Back to Journals » Clinical Ophthalmology » Volume 17
Association of Treatment Duration and Clinical Outcomes in Dry Eye Treatment with Sutureless Cryopreserved Amniotic Membrane
Authors McDonald M, Janik SB, Bowden FW, Chokshi A, Singer MA, Tighe S, Mead OG , Nanda S, Qazi MA , Dierker D , Shupe AT, McMurren BJ
Received 16 June 2023
Accepted for publication 22 August 2023
Published 12 September 2023 Volume 2023:17 Pages 2697—2703
DOI https://doi.org/10.2147/OPTH.S423040
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Marguerite McDonald,1 Susan B Janik,2 Frank W Bowden,3 Amit Chokshi,4 Michael A Singer,5 Sean Tighe,6,7 Olivia G Mead,6 Seema Nanda,8 Mujtaba A Qazi,9 Damon Dierker,10 Adam T Shupe,11 Brittany J McMurren12
1Ophthalmic Consultants of Long Island, Lynbrook, NY, USA; 2Solinsky Eye Care, Kensington, CT, USA; 3Bowden Eye & Associates, Jacksonville, FL, USA; 4Florida Eye Specialists, Jacksonville, FL, USA; 5Medical Center Ophthalmology Associates, San Antonio, TX, USA; 6BioTissue Holdings, Inc, Miami, FL, USA; 7Florida International University Herbert Wertheim College of Medicine, Miami, FL, USA; 8Nanda Dry Eye & Vision Institute, Houston, TX, USA; 9Pepose Vision Institute, Chesterfield, MO, USA; 10Eye Surgeons of Indiana, Indianapolis, IN, USA; 11Royo Eye Care, Marysville, CA, USA; 12Werner Optometry, San Diego, CA, USA
Correspondence: Sean Tighe, 7300 Corporate Center Drive, Suite 700, Miami, FL, 33126, USA, Email [email protected]
Background: While sutureless, cryopreserved amniotic membrane (cAM) has been shown to significantly improve signs and symptoms of dry eye disease (DED), no studies have assessed the association of cAM treatment duration to the differential response in clinical outcomes.
Methods: A multi-center, retrospective study was conducted on patients with moderate-to-severe DED who were treated with self-retained cAM (Prokera® Slim) for 2 to 7 days. The primary outcome measure was DEWS severity score assessed at 1 week, 1 month, and 3 months. Secondary outcome measures included ocular discomfort, visual symptoms, corneal staining, and visual acuity.
Results: A total of 89 eyes (77 patients) with moderate-to-severe DED (DEWS severity 3.24 ± 0.56) received treatment with self-retained cAM for 2 days (n = 10), 3 days (n = 15), 4 days (n = 12), 5 days (n = 19), 6 days (n = 6), or 7 days (n = 27). DEWS scores significantly improved at 1 week, 1 month, and 3 months for all treatment duration groups, with no significant difference observed between groups at any timepoint. In addition to an improvement in DEWS severity scores, those receiving cAM treatment for 2 days demonstrated a significant improvement in corneal staining, visual symptoms, and ocular discomfort at 1 week, 1 month, and 3 months.
Conclusion: This retrospective study suggests that a single placement of self-retained cAM for 2 days can significantly improve signs and symptoms of DED with a lasting benefit observed for up to 3 months.
Keywords: amniotic membrane, cryopreserved, dry eye, ocular surface, Prokera
Introduction
Dry eye disease (DED) is a multifactorial disease affecting an estimated 16 million people in the United States.1 First-line therapies include artificial tears and topical anti-inflammatories, including corticosteroids, cyclosporine, and lifitegrast. Other common therapies include punctal occlusion for individuals with aqueous tear deficiency and warm compresses and lid hygiene for those with meibomian gland dysfunction.2 However, these treatments may fail to alleviate signs and symptoms in those with more severe forms of dry eye, necessitating the use of alternative therapies. One such treatment includes sutureless, self-retained cryopreserved amniotic membrane (cAM), which has been regarded as a standard of care for the treatment of many ocular surface diseases in the United States. Sutureless cAM covers and protects the corneal surface while promoting corneal healing through its anti-inflammatory and anti-scarring properties that support epithelial adhesion and differentiation.3,4 When used in patients with severe DED, cAM has been shown to significantly improve the ocular surface health and symptoms for up to 6 months.5–9 In one prospective, randomized study, treatment with cAM for 3–5 days resulted in a significant improvement in dry eye severity score, corneal staining, tear break-up time, and corneal nerve density in DED patients at 1 and 3 months, whereas control subjects receiving conventional maximum treatment showed no significant change.6 Aside from the anti-inflammatory benefits, the lasting effect of a single placement of cAM was also attributed to the regeneration of the corneal nerves, which play a vital role in epithelial regeneration and tear film stability through reflex tearing and blinking.6
Despite the therapeutic benefits of sutureless cAM, foreign body sensation is observed in some patients and may temporarily blur vision, while it is historically placed over the ocular surface for 5–7 days in patients.8,10 While a number of studies have demonstrated a significant improvement in signs and symptoms of DED after treatment with cAM for an average of 5 days,5–9 it remains unclear if placing the device on the ocular surface for a shorter period of time may improve patients’ experience while still providing similar clinical benefits. Thus, the purpose of this study was to assess the therapeutic benefit of sutureless cAM in DED patients across various treatment durations and to determine whether a shorter treatment duration of two days provides similar clinical outcomes with a lasting benefit.
Methods
This multi-center, retrospective study evaluated the effectiveness of self-retained cAM in reducing signs and symptoms of DED by treatment duration across ten clinical sites. We have previously reported on this data cohort as a whole.5 The study was exempted under 45 CFR §46.101(b)(4) by the Western Institutional Review Board (Puyallup, WA, USA) and was conducted in accordance with the tenets of the Declaration of Helsinki. Patients were included in the study if they were 18 years or older, had been diagnosed with moderate-to-severe DED as defined by the Report of the International Dry Eye WorkShop (DEWS 2–4),11 and were subsequently treated with self-retained cryopreserved AM (Prokera® Slim, Bio-Tissue, Miami, FL, USA) for 2 to 7 days. Only patients who had completed 1 week, 1 month and 3 months of follow-up were included for analysis. Exclusion criteria included symblepharon, ocular surgery or injury within 3 months, contact lens use, and those who had trigeminal nerve damage or had undergone previous brain surgery. Data collection was limited to information existing in the electronic medical records and included patient demographics, comorbidities, prior and concomitant dry eye treatments, chief complaints (ocular pain, discomfort, photophobia, blurry vision, redness), duration of cAM treatment, and complications.
Treatment
Cryopreserved AM was thawed at room temperature for several minutes and rinsed with saline solution prior to insertion with topical anesthesia (0.5% proparacaine hydrochloride eye drops). The device was placed into the superior fornix while the patient looked down and was then slid under the lower eyelid. Patients returned to the office after 2 to 7 days for removal of the device.
Outcomes
Outcomes were assessed at 1 week, 1 month, and 3 months post-treatment. The primary outcome measure was the DEWS severity score, which was based on the overall assessment of clinical signs and symptoms and graded using a 4-tier scale as previously described.11 Secondary outcome measures included ocular discomfort, visual symptoms, corneal staining, and visual acuity (VA). Severity and frequency of both ocular discomfort and visual symptoms were graded from level 1 (none or mild and/or episodic) to level 4 (severe and/or disabling and constant). Corneal staining was graded by severity and location as (1) none to mild, (2) variable, (3) marked central, or (4) severe punctate erosions.
Statistical Analysis
All statistical analyses were carried out using SPSS Software version 20.0 (IBM; Armonk, NY, USA). Continuous outcomes were reported as mean ± standard deviation (range), and categorical data were reported as frequency (percentage). Ordinal variables, such as DEWS severity and corneal staining, were compared between baseline and follow-up using the Wilcoxon Signed Rank test. Continuous variables, such as VA, were assessed between two timepoints using the paired samples t-test or between three timepoints using a one-way ANOVA. Kendall’s tau-b coefficient (τb) was used to assess correlations between two non-parametric data samples. A P value < 0.05 was considered statistically significant.
Results
A total of 89 eyes of 77 patients (63 females, 14 males) with moderate-to-severe DED met the eligibility criteria and were included for analysis. The mean age at the time of treatment was 68.9 ± 10.8 years (range: 43–89), and comorbidities included cataract (37.1%), glaucoma (23.6%), lagophthalmos (7.9%), and macular degeneration (4.5%). Upon examination, patients presented with moderate-to-severe DED (DEWS severity 3.24 ± 0.56) despite treatment with artificial tears (86.5%), cyclosporine (51.7%), corticosteroids (40.4%), punctal occlusion (32.6%), antibiotics (25.8%), autologous serum (7.9%), and NSAIDs (4.5%). More specifically, 30.3% of eyes presented with DEWS grade 4, 62.9% of eyes were DEWS grade 3, and 6.7% of eyes were DEWS grade 2. The majority of patients presented with ocular discomfort (85.4%) and blurred vision (59.6%), with other chief complaints including pain (37.1%), redness (32.6%), and photophobia (12.4%). Baseline characteristics, including age, DEWS scores, logMAR VA, chief complaints, and number of prior treatments, did not significantly differ between treatment duration groups (p > 0.05).
Self-retained cAM was placed for an average of 4.9 ± 1.8 days. Specifically, cAM was placed for 2 days in 10 eyes, 3 days in 15 eyes, 4 days in 12 eyes, 5 days in 19 eyes, 6 days in 6 eyes, and 7 days in 27 eyes. Patients continued use of ocular treatment therapies, and tape-tarsorrhaphy was implemented following cAM placement in 24 (27%) eyes. Upon removal of the device, the cAM was intact in 30.3% of eyes, partially dissolved in 19.1% of eyes, completely dissolved in 39.3% of eyes, and not noted in 11.2% of eyes. Extent of cAM dissolution was significantly correlated with the duration of placement on the ocular surface (τb = 0.395, p < 0.001). A total of 8 eyes (10.1%) necessitated additional treatment, which was significantly correlated with the presence of lagophthalmos (τb = 0.32, p = 0.003). Re-treatment was not significantly correlated with treatment duration (p = 0.21).
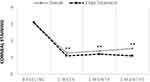
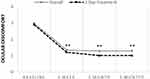
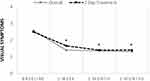
Following cAM treatment, DEWS severity significantly improved from 3.24 ± 0.56 at baseline to 1.45 ± 0.65 at 1 week, 1.45 ± 0.65 at 1 month, and 1.47 ± 0.63 at 3 months (Table 1, p < 0.0001). This was accompanied by a significant improvement in overall corneal staining scores (Figure 1), ocular discomfort scores (Figure 2), and visual symptom scores (Figure 3) at all follow-up visits (p < 0.0001). Furthermore, VA significantly improved from logMAR 0.30 at baseline to logMAR 0.22 at 1 and 3 months (p = 0.001), corresponding to an average increase in VA by 0.9 Snellen lines. No complications or adverse events attributed to self-retained cAM were observed.
 |
Table 1 DEWS Scores by Treatment Duration with Cryopreserved Amniotic Membrane (cAM) |
DEWS severity scores by cAM treatment duration are presented in Table 1. DEWS scores significantly improved at 1 week, 1 month, and 3 months with all treatment durations, with no significant difference observed between groups at any timepoint (Table 1). When assessing only those who received cAM treatment for 2 days, DEWS severity scores significantly improved from 3.1 ± 0.6 at baseline to 1.5 ± 0.5 at 1 week (p = 0.006) and 1.2 ± 0.4 at both 1 and 3 months (p = 0.004, Table 1, Figure 4). This was accompanied by a significant improvement in corneal staining (Figure 1), ocular discomfort (Figure 2), and visual symptoms (Figure 3) at 1 week, 1 month, and 3 months, with no significant differences observed at any timepoint when compared to the entire study sample (Figures 1–3). Specifically, corneal staining scores significantly improved from 3.1 ± 0.6 at baseline to 1.1 ± 0.3, 1.2 ± 0.6, and 1.1 ± 0.3 at 1 week (p = 0.004), 1 month (p = 0.006), and 3 months (p = 0.004), respectively (Figure 1). Furthermore, ocular discomfort significantly improved from 2.9 ± 0.7 at baseline to 1.2 ± 0.4, 1.0 ± 0.0, and 1.0 ± 0.0 at 1 week, 1 month, and 3 months post-treatment, respectively (p = 0.004, Figure 2). Visual symptoms significantly improved from 2.5 ± 1.0 at baseline to 1.7 ± 0.9, 1.4 ± 0.5, and 1.4 ± 0.7 at 1 week (p = 0.04), 1 month (p = 0.02), and 3 months (p = 0.02), respectively (Figure 3). Only one case (10%) who received cAM treatment for 2 days required re-treatment.
Discussion
DED is a multifactorial disorder of the ocular surface characterized by tear film instability and inflammation that compromises both corneal epithelial and corneal nerve health, resulting in ocular surface breakdown and a self-perpetuating cycle of inflammation.12 While many conventional treatments aim to address signs and symptoms of DED by reducing inflammation, some of these therapies may require persistent application and up to 3 months of treatment to obtain a clinical benefit.13,14 Furthermore, many of these treatments may not effectively restore the corneal nerves, which are often compromised in patients with DED15 and play a vital role in maintaining corneal epithelial health,16–18 thus limiting their durability of clinical response. For example, lifitegrast, which is a commonly used treatment for DED, has been shown to be effective in reducing symptoms of ocular dryness and improving inferior corneal staining after 3 months of continued treatment but does not significantly improve corneal sensitivity.13,14 Additionally, although artificial tears may provide some benefit,19,20 one study has shown no significant improvement in sign or symptoms of patients with low corneal sub-basal nerve fiber length.21 On the contrary, cAM targets both innate and adaptive immune responses through a multi-modal approach,22–26 the former of which is achieved by promoting apoptosis of activated pro-inflammatory neutrophils and macrophages, polarization of macrophages from the M1 to the M2 phenotype and increasing macrophage phagocytosis of apoptotic neutrophils.22–25 Moreover, such an anti-inflammatory effect extends to adaptive immune responses by suppressing the activation of Th1 and Th17 lymphocytes and promoting the expansion of Treg cells, which ultimately suppresses CD4+ T cell activation and downregulates alloreactive immune responses.23,26 These anti-inflammatory actions ultimately promote corneal epithelialization27 and corneal nerve regeneration6 in patients with ocular surface disease following treatment for as little as 5 days. A randomized, controlled trial demonstrated that a single placement of sutureless cAM for 3 to 5 days resulted in a significant improvement in both signs and symptoms of DED as well as a significant increase in corneal nerve density and sensitivity at 3 months compared to those receiving conventional treatment.6 Thus, cAM may be beneficial in patients with moderate-to-severe DED who have failed other conventional treatment options, as it can improve both corneal epithelial and corneal nerve health.
While sutureless cAM has been shown to improve the signs and symptoms of moderate-to-severe DED for up to 6 months following treatment for an average of 5 days,5–9 no prior studies have assessed whether the clinical benefit of cAM is retained following a shorter treatment duration. In this retrospective study, we found that treatment with cAM for only 2 days achieved similar significantly improved signs and symptoms in patients with moderate-to-severe DED as early as 1-week post-treatment, with a significant benefit observed up to 3 months. Notably, when assessing outcomes by treatment duration, all groups demonstrated a significant and similar improvement in DED severity, suggesting that a similar benefit can be obtained following treatment for as little as 2 days. These findings are notable as a shorter treatment duration may mitigate discomfort from the polycarbonate ring as well as reduce the duration of potential visual impairment due to the cAM’s semi-translucent nature, which may ultimately improve patient quality of life. Due to the study’s retrospective design, prospective, randomized studies are warranted to verify the study findings and confirm that improvement in signs and symptoms of DED is similar regardless of cAM treatment duration, and a significant improvement in outcomes can be achieved with only 2 days of treatment. Furthermore, future studies should include patient satisfaction as an outcome measure to determine whether shorter treatment duration is associated with higher patient satisfaction.
Conclusion
This retrospective study suggests that self-retained cAM significantly improves signs and symptoms of DED regardless of treatment duration, with a shorter treatment duration of two days resulting in significant clinical improvement and a lasting benefit for up to 3 months.
Acknowledgment
Material is under consideration for presentation for the American Academy of Ophthalmology Annual Meeting, 2023, in San Francisco, CA.
Funding
No financial support. The development of Prokera® was supported in part with grant number EY014768 from the National Institutes of Health (NIH) and National Eye Institute (NEI). The content is solely the responsibility of the authors and does not necessarily represent the opinion of the NIH or the NEI.
Disclosure
Dr Sean Tighe and Mrs Olivia Mead are employees of BioTissue Holdings Inc. Dr Marguerite McDonald reports personal fees from BioTissue, during the conduct of the study. Dr Susan Janik reports a research grant from BioTissue for prior work, and Physician Recommended Nutriceuticals--Advisory Board outside the submitted work. Dr Frank W Bowden reports speaker fees from Sun and B+L, advisor board from Sightsciences, outside the submitted work. Dr Seema Nanda reports personal fees from Nanda Dry Eye & Vision Institute, during the conduct of the study; personal fees from Nanda Dry Eye & Vision Institute, outside the submitted work. Dr Damon Dierker reports personal fees from Bio-Tissue, during the conduct of the study; personal fees from Alcon, Allergan, Bausch & Lomb, Dompe, Novartis, Oyster Point Pharma, Sun Pharma, outside the submitted work. The authors report no other conflicts of interest in this work.
References
1. Farrand KF, Fridman M, Stillman I, Schaumberg DA. Prevalence of diagnosed dry eye disease in the United States among adults aged 18 years and older. Am J Ophthalmol. 2017;182:90–98. doi:10.1016/j.ajo.2017.06.033
2. Sabeti S, Kheirkhah A, Yin J, Dana R. Management of meibomian gland dysfunction: a review. Surv Ophthalmol. 2020;65:205–217. doi:10.1016/j.survophthal.2019.08.007
3. Mead OG, Tighe S, Tseng SCG. Amniotic membrane transplantation for managing dry eye and neurotrophic keratitis. Taiwan J Ophthalmol. 2020;10:13–21. doi:10.4103/tjo.tjo_5_20
4. Tighe S, Mead OG, Lee A, Tseng SCG. Basic science review of birth tissue uses in ophthalmology. Taiwan J Ophthalmol. 2020;10:3–12. doi:10.4103/tjo.tjo_4_20
5. McDonald MB, Sheha H, Tighe S, et al. Treatment outcomes in the DRy Eye Amniotic Membrane (DREAM) study. Clin Ophthalmol. 2018;9:677–681. doi:10.2147/OPTH.S162203
6. John T, Tighe S, Sheha H, et al. Corneal nerve regeneration after self-retained cryopreserved amniotic membrane in dry eye disease. J Ophthalmol. 2017;2017:10. doi:10.1155/2017/6404918
7. Cheng AM, Zhao D, Chen R, et al. Accelerated restoration of ocular surface health in dry eye disease by self-retained cryopreserved amniotic membrane. Ocul Surf. 2016;14:56–63. doi:10.1016/j.jtos.2015.07.003
8. Sheppard J, Yeu E, Tseng S. Sutureless Cryopreserved Amniotic Membrane Transplantation Accelerates Ocular Surface Healing and Topographic Stabilization for Dry Eye Patients. NJ, USA: Wiley-Blackwell; 2015.
9. Vendal Z. Management of glaucoma medication induced dry eye disease with self-retained cryopreserved amniotic membrane. J Dry Eye Dis. 2022;5:e28–e34. doi:10.22374/jded.v5i1.41
10. Suri K, Kosker M, Raber IM, et al. Sutureless amniotic membrane ProKera for ocular surface disorders: short-term results. Eye Contact Lens. 2013;39:341–347. doi:10.1097/ICL.0b013e3182a2f8fa
11. Lemp MA, Foulks GN. The definition and classification of dry eye disease: report of the definition and classification subcommittee of the international dry eye workshop. Ocul Surf. 2007;5:75–92. doi:10.1016/S1542-0124(12)70081-2
12. Stevenson W, Chauhan SK, Dana R. Dry eye disease: an immune-mediated ocular surface disorder. Arch Ophthalmol. 2012;130:90–100. doi:10.1001/archophthalmol.2011.364
13. Holland EJ, Luchs J, Karpecki PM, et al. Lifitegrast for the treatment of dry eye disease: results of a Phase III, randomized, double-masked, placebo-controlled trial (OPUS-3). Ophthalmology. 2017;124:53–60. doi:10.1016/j.ophtha.2016.09.025
14. Sheppard JD, Torkildsen GL, Lonsdale JD, et al. Lifitegrast ophthalmic solution 5.0% for treatment of dry eye disease: results of the OPUS-1 Phase 3 study. Ophthalmology. 2014;121:475–483. doi:10.1016/j.ophtha.2013.09.015
15. Tepelus TC, Chiu GB, Huang J, et al. Correlation between corneal innervation and inflammation evaluated with confocal microscopy and symptomatology in patients with dry eye syndromes: a preliminary study. Graefes Arch Clin Exp Ophthalmol. 2017;255:1771–1778. doi:10.1007/s00417-017-3680-3
16. Okada Y, Sumioka T, Ichikawa K, et al. Sensory nerve supports epithelial stem cell function in healing of corneal epithelium in mice: the role of trigeminal nerve transient receptor potential vanilloid 4. Lab Invest. 2019;99:210–230. doi:10.1038/s41374-018-0118-4
17. Shi X, Wang L, Clark JD, Kingery WS. Keratinocytes express cytokines and nerve growth factor in response to neuropeptide activation of the ERK1/2 and JNK MAPK transcription pathways. Regul Pept. 2013;186:92–103. doi:10.1016/j.regpep.2013.08.001
18. Yang L, Di G, Qi X, et al. Substance P promotes diabetic corneal epithelial wound healing through molecular mechanisms mediated via the neurokinin-1 receptor. Diabetes. 2014;63:4262–4274. doi:10.2337/db14-0163
19. Arif FAC, Hilmi MR, Kamal KM. A prospective contralateral eye comparison of the tolerability of two artificial tears with different physical properties in patients with dry eye disease. Med Hypothesis Discov Innov. 2023;4:1–6. doi:10.51329/mehdioptometry167
20. Che Arif F, Hilmi MR, Kamal K, Ithnin M. Comparison of immediate effects on usage of dual polymer artificial tears on changes in tear film characteristics. IIUM Med J Malays. 2020;2020:18.
21. Kheirkhah A, Dohlman TH, Amparo F, et al. Effects of corneal nerve density on the response to treatment in dry eye disease. Ophthalmology. 2015;122:662–668. doi:10.1016/j.ophtha.2014.11.006
22. He H, Li W, Tseng DY, et al. Biochemical characterization and function of complexes formed by hyaluronan and the heavy chains of inter-alpha-inhibitor (HC*HA) purified from extracts of human amniotic membrane. J Biol Chem. 2009;284:20136–20146. doi:10.1074/jbc.M109.021881
23. He H, Tan Y, Duffort S, Perez VL, Tseng SC. In vivo downregulation of innate and adaptive immune responses in corneal allograft rejection by HC-HA/PTX3 complex purified from amniotic membrane. Invest Ophthalmol Vis Sci. 2014;55:1647–1656. doi:10.1167/iovs.13-13094
24. He H, Li W, Chen SY, et al. Suppression of activation and induction of apoptosis in RAW264.7 cells by amniotic membrane extract. Invest Ophthalmol Vis Sci. 2008;49:4468–4475. doi:10.1167/iovs.08-1781
25. He H, Zhang S, Tighe S, Son J, Tseng SC. Immobilized heavy chain-hyaluronic acid polarizes lipopolysaccharide-activated macrophages toward M2 phenotype. J Biol Chem. 2013;288:25792–25803. doi:10.1074/jbc.M113.479584
26. He H, Kuriyan AE, C-W S, et al. Inhibition of proliferation and epithelial mesenchymal transition in retinal pigment epithelial cells by heavy chain-hyaluronan/pentraxin 3. Sci Rep. 2017;7:43736. doi:10.1038/srep43736
27. Tighe S, Moein H-R, Chua L, Cheng A, Hamrah P, Tseng SCG. Topical cryopreserved amniotic membrane and umbilical cord eye drops promote re-epithelialization in a murine corneal abrasion ModelAMUC for promoting re-epithelialization. Invest Ophthalmol Vis Sci. 2017;58:1586–1593. doi:10.1167/iovs.16-20834
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.