Back to Journals » Clinical Ophthalmology » Volume 18
Association Between Peripheral Retinal Defocus and Myopia by Multispectral Refraction Topography in Chinese Children
Authors Bao T, Qin L, Hou G, Jiang H, Wang L, Wang Y, Wu J, Wang J, Pang Y
Received 16 November 2023
Accepted for publication 14 February 2024
Published 20 February 2024 Volume 2024:18 Pages 517—523
DOI https://doi.org/10.2147/OPTH.S450224
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Tong Bao,1,* Liru Qin,2,* Guimei Hou,1 Hongmei Jiang,1 Lifeng Wang,1 Ying Wang,1 Junhui Wu,1 Jinli Wang,3 Yunlei Pang4
1Department of Ophthalmological Examination, Chifeng Chaoju Eye Hospital, Chifeng, People’s Republic of China; 2Department of Ophthalmology, Inner Mongolia Baogang Hospital, Baotou, People’s Republic of China; 3Department of Cataract, Chifeng Chaoju Eye Hospital, Chifeng, People’s Republic of China; 4Department of Ophthalmic Plastic Surgery, Chifeng Chaoju Eye Hospital, Chifeng, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Jinli Wang, Department of Cataract, Chifeng Chaoju Eye Hospital, Chifeng, People’s Republic of China, Email [email protected] Yunlei Pang, Department of Ophthalmic Plastic Surgery, Chifeng Chaoju Eye Hospital, Chifeng, People’s Republic of China, Email [email protected]
Objective: To investigate the association between the peripheral refractive errors of the fundus in different regions and moderate and high myopia.
Methods: In this case-control study, 320 children and adolescents aged 6 to 18 years were recruited. Peripheral refractive errors were measured using multispectral retinal refractive topography (MRT). Spherical equivalent (SE) and cylinder errors were classified into low, moderate, and high categories based on the magnitude range. Logistic regression was performed to test the factors associated with myopia.
Results: There were 152 participants with low myopia and 168 participants with moderate and high myopia included in the current study. Participants with moderate and high myopia were most likely to be older, with larger axial length (AL), lower SE, less time to watch electronic devices on the weekend, a higher difference between central refractive error and paracentral refractive error from the superior side of the retina (RDV-S), but a smaller difference between the central refractive error and paracentral refractive error from the inferior side of the retina (RDV-I) than those with low myopia (all P < 0.05). After logistic analysis, female sex (odds ratio [OR] = 4.14; 95% confidence interval [CI] = 2.16– 7.97, P < 0.001), AL (OR = 6.88, 95% CI = 4.33– 10.93, P < 0.001), and RDV-I (OR = 0.52, 95% CI = 0.32– 0.86, P = 0.010) were independent factors for moderate and high myopia.
Conclusion: Our study demonstrated that the retina peripheral refraction of the eyes (RDV-I) was associated with moderate and high myopia, and RDV-S was only associated with high myopia.
Keywords: peripheral refractive errors, myopia, spherical equivalent, logistic analysis, ocular biometrics
Introduction
Myopia is one of the most common refractive errors, and its incidence increases annually; thus, it has become an important public issue worldwide.1 Globally, it is estimated that the number of people suffering from myopia is approximately1.45 billion, with the highest prevalence rate in Asia.2,3 The mechanism of myopia development is still unclear; however, current evidence indicates that peripheral retinal refractive status may be related to occurrence of myopia.4–6 More outdoor activities may reduce the process of myopia due to modifying retinal refractive status.7,8 The peripheral retina of emmetropia is associated with a mild relative myopic refractive state, while the peripheral retina of uncorrected hyperopia is closely related to a slightly higher relative myopic refractive status.9
After light enters the eye, the central image can be focused on the retina, but the peripheral focus is located before and after the retina. When the object is focused on the retina, it will promote the growth of the eye axis, leading to myopia. Multispectral refraction topography (MRT) uses single spectra to respond to light of a special wavelength to sequentially collect fundus images.8 Using a deep development computer algorithm (ie, a series of neural network-based U-Nets), the multispectral images after lens compensation were compared and analyzed, and the corresponding terrain map was drawn after calculating and summarizing the actual refractive values of each pixel. This method can be used to predict the occurrence and development of myopia in advance, and to scientifically evaluate the effectiveness of various forms of myopia prevention and control. To date, many previous studies have investigated the association between MRT measurements and myopia; however, those studies did not adjust variables such as body mass index, or lifestyle factors.10–13 Therefore, this study aimed to investigate the association between peripheral retinal defocus measurements and myopia.
Methods
Study Design and Subjects
In this cross-sectional observational study, we collected information on 320 patients with myopia who were seen at Chifeng Chaoju Eye Hospital between January and June 2023. Ethical approval was obtained from the Ethics Committee of the Chifeng Chaoju Eye Hospital. Written informed consent was obtained from the child’s parents or guardian.
Eye Examination and Questionnaire
Patients with spherical equivalent (SE) errors in both eyes of at least −0.5 diopters (D) seen in the ophthalmology outpatient department of Chifeng Chaoju Eye Hospital between June 1 and September 30, 2023 were eligible for the current study. The inclusion criteria were as follows: (1) between the ages of 6 and 18 years, and (2) best-corrected visual acuity (BCVA) of 20/20 in both eyes. The exclusion criteria were as follows: (1) any ocular diseases or previous ocular surgery history, (2) a history of corneal contact lenses or atropine eye drops, and (3) a history of any severe systemic disease. The study included only the right eye.
All children and adolescents underwent a questionnaire and comprehensive eye examination. Demographic information, family history, and lifestyle factors such as time to look at electronic devices and time spent outdoors were collected. The time was categorized as low (<2 hours), normal (2–4 hours) and high (>4 hours). Body weight and height were measured and BMI was calculated using the formula:  . Refractive examination was performed using an autorefractometer (AR-360A, NIDEK Co. Ltd., Japan) after full cycloplegia, using mixed eye drops containing 0.5% tropicamide and 0.5% phenylephrine (SINQI Pharmaceutical Co., Ltd., Shenyang, China) for mydriasis, every 10 minutes, followed by 3 drops and observation for 10 minutes. Photometry was performed in a semi-dark room environment. This examination was completed by an experienced optometrist. Refractive error value was presented as sphere (S) and cylinder (C) measurements. The final refractive error was recorded as the spherical equivalent (SE), and the SE value (D) was SE = S + C/2. The intraocular pressure (IOP) was measured using a non-contact tonometer NT-4000 (Nidek Co. Ltd., Gamagori, Japan). The axial length (AL) was measured by IOL Master Biometry (Master 2000, Zeiss Co., Germany). The mean of three measurements was collected as the final result. Retinal defocus measurements were tested using multispectral refraction topography (version 1.0.5T05C; Thondar, Inc.). The parameters were defined as follows: peripheral refractive errors (RPRE); peripheral refractive error from center to peripheral 53°of retina (TRDV) and four regions − RDV-Superior (RDV-S), RDV-Inferior (RDV-I), RDV-Temporal (RDV-T), and RDV-Nasal (RDV-N) − from the fovea to 53 degrees (RDV-15, RDV-30, RDV-45) (Figure 1).
. Refractive examination was performed using an autorefractometer (AR-360A, NIDEK Co. Ltd., Japan) after full cycloplegia, using mixed eye drops containing 0.5% tropicamide and 0.5% phenylephrine (SINQI Pharmaceutical Co., Ltd., Shenyang, China) for mydriasis, every 10 minutes, followed by 3 drops and observation for 10 minutes. Photometry was performed in a semi-dark room environment. This examination was completed by an experienced optometrist. Refractive error value was presented as sphere (S) and cylinder (C) measurements. The final refractive error was recorded as the spherical equivalent (SE), and the SE value (D) was SE = S + C/2. The intraocular pressure (IOP) was measured using a non-contact tonometer NT-4000 (Nidek Co. Ltd., Gamagori, Japan). The axial length (AL) was measured by IOL Master Biometry (Master 2000, Zeiss Co., Germany). The mean of three measurements was collected as the final result. Retinal defocus measurements were tested using multispectral refraction topography (version 1.0.5T05C; Thondar, Inc.). The parameters were defined as follows: peripheral refractive errors (RPRE); peripheral refractive error from center to peripheral 53°of retina (TRDV) and four regions − RDV-Superior (RDV-S), RDV-Inferior (RDV-I), RDV-Temporal (RDV-T), and RDV-Nasal (RDV-N) − from the fovea to 53 degrees (RDV-15, RDV-30, RDV-45) (Figure 1).
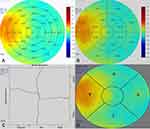 |
Figure 1 Multispectral refractive topography. (A) Mean-R; (B) Relative-R; (C) Profile; (D) Quadrant. |
Myopia Definition and Category
Participants were classified into two refractive groups according to central SE refractive error: low myopia was defined as an SE of 0 to −2.99 D, moderate myopia as an SE of −3D and −6, and high myopia as an SE of > −6D. In this study, we combined both moderate and high myopia into one group.
Statistical Analysis
All statistical analysis was performed using SPSS 26.0 (SPSS Inc., Chicago, IL, USA). Data were presented as mean ± standard deviation (SD) for continuous measures and analyzed by the independent sample t-test. On the other hand, categorical measurements were presented as percentages and compared using Pearson chi-square test. Logistic regression analysis was used to analyze the relationship between biomedical ocular information, demographic information, lifestyle indicators, and myopia. Statistical significance was interpreted as a P-value of less than 0.05.
Results
Currently, 320 children and adolescents (320 eyes) involving 161 boys and 159 girls aged 6 to 18 years were included. Of which, 152 had low myopia (mean SE: −1.75 ± 1.0 D), and 168 had moderate to high myopia (mean SE: −4.25 ± 1.94 D). Compared with low myopia, participants with moderate and high myopia were most likely to be older, with larger AL, lower SE, less time to watch electronic devices on the weekend, higher RDV-S but lower RDV-I than those with low myopia (all P <0.05; Table 1).
 |
Table 1 Demographic and Ocular Characteristics of the Two Refractive Groups |
In the multivariate analysis using logistic regression, female sex (OR = 4.14; 95% CI = 2.16–7.97, P <0.001), AL (OR = 6.88, 95% CI = 4.33–10.93, P <0.001), and RDV-I (OR = 0.52, 95% CI = 0.32–0.86, P = 0.010) was significantly correlated with moderate and high myopia (Table 2).
 |
Table 2 Risk Factors Associated with Moderate to High Myopia |
In subgroup analysis, female sex (OR = 3.62, 95% CI = 1.86–7.04, P <0.001) and AL (OR = 5.35, 95% CI = 3.37–8.49, P <0.001) were associated with moderate myopia. Furthermore, female sex (OR = 4.64, 95% CI = 1.81–11.87, P <0.001), age (OR = 1.31, 95% CI = 1.05–1.61, P = 0.015), AL (OR = 18.29, 95% CI = 9.34–35.83, P <0.001), and RDV-S (OR = 2.71, 95% CI = 1.34–5.49, P = 0.006) were associated with high myopia (Table 3).
 |
Table 3 Risk Factors Associated with Moderate and High Myopia |
Discussion
With the development of socio-economic improvements, myopia among children and adolescents has gradually become the focus of public health measures. Early screening and mechanisms of investigation are important. MRT is new equipment using multispectral imaging technology. This instrument collects ocular fundus images, and parameters are calculated by a novel computer algorithm according to subtle differences in fundus images of different wavelengths. MRT can reveal the refractive status of some points of the retina within 53 degrees by successively collecting fundus images with different wavelengths of a single spectral light, which has been reported elsewhere.14 However, the association between its parameters and moderate and high myopia has not been fully verified and affirmed in clinical practice.
In the current study, it is noteworthy that participants had higher RDV-S but lower RDV-I than those with low myopia. Furthermore, female sex, AL, and RDV-I were significantly correlated with moderate and high myopia. Generally, compared with low myopia, participants with a higher difference between central refractive error and paracentral refractive error from the inferior side of the retina had a 0.52 times higher risk for moderate and high myopia; while participants with a higher difference between central refractive error and paracentral refractive error from the superior side of the retina had a 2.71 times higher risk for high myopia. Recently, another relative sample size study indicated that children had a myopia defocus within 15° eccentricity.10 Moreover, the retina defocus of the fovea area has less influence on the occurrence of myopia. Generally, hyperopia defocus at 30° and 45° eccentricity of fundus is observed among children with high myopia, while children with low and moderate myopia present hyperopia at 45° eccentricity. In view of the peripheral refractive errors, the hyperopic shift was larger in eyes with moderate myopia than in those with low myopia.6
Peripheral defocus refers to the myopia degree state of the peripheral retina; the optics of the eyeball and the curve of the retina both contribute to the peripheral refraction of the retina.15 Defocus of the peripheral retina has benefits in controlling the growth in axial length, which may be associated with reducing changes in choroidal thickness.16 A previous study indicated that the defocused signals around the retina occupy a dominant position in the process of growth in axial length.17 Generally, both the central and peripheral retina provide visual signals to the retina, thereby directly influencing refractive development and ocular growth. It can be inferred that differences in the distribution and sensitivity of visual neurons from the central and peripheral retina may be important factors in the different responses of the retina to peripheral defocus in different regions, with different impacts on growth of the eyeball. Herein, understanding the association between central and peripheral retinal defocus may have key implications for the control of myopia.
Furthermore, children with peripheral hyperopia defocus experience it two years before the development of myopia, which indicates that peripheral hyperopia defocus may appear in emmetropia.18 Unfortunately, there is no emmetropia included in the current study; thus, we cannot investigate the association between peripheral hyperopia defocus and low myopia, or even its predictive significance for the occurrence of myopia.
In the four quadrants, we found that RDV-I in our study was associated with moderate and high myopia. Moreover, the higher was the degree of myopia, the larger was its significance. Another study evaluated the peripheral refractive errors in horizontal and vertical positions, and two diagonal meridians, and suggested that the hyperopic shift was larger toward the inferior visual field than toward the superior visual field in the moderate and high myopia groups.19 In contrast, Gregor F. Schmid and co-researchers indicated that the steepening of the relative peripheral eye length varied significantly in the superior retina.20 The exact mechanism of the role of peripheral refractive error in myopic occurrence remains unclear. On the one hand, peripheral hyperopic defocus is associated with axial elongation during myopia development. On the other hand, peripheral hyperopia may be a result of eye growth. Further studies are warranted to explore the specific mechanism between peripheral hyperopic defocus and myopia.
In our study, we found that myopes with more diopters used digital devices for fewer hours on the weekend. This may be due to them spending more time studying on weekends, so although they spend less time watching electronic devices, they have a higher degree of myopia. Another scenario is that because this study is cross-sectional, those with high myopia were asked to reduce their electronic devise usage time on weekends. These are all our speculations, and further investigation is needed to confirm them.
A strength of the current study is the association between MRT indicators and myopia adjusted with more variables. There are several limitations in our study too, however. First, the findings are limited by the small sample size and the case-control design. Herein, further prospective studies with a larger sample size are needed to confirm the present findings. Second, we only included participants with myopia and no subjects with emmetropia; therefore, our findings should be interpolated with some caution.
Conclusion
In summary, our findings suggest that the RDV in the inferior retina is associated with both moderate and high myopia, and RDV in the superior side of retina is only associated with high myopia. Consequently, the study concluded that peripheral hyperopic defocus components may be identified as a factor related to myopia.
Data Sharing Statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethical Approval
The study was performed in accordance with the Helsinki Declaration of 1964 and its later amendments and approved by the Ethics Committee of Chifeng Chaoju Eye Hospital. All participants were aware of the collection of their data for this study and informed consent was obtained from each participant.
Acknowledgments
We thank the participants of the study.
Disclosure
All authors declare that they have no competing interests in this work.
References
1. Liu L, Jiao J, Yang X, et al. Global, regional, and national burdens of blindness and vision loss in children and adolescents from 1990 to 2019: a trend analysis. Ophthalmology. 2023;130(6):575–587. doi:10.1016/j.ophtha.2023.02.002
2. Wen G, Tarczy-Hornoch K, McKean-Cowdin R, et al. Prevalence of myopia, hyperopia, and astigmatism in non-Hispanic white and Asian children: multi-ethnic pediatric eye disease study. Ophthalmology. 2013;120(10):2109–2116. doi:10.1016/j.ophtha.2013.06.039
3. Yusufu M, Bukhari J, Yu X, et al. Challenges in eye care in the Asia-Pacific Region. Asia Pac J Ophthalmol. 2021;10(5):423–429. doi:10.1097/APO.0000000000000391
4. Smith EL, Hung L-F, Huang J. Relative peripheral hyperopic defocus alters central refractive development in infant monkeys. Vision Res. 2009;49(19):2386–2392. doi:10.1016/j.visres.2009.07.011
5. Seidemann A, Schaeffel F, Guirao A, et al. Peripheral refractive errors in myopic, emmetropic, and hyperopic young subjects. J Opt Soc Am a Opt Image Sci Vis. 2002;19(12):2363–2373. doi:10.1364/JOSAA.19.002363
6. Chen X, Sankaridurg P, Donovan L, et al. Characteristics of peripheral refractive errors of myopic and non-myopic Chinese eyes. Vision Res. 2010;50(1):31–35. doi:10.1016/j.visres.2009.10.004
7. Karthikeyan SK, Ashwini DL, Priyanka M, et al. Physical activity, time spent outdoors, and near work in relation to myopia prevalence, incidence, and progression: an overview of systematic reviews and meta-analyses. Indian J Ophthalmol. 2022;70(3):728–739. doi:10.4103/ijo.IJO_1564_21
8. Muralidharan AR, Lança C, Biswas S, et al. Light and myopia: from epidemiological studies to neurobiological mechanisms. Ther Adv Ophthalmol. 2021;13:25158414211059246. doi:10.1177/25158414211059246
9. Atchison DA, Pritchard N, White SD, Griffiths AM. Influence of age on peripheral refraction. Vision Res. 2005;45(6):715–720. doi:10.1016/j.visres.2004.09.028
10. Zhao Q, Du X, Yang Y, et al. Quantitative analysis of peripheral retinal defocus checked by multispectral refraction topography in myopia among youth. Chin Med J. 2023;136(4):476–478. doi:10.1097/CM9.0000000000002606
11. Xiaoli L, Xiangyue Z, Lihua L, et al. Comparative study of relative peripheral refraction in children with different degrees of myopia. Front Med. 2022;9:800653. doi:10.3389/fmed.2022.800653
12. Zheng X, Cheng D, Lu X, et al. Relationship between peripheral refraction in different retinal regions and myopia development of Young Chinese People. Front Med. 2021;8:802706. doi:10.3389/fmed.2021.802706
13. N-J N, F-Y M, X-M W, et al. Novel application of multispectral refraction topography in the observation of myopic control effect by orthokeratology lens in adolescents. World J Clin Cases. 2021;9(30):8985–8998. doi:10.12998/wjcc.v9.i30.8985
14. Liao YR, Yang ZL, Li ZJ, et al. A quantitative comparison of multispectral refraction topography and autorefractometer in young adults. Front Med. 2021;8:715640. doi:10.3389/fmed.2021.715640
15. Verkicharla PK, Mathur A, Mallen EA, et al. Eye shape and retinal shape, and their relation to peripheral refraction. Ophthalmic Physiol Opt. 2012;32(3):184–199. doi:10.1111/j.1475-1313.2012.00906.x
16. Huang YY, Wang YL, Shen Y, et al. Defocus-induced spatial changes in choroidal thickness of chicks observed by wide-field swept-source OCT. Exp Eye Res. 2023;233:109564. doi:10.1016/j.exer.2023.109564
17. Benavente-Pérez A, Nour A, Troilo D. Axial eye growth and refractive error development can be modified by exposing the peripheral retina to relative myopic or hyperopic defocus. Invest Ophthalmol Vis Sci. 2014;55(10):6765–6773. doi:10.1167/iovs.14-14524
18. Mutti DO, Hayes JR, Mitchell GL, et al. Refractive error, axial length, and relative peripheral refractive error before and after the onset of myopia. Invest Ophthalmol Vis Sci. 2007;48(6):2510–2519. doi:10.1167/iovs.06-0562
19. Shen J, Spors F, Egan D, et al. Peripheral refraction and image blur in four meridians in emmetropes and myopes. Clin Ophthalmol. 2018;12:345–358. doi:10.2147/OPTH.S151288
20. Schmid GF. Association between retinal steepness and central myopic shift in children. Optom Vis Sci. 2011;88(6):684–690. doi:10.1097/OPX.0b013e3182152646
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
