospitalization rate increased from 169 (per 100,000 population) in 2014 to 193 in 2015. Similarly, the number and the crude hospitalization rates of uncontrolled diabetes, short-term complications, and long-term complications increased from 2014 to 2015 (Table 4).
Associations between structures and resources of primary care at the district level and age-standardized DM hospitalization ratio
The standardized hospitalization ratios for overall DM and uncontrolled diabetes had a significant positive association with the HHI value (overall DM; beta [standard error, SE]=0.003 [0.001], 95% CI 0.000, 0.006) but a negative association with the physician density and bed supply (overall DM; beta [SE]=−1.350 [0.674], 95% CI −2.671, –0.028), beta [SE]=−0.023 [0.011], 95% CI −0.045, –0.001, respectively). An increase in health care facility density was associated with a lower ratio of short-term complications and a higher ratio of long-term complications. Higher standardized hospitalization ratios for overall DM, uncontrolled diabetes, and long-term complications were strongly associated with districts located in rural areas (Table 5).
Discussion
Our study found that factors of the primary care structure and resources were relevant determinants of better health outcomes, as measured by the lower standardized DM hospitalization ratio, including higher health care facility density (in the case of short-term complications), a lower concentration of outpatient utilization, and higher physician density and bed supply. In addition, rurality was significantly associated with an increase in hospitalization ratio and thus poorer health outcomes.
First, the health care facility density variable may reflect the district health service structure and accessibility. People in areas with higher density might have easy access to primary care within a radius of 10 km. Conversely, areas with lower density might indicate that people must travel farther from home to the nearest primary care center. In addition, an area with more health care facilities might indicate the presence of more health human resources that operate and deliver preventive and health promotion programs to improve health services coverage. This finding aligns with previous studies regarding ease of access to primary care as one of the major determinants of health outcomes.22 For example, evidence from a systematic review focusing on hospitalization rates for ACSCs and accessibility confirmed that lower rates were found in areas with greater access to primary care settings.14
The findings of this study showed that hospitalizations for short-term complications were negatively correlated with health care facility density and positively associated with long-term complications. The benefits of having more health care facilities and health care professionals in an area might be reduced by barriers that limit the timely response to acute life-threatening illness, such as short-term complications of DM. More timely access would result in relief of illness severity at prehospital stages and help to prevent emergency hospitalizations. Such associations have been consistently observed, for example, in a previous study that reported that improving timely access to primary care for early treatment of exacerbations resulted in a lower rate of emergency admissions for asthma.23
However, the development and progression of long-term complications are dependent on not only accessibility but also the continuity of care10 as well as patient awareness and self-management24 over long periods. Moreover, the presence of an increase of hospitalizations for long-term complications might be due to less effective preventive care and chronic disease management in primary care over a long period.10,15 Thus, it may be assumed that hospitalizations for long-term complications cannot reflect the structure of health care facilities within a 2-year period of analysis. Long-term outcomes might be a consequence of the complex accumulation of multiple factors over a long period. Therefore, the analysis should be interpreted with considerable caution. Examination of both inpatient and outpatient data as well as patients’ lifestyle may provide a more complete picture of this relationship.
Second, this study found that the structural variable of primary care, namely, the outpatient utilization concentration, was positively correlated with hospitalizations for ACSCs. This index may represent the structure of outpatient utilization and the available choices of health care facilities in the area. These findings differ from previous results reported in the literature, such as a study among Medicaid patients that indicated that a higher concentration of Medicaid care enrollment affected better access to care and was negatively associated with hospitalizations for ACSCs25 and a study of asthmatic children that showed that a higher concentration of patient visits increased continuity of care and led to a reduced rate of hospitalizations for ACSCs.26 However, another study found no significant impact of structural concentration on the rate of hospitalizations for ACSCs.27 Background differences in health services systems across countries may be an important cause of the differences in these results.
Most primary care centers in Thailand have only a nurse and/or other health care professionals who play a key role, whereas physicians are available only in district hospitals; patients can move directly from a primary care center to a hospital with no barriers.12 Patients’ perceptions of service quality might vary based on provider type.28 Patients’ perceptions of outpatient services in the primary care settings of Thailand showed significant differences between perceptions and expectations,29,30 and the two largest gaps were detected in the responsiveness and reliability dimensions.30 These gaps might be attributable to a marked shift in outpatient visits from primary care centers to hospital outpatient departments, even for primary health care needs or common conditions. This situation might potentially increase providers’ workload and thus affect the quality of care. Conversely, in circumstances with a more evenly distributed outpatient utilization without a dominant facility, health professionals can provide higher quality care throughout their catchment area with a lower workload. As a result, the hospitalization rate might decrease as the concentration decreases. Future in-depth studies are needed.
Third, our finding of the effects of human resources is consistent with previous evidence from a systematic review that found an association between DM hospitalizations and the level of primary care resources.8 Health human resources are identified as one of the core building blocks of a health system, and a relationship has been demonstrated between the health care workforce, especially the primary care physician supply, and better health outcomes.1 Evidence from a recent systematic review9 and previous studies across countries31–33 revealed an inverse association between physician supply and the rates of admissions for ACSCs, particularly in older patients with chronic conditions such as DM and asthma. It is reasonable to assume that in a district with more physicians, patients can be treated thoroughly and effectively, and better health outcomes will result from the reduction of hospitalizations for ACSCs.
Moreover, hospitalizations for ACSCs were found to be significantly lower in districts with more beds. In the context of Thailand, the number of active beds refers to the level of the hospital. Differences in hospital level could indicate differences in the type of practice, the availability of advanced services, such as medical investigation and equipment, and the presence of specialists or multidisciplinary care.12 Hence, the total bed number in each district is a proxy reflecting capabilities rather than availability. A facility with more beds can support more staff who can more easily observe and evaluate patients in the process of care; thus, the facility might have a lower hospitalization rate than a district with a lower bed supply.
Despite the significant factors of primary care structure and resources, our multiple regression model showed that rurality remained a predictor of DM outcomes. This finding is consistent with previous studies that found that rurality is a determinant of increases in hospitalizations for ACSCs,32,34–36 highlighting disparities in accessibility, ability to receive timely treatment, and/or the effectiveness of ambulatory care in rural areas. Rurality itself might be a proxy of unobserved environmental and other contextual factors that influence health outcomes. A possible explanation for rurality may be that rural areas in Thailand often lack public transport alternatives, especially for people who do not live near highways and main roads. In addition, some remote areas encounter poor weather conditions and therefore have poor access to health services.37,38
Furthermore, people in rural communities often experience certain social factors such as poverty and unemployment, which can contribute to health status. Poor health literacy is a problem in areas with more poverty and less education.22 These factors may be complemented by the existing barriers. In this study, we found that the percentage of patients who had graduated at a lower level than secondary school was lower in rural districts than in urban districts by approximately 10%.
We expected to demonstrate that other health care professionals, such as nurses, may affect health outcomes because they play a crucial role in primary care settings. These findings do not support previous research in this area.39,40 A possible reason for this apparent lack of correlation between the nurse supply and health outcomes is that this variable might correlate with another significant supply-related variable, such as number of physicians and hospital beds. Therefore, it does not show a significant relationship. Another possible explanation is that the number of nurses per 10,000 population did not vary among the districts or might be higher than the critical threshold to affect the performance of primary care in the context of Thailand.
We recognize that the present study might have some limitations. First, among a wide range of health problems that could be managed at the primary care level, we used only diabetes care and DM hospitalizations to trace the accessibility, quality, and outcomes of primary care. Previous studies showed that different system factors in primary care might affect disease outcomes differently.41,42 However, diabetes is a common health problem in Thailand with increasing prevalence. We strongly believe that diabetes care can reflect primary care performance in all dimensions, including access to care, prevention and treatment effectiveness, and continuity of care, as well as the coordination of health care providers at all levels in an area. Additionally, hospitalizations for ACSCs can be used as an easy and inexpensive screening tool. The high heterogeneity found in the hospitalization rates for ACSCs suggests critical area differences in the quality of primary care. However, these indicators may be influenced by certain factors outside the health care system, such as socioeconomic status, poor environmental conditions, and lack of patient adherence to treatment.15,43 In this study, we were unable to consider a number of potential confounding factors.
Second, the differences in units of analysis were dependent on the administrative structure that provides independent care in each country. In this study, the district was used as a unit of analysis because in Thailand, the district health network can be managed independently under national and provincial policy. Previous studies across countries selected varying geographical units;44 therefore, comparisons should be treated with considerable caution.
Third, differences in contextual factors might limit the generalizability of the findings across countries, particularly the existence of universal health coverage and the dominant public system in Thailand that remove the direct financial barrier. However, other barriers to accessing care may exist, such as barriers to geographical access38 or a lack of availability of caretakers to take patients, particularly older patients, to health facilities.37
Further research is needed to understand what accounts for a higher likelihood of hospitalizations in areas with a low number of health care facilities and physician density, and a higher concentration of outpatient visits and in rural areas. More broadly, to confirm our findings, research is needed to determine the association between the structures and resources of primary care and hospitalizations for ACSCs in other categories conditions, such as acute or vaccine-preventable conditions.
Conclusion
The structural factors and health resources of primary care were associated with population health outcomes at the district level through DM hospitalization. Better health outcomes were related to a decreasing concentration of outpatient utilization and increasing physician density, bed supply, and health care facility density (in the case of short-term complications). Additionally, rurality was related to higher hospitalization and thus to poorer health outcomes. Reorganization at the district level is required to restructure these factors for better population health. Policymakers should implement health intervention programs and health policies to achieve better outcomes through health resources and the distribution of outpatient utilization, particularly in rural areas. The hospitalization rates for ACSCs may serve as a useful benchmark indicator between and within areas for policymakers to prioritize and target efforts to reduce the gap in health outcomes.
Ethics approval and informed consent
The study protocol was approved by the Institutional Review Board, Faculty of Medicine, Chulalongkorn University, Bangkok, Thailand. The reference number was 156/59. Since all of the data in the study were secondary data, written informed consent was not possible. Participants’ confidentiality was ensured by data protection and encrypted data. The data were used with the permission of NHSO and MOPH, and the data cannot be shared.
Data availability
None of the datasets generated and analyzed during the current study are publicly available. This is due to the need to protect participant confidentiality as agreed upon with all of the data sources. For DM, hospitalization rates under the UCS were publicly available in the NHSO annual reports. However, the data definition and scope of analysis were different from those used in this study.45
Acknowledgments
The authors would like to thank the staffs of the NHSO, Bureau of Policy and Strategy, MOPH, Bureau of Inspection and Evaluation, Division of Personnel Administrative, MOPH, and The Health Insurance Group, MOPH for preparing and providing the data. The authors would also like to acknowledge the 90th Anniversary of Chulalongkorn University Fund (Ratchadaphiseksomphot Endowment Fund), Chulalongkorn University Graduate Scholarship, and the National Research Council of Thailand (NRCT) for funding this study. This study was funded by the 90th Anniversary of Chulalongkorn University Fund (Ratchadaphiseksomphot Endowment Fund), Chulalongkorn University Graduate Scholarship, and the NRCT.
Author contributions
DK and JS were involved in the conception and study design. DK participated in the data collection, data analysis, and drafted the manuscript. JS contributed to reading and revising the manuscript. All the authors read and approved the final manuscript. All authors contributed toward data analysis, drafting and revising the paper and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
Starfield B, Shi L, Macinko J. Contribution of primary care to health systems and health. Milbank Q. 2005;83(3):457–502. | ||
Starfield B. Primary Care and Equity in Health: The Importance to Effectiveness and Equity of Responsiveness to Peoples’ Needs. Humanity Soc. 2009;33(1–2):56–73. | ||
Mcelduff P, Lyratzopoulos G, Edwards R, Heller RF, Shekelle P, Roland M. Will changes in primary care improve health outcomes? Modelling the impact of financial incentives introduced to improve quality of care in the UK. Qual Saf Health Care. 2004;13(3):191–197. | ||
Martin S, Smith P, Gravelle H, Rice N. Evidence: Do Quality Improvements in Primary Care Reduce Secondary Care Costs? London: The Health Foundation; 2011. Available from: http://www.health.org.uk/sites/health/files/DoQualityImprovementsInPrimaryCareReduceSecondaryCareCosts_summary.pdf. Accessed April 28, 2017. | ||
Shin DW, Cho J, Yang HK, et al. Impact of continuity of care on mortality and health care costs: a nationwide cohort study in Korea. Ann Fam Med. 2014;12(6):534–541. | ||
Mosadeghrad AM. Factors influencing healthcare service quality. Int J Health Policy Manag. 2014;3(2):77–89. | ||
Hogg W, Rowan M, Russell G, Geneau R, Muldoon L. Framework for primary care organizations: the importance of a structural domain. Int J Qual Health Care. 2008;20(5):308–313. | ||
Gibson OR, Segal L, Mcdermott RA. A systematic review of evidence on the association between hospitalisation for chronic disease related ambulatory care sensitive conditions and primary health care resourcing. BMC Health Serv Res. 2013;13(1):336. | ||
van Loenen T, van den Berg MJ, Westert GP, Faber MJ. Organizational aspects of primary care related to avoidable hospitalization: a systematic review. Fam Pract. 2014;31(5):502–516. | ||
van Loenen T, Faber MJ, Westert GP, van den Berg MJ. The impact of primary care organization on avoidable hospital admissions for diabetes in 23 countries. Scand J Prim Health Care. 2016;34(1):5–12. | ||
UHC Coalition. Thailand: At the forefront of Universal Health Coverage. Medium; 2016. Available from: https://medium.com/health-for-all/thailand-at-the-forefront-of-universal-health-coverage-d1bb9c0c3e79. Accessed April 29, 2017. | ||
World Health Organization, Asia Pacific Observatory on Health Systems and Policies. The Kingdom of Thailand Health System Review. Manila: WHO Regional Office for the Western Pacific; 2015. Available from: http://apps.who.int/iris/bitstream/handle/10665/208216/9789290617136_eng.pdf?sequence=1&isAllowed=y. Accessed October 6, 2017. | ||
Constitution of Thailand 2017. Available from: http://www.parliament.go.th/ewtcommittee/ewt/draftconstitution2/ewt_dl_link.php?nid=1038&filename=index. Accessed April 29, 2017. | ||
Rosano A, Loha CA, Falvo R, et al. The relationship between avoidable hospitalization and accessibility to primary care: a systematic review. Eur J Public Health. 2013;23(3):356–360. | ||
Agency for Healthcare Research and Quality. Prevention Quality Indicators Overview; 2016. Available from: https://www.qualityindicators.ahrq.gov/Modules/pqi_resources.aspx. Accessed April 1, 2017. | ||
Ariyapruchya K, Martin MES, Reungsri T, Luo X. Thailand Economic Monitor. Bangkok: The World Bank; 2016. Available from: http://documents.worldbank.org/curated/en/830261469638312246/pdf/107267-WP-PUBLIC-Thailand-Economic-Monitor-2016.pdf. Accessed April 29, 2017. | ||
Reutrakul S, Deerochanawong C. Diabetes in Thailand: Status and Policy. Curr Diab Rep. 2016;16(3):28. | ||
Agency for Healthcare Research and Quality. AHRQ – Quality Indicators. Available from: http://www.qualityindicators.ahrq.gov/Modules/PQI_TechSpec_ICD10_v70.aspx. Accessed April 26, 2018. | ||
Cutler DM, Hospitals SMF. Market Share, and Consolidation. JAMA. 2013;10(18):1964. | ||
Ramiarina RA, Ramiarina BL, Almeida RM, Pereira WC. Comorbidity adjustment index for the international classification of diseases, 10th revision. Rev Saude Publica. 2008;42(4):590–597. | ||
Huang YQ, Gou R, Diao YS, et al. Charlson comorbidity index helps predict the risk of mortality for patients with type 2 diabetic nephropathy. J Zhejiang Univ Sci B. 2014;15(1):58–66. | ||
Rural Health Information Hub. Social Determinants of Health for Rural People. Available from: https://www.ruralhealthinfo.org/topics/social-determinants-of-health. Accessed September 7, 2017. | ||
Fleetcroft R, Noble M, Martin A, Coombes E, Ford J, Steel N. Emergency hospital admissions for asthma and access to primary care: cross-sectional analysis. Br J Gen Pract. 2016;66(650):e640–e646. | ||
Nazar CM, Bojerenu MM, Safdar M, Marwat J. Effectiveness of diabetes education and awareness of diabetes mellitus in combating diabetes in the United Kigdom; a literature review. J Nephropharmacol. 2016;5(2):110–115. | ||
Park J, Lee KH. The association between managed care enrollments and potentially preventable hospitalization among adult Medicaid recipients in Florida. BMC Health Serv Res. 2014;14(1):247. | ||
Cho KH, Park EC, Nam YS, Lee SH, Nam CM, Lee SG. Impact of Market Competition on Continuity of Care and Hospital Admissions for Asthmatic Children: A Longitudinal Analysis of Nationwide Health Insurance Data 2009-2013. PLoS One. 2016;11(3):e0150926. | ||
Dietrichson J, Ellegard LM, Kjellsson G. Effects of Increased Competition on Quality of Primary Care in Sweden. Department of Economics, Lund University; 2016. Available from: http://project.nek.lu.se/publications/workpap/papers/wp16_36.pdf. Accessed September 3, 2017. | ||
Johnson DM, Russell RS, White SW. Perceptions of care quality and the effect on patient satisfaction. Inter J Qual Reliab Manag. 2016;33(8):1202–1229. | ||
Kongvaree K. Expectation and Perception of People Toward Service Quality of Tambon Health Promoting Hospital in Khlonglan District, Kamphaeng Phet Province [dissertation]. Nakorn Pathom: Mahidol University; 2013. | ||
Kaewkim W. Expectations and Perceptions of Health Service Recipients Toward Quality Service in Sub-district Health Promoting Hospitals, NakhonSi Thammarat Province [dissertation]. Nonthaburi: Sukhothai Thammathirat Open University; 2011. | ||
Weeks WB, Ventelou B, Paraponaris A. Rates of admission for ambulatory care sensitive conditions in France in 2009-2010: trends, geographic variation, costs, and an international comparison. Eur J Health Econ. 2016;17(4):453–470. | ||
Berlin C, Busato A, Rosemann T, Djalali S, Maessen M. Avoidable hospitalizations in Switzerland: a small area analysis on regional variation, density of physicians, hospital supply and rurality. BMC Health Serv Res. 2014;14:289. | ||
Chang CH, Stukel TA, Flood AB, Goodman DC. Primary care physician workforce and Medicare beneficiaries’ health outcomes. JAMA. 2011;305(20):2096–2104. | ||
Laditka JN, Laditka SB, Probst JC. Health care access in rural areas: Evidence that hospitalization for ambulatory care-sensitive conditions in the United States may increase with the level of rurality. Health Place. 2009;15(3):761–770. | ||
Thorpe JM, van Houtven CH, Sleath BL, Thorpe CT. Rural-urban differences in preventable hospitalizations among community-dwelling veterans with dementia. J Rural Health. 2010;26(2):146–155. | ||
Nayar P, Nguyen AT, Apenteng B, Yu F. Preventable hospitalizations: does rurality or non-physician clinician supply matter? J Community Health. 2012;37(2):487–494. | ||
The World Bank Closing the Health Gaps for the Elderly in Thailand. Available from: http://www.worldbank.org/en/country/thailand/publication/closing-the-health-gaps-for-the-elderly-in-thailand. Accessed October 4, 2017. | ||
Yingtaweesak T, Yoshida Y, Hemhongsa P, Hamajima N, Chaiyakae S. Accessibility of health care service in Thasongyang, Tak Province, Thailand. Nagoya J Med Sci. 2013;75(3–4):243–250. | ||
Nguyen MP, Mirzoev T, Le TM, Tm L. Contribution of health workforce to health outcomes: empirical evidence from Vietnam. Hum Resour Health. 2016;14(1):68. | ||
Clarke SP, Donaldson NE. Nurse Staffing and Patient Care Quality and Safety. In: Hughes RG, editor. Patient Safety and Quality: An Evidence-Based Handbook for Nurses. Rockville, MD: Agency for Healthcare Research and Quality; 2008. | ||
Rizza P, Bianco A, Pavia M, Angelillo IF. Preventable hospitalization and access to primary health care in an area of Southern Italy. BMC Health Serv Res. 2007;7:134. | ||
Busby J, Purdy S, Hollingworth W. How do population, general practice and hospital factors influence ambulatory care sensitive admissions: a cross sectional study. BMC Fam Pract. 2017;18(1):67. | ||
Gibbons DC, Bindman AB, Soljak MA, Millett C, Majeed A. Defining primary care sensitive conditions: a necessity for effective primary care delivery? J R Soc Med. 2012;105(10):422–428. | ||
Busby J, Purdy S, Hollingworth W. A systematic review of the magnitude and cause of geographic variation in unplanned hospital admission rates and length of stay for ambulatory care sensitive conditions. BMC Health Serv Res. 2015;15:324. | ||
National Health Security Office (NHSO). NHSO Annual Report Fiscal Year; 2017. Available from: https://www.nhso.go.th/frontend/page-about_result.aspx. Accessed July 22, 2018. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.