Back to Journals » Clinical Interventions in Aging » Volume 17
Association Between Low Serum Phosphate Level and Risk of Falls in Hospitalized Patients Over 50 Years of Age: A Retrospective Observational Cohort Study
Authors Jang SA , Kwon SJ , Kim CS, Park SW, Kim KM
Received 29 March 2022
Accepted for publication 1 August 2022
Published 8 September 2022 Volume 2022:17 Pages 1343—1351
DOI https://doi.org/10.2147/CIA.S368404
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Maddalena Illario
Seol A Jang,* Su Jin Kwon,* Chul Sik Kim, Seok Won Park, Kyoung Min Kim
Division of Endocrinology, Department of Internal Medicine, Yongin Severance Hospital, Yonsei University College of Medicine, Yongin, South Korea
*These authors contributed equally to this work
Correspondence: Kyoung Min Kim, Division of Endocrinology, Department of Internal Medicine, Yongin Severance Hospital, Yonsei University College of Medicine, Yongin, South Korea, Tel +82 31-5189-8798, Fax +82 31-5189-8567, Email [email protected]
Purpose: Falls are the leading cause of injury among hospitalized patients, particularly among older patients. We investigated the association between serum phosphate (s-phosphate) levels and the risk of in-hospital falls.
Patients and Methods: This retrospective observational cohort study included all patients aged over 50 years who were admitted to Yongin Severance Hospital in South Korea between January 2018 and March 2021. Demographic, anthropometric, and biochemical parameters were recorded on admission. S-phosphate levels were classified into three groups: below normal (< 2.8 mg/dL), normal (2.8– 4.4 mg/dL), and above normal (≥ 4.5 mg/dL). The normal group was further stratified into tertiles (2.8– 3.2, 3.3– 3.7, and 3.8– 4.4 mg/dL). The incidence of in-hospital falls was compared between the five groups. Logistic regression analyses were performed to assess the association between s-phosphate levels and the incidence of falls during the hospital stay, with clinical factors included as covariates in the multivariable models.
Results: A total of 15,485 patients (female: 52.1%) with a median age of 70.0 years (interquartile range: 60.0– 79.0 years) were included in the analysis, of whom 295 (1.9%) experienced a fall during the hospital stay. The incidence of falls was significantly higher among patients with lower s-phosphate levels, and this relationship also applied among patients with s-phosphate levels within the normal range as well. The association between lower s-phosphate levels and increased risk of falls remained significant in the adjusted analyses.
Conclusion: A lower s-phosphate level on admission was independently associated with an increased risk of in-hospital falls. Further studies are needed to determine whether the s-phosphate level on admission could improve prediction of the risk of in-hospital falls.
Keywords: in-hospital falls, older adults, blood biochemistry, risk prediction
Introduction
Falls are one of the most common health-related adverse events, occurring in more than one-third of persons aged 65 years and older each year.1–4 In addition, 10–20% of falls result in serious injury, hospitalization, or death.5 Despite awareness on the clinical importance of falls among older adults and efforts to prevent falls, the incidence of falls continues to increase in aging societies.6,7
Falls are associated with increased morbidity and mortality, immobility, decreased quality of life, functional dependency, admission to long-term care facilities, and increased medical costs.8,9 Falls among hospitalized patients may necessitate unplanned medical procedures and treatment and lead to longer hospital stays owing to the increased incidence of hospitalization-related complications. Furthermore, the increased medical cost is a burden for both patients and medical institutions.10 Therefore, the incidence of in-hospital falls is an important indicator that is used to evaluate the quality of hospital care.
Several strategies, such as multifactorial assessment and intervention programs, have been proposed for reducing the risk of falls among older patients and some strategies are effective at reducing the incidence and severity of falls.11–14 Identifying older persons who are at an increased risk of falls is a critical first step for preventing falls.6 Previous studies have identified several clinical factors that influence the risk of falls among patients, including history of falls, recent weight loss, muscle weakness, and urinary difficulties.15,16 However, most of these parameters are evaluated based on patient responses to questions or on the need for additional measures; thus, the availability and accuracy of data on such measures are limited.17,18 Therefore, more accessible and intuitive risk measures are needed in the clinical setting for assessing the risk of falls, especially among older patients.
In the review of the literature, abnormalities of phosphate handling and phosphate levels were common in older people and were clinically important in some cases.19 As well as in specific diseases or conditions, it was reported that serum phosphate (s-phosphate) levels were associated with in-hospital mortality in general hospitalized patients.20 The level of s-phosphate is one of the most commonly assessed serum measures in hospitalized patients. Abnormal s-phosphate levels are common, with a prevalence up to 45% in hospitalized patients.21,22 Several studies have suggested that phosphates play a role in musculoskeletal health.23–25 However, to the best of our knowledge, the association between s-phosphate levels and the risk of falls has not been studied previously. If the level of s-phosphate is associated with the risk of falls among hospitalized patients, it could be used as a readily available objective measure to assess the risk of falls among hospitalized patients. Therefore, we investigated the association between the s-phosphate level on admission and the risk of falls among hospitalized patients using data from hospital electronic health records (EHRs).
Material and Methods
Study Design and Participants
We conducted a single-center, retrospective cohort study of patients admitted to Yongin Severance Hospital between January 2018 and March 2021. Patients who did not have data on s-phosphate levels or who were aged under 50 years on admission were excluded. If a patient was hospitalized more than once, only the first hospitalization was included in the analysis. The study was conducted in compliance with the principles of the Declaration of Helsinki. The protocol was approved by the Institutional Review Board of Yongin Severance Hospital (IRB number: 9–2021-0037). The requirement for informed consent was waived because of the retrospective nature of the study.
Demographic Data and Anthropometric and Biochemical Measurements
Demographics data were collected on admission, including personal characteristics (age and sex) and history of falls in the past 6 months. Patients’ height and weight were measured in light clothing and without shoes to the nearest 0.1 cm and 0.1 kg, respectively. Body mass index (BMI) was calculated by determining the ratio of weight to the square of height (expressed in kg/m2). For biochemical analyses, blood samples were collected from patients at the time of admission and the s-phosphate (mg/dL), calcium (mg/dL), alkaline phosphatase (ALP) (IU/L), glucose (mg/dL), blood urea nitrogen (BUN) (mg/dL), creatinine (mg/dL), and uric acid (mg/dL) levels were assessed. If there were multiple measurements, we included the first set of measurements during hospitalization.
Fall Incidence
The occurrence of falls during hospitalization was the primary outcome. A fall was defined as “inadvertently coming to rest on the ground, floor, or other lower level, excluding intentional change in position to rest in furniture, wall or other objects.”26
Fall Risk Score
The fall risk score was calculated on admission for all hospitalized patients using the Johns Hopkins Fall Risk Assessment Tool.27 This tool consists of seven indicators: age, history of falls, bowel and urinary incontinence, medications, patient care equipment (such as IV infusion, chest tube, indwelling catheter), mobility, and cognition. A score of 6–13 is associated with a moderate risk of falls, and a score of ≥14 is associated with a high risk of falls.
Statistical Analyses
The s-phosphate level was first stratified as below normal (BN, <2.8 mg/dL), normal (2.8–4.4 mg/dL), and above normal (AN, ≥4.5 mg/dL), and s-phosphate levels within the normal range were further divided into tertiles. Then, all analyses were performed using these five groups (BN: <2.8 mg/dL; tertile 1 [T1]: 2.8–3.2 mg/dL; tertile 2 [T2]: 3.3–3.7 mg/dL; tertile 3 [T3]: 3.8–4.4 mg/dL; AN: ≥4.5 mg/dL). We performed two sets of analyses, including and excluding patients with extremely high s-phosphate levels (>6.0 mg/dL) to exclude patients with secondary hyperphosphatemia. However, the results did not differ. Therefore, the primary analyses were carried out excluding patients with s-phosphate levels >6.0 mg/dL. Continuous variables were tested for conformity to the normal distribution using skewness, kurtosis, and quantile–quantile (Q-Q) plots. Baseline clinical characteristics were compared between the five groups using one-way analysis of variance or Pearson’s chi-square test. Continuous variables are reported as the median and interquartile range (IQR), and categorical variables are reported as frequencies and percentages. Associations between s-phosphate levels and other clinical and laboratory variables were tested using Spearman correlation coefficient. Variables that correlated with s-phosphate levels were included as covariates in the multivariable models (Supplementary Figure 1). The incidence rate of falls in each phosphate group was compared using a linear test. Logistic regression analyses were performed to test for associations between s-phosphate levels and the risk of falls using the AN group as the reference group. Unadjusted analyses and four different adjusted models were used: Model I adjusted for age. Model II adjusted for age, creatinine, BUN, and uric acid. Model III adjusted for age, creatinine, BUN, uric acid, height, weight, BMI, systolic blood pressure (SBP), diastolic blood pressure (DBP), pulse, cholesterol, ALP, alanine aminotransferase (ALT), bilirubin, protein, albumin, hematocrit, and red cell distribution width, and the fall risk score. Model IV adjusted for age, creatinine, BUN, uric acid, height, weight, BMI, SBP, DBP, pulse, cholesterol, ALP, ALT, bilirubin, protein, albumin, hematocrit, and red cell distribution width, and fall history. All analyses were done using R statistics (version 4.0.5). Two-sided p-values ≤0.05 indicated statistical significance.
Results
Baseline Characteristics of Study Participants
A total of 15,485 patients were included in the analyses. The baseline characteristics of study participants are shown in Table 1. The median (IQR) age was 70.0 (60.0–79.0) years, and 52.1% were women. The median (IQR) hospital stay was 5.0 (2.0–9.0) days, and 33.3% of participants were admitted to the surgical department for minor or major operations. Among all study participants, 691 (4.5%) had a history of a fall within the previous 6 months.
 |
Table 1 Baseline Characteristics of Study Population |
Clinical and Biochemical Parameters According to s-Phosphate Levels
The s-phosphate level was skewed toward higher values with a median (IQR) value of 3.5 (3.0–3.9) mg/dL (Supplementary Figure 2).
The clinical and biochemical measures in each phosphate group are summarized in Table 1. The s-phosphate levels were lower in older patients (p < 0.001). The SBP, pulse rate, and ALP level were higher and the cholesterol level was lower among patients with lower s-phosphate levels (all ptrend < 0.001). In contrast, higher s-phosphate levels were associated with higher BUN, creatinine, and uric acid levels (all ptrend < 0.001). Patients with higher phosphate levels were more likely to have a history of falls (ptrend = 0.029). The fall risk score on admission did not differ significantly according to the s-phosphate level (ptrend = 0.381). The baseline clinical characteristics including those of participants with s-phosphate levels >6.0 mg/dL are shown in Supplementary Table 1. The results were similar to the results of participants with s-phosphate levels >6.0 mg/dL excluded.
Association Between s-Phosphate Level and Risk of Falls
Of the 15,485 participants, 295 (1.9%) experienced a fall during their hospital stay. The incidence of falls was significantly higher among patients with a lower s-phosphate level (Figure 1). The trend toward a higher incidence of falls with lower s-phosphate levels was observed even among patients with s-phosphate levels within the normal range (BN group, 2.2%; T1 group, 2.3%; T2 group, 1.9%; T3 group, 1.7%; AN group, 1.1%).
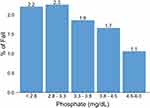 |
Figure 1 Incidence of falls during hospitalization according to the serum phosphate level on admission. |
In the unadjusted logistic regression analysis, the risk of falls in the BN and T1 groups was more than double that of the AN group (odds ratio [OR], 95% confidence interval [CI]: 2.1, 1.2–4.0; and 2.2, 1.2–4.1, respectively) (Table 2). In the age-adjusted model, the risk of falls was inversely related to the s-phosphate level (Model I in Table 2). After adjusting for age, creatinine, BUN, uric acid, height, weight, BMI, SBP, DBP, pulse, cholesterol, ALP, ALT, bilirubin, protein, albumin, hematocrit, and red cell distribution width and fall risk score in the BN group was more than three-fold times higher than that in the AN group: OR, 95% CI: 3.3, 1.5–8.5 (Model III in Table 2). Further adjustment for history of fall did not change the results (Model IV in Table 2).
 |
Table 2 Association Between Serum Phosphate Level and Fall Risk |
Discussion
In this study, a lower s-phosphate level was associated with a significantly higher risk of falls among hospitalized patients over 50 years of age. The risk of falls was inversely related to the s-phosphate level on admission, even among patients with s-phosphate levels within the normal range. This association was consistent after further adjustment for other clinical risk factors for falls, including a history of falls and the high fall risk assessment score. To our knowledge, this is the first study to report a significant association between s-phosphate levels and the risk of falls among hospitalized patients.
Despite the medical importance of falls among older patients, only few readily applicable models for predicting falls are available.28 A risk algorithm has been proposed for predicting falls, but its predictive ability is relatively low.28,29 Although previous studies have identified various risk factors, the risk factors identified generally have disadvantages because they require additional measurements or are difficult to measure in frail patients and patients with acute disease.30,31 Therefore, further studies are needed to identify easily applicable fall-related risk factors. In this study, s-phosphate, a marker that is widely measured among hospitalized patients, was shown to have a significant association with the risk of falling.
In this study, lower levels of s-phosphate were associated with a higher risk of falls during the hospital stay. The underlying mechanism through which lower phosphate levels are associated with an increased risk of falls is unclear. Some previous studies have shown that phosphate may play a role in muscle biology. Animal and human studies suggest that either phosphorus depletion or hypophosphatemia has an adverse effect on muscle function and composition.32 Hypophosphatemia causes severe muscle weakness in many organisms, including humans,33,34 dogs,32 and rodents.35 Pesta et al36 found that both the s-phosphate level and muscle ATP synthetic flux were 50% lower in a patient with hereditary hypophosphatemic rickets with hypercalciuria than in healthy controls but were completely normalized after oral phosphate supplementation. These results suggest that phosphate plays an important role in muscle function. An animal study in dog conducted by Fuller et al32 found that moderate phosphorus depletion can induce reversible changes in skeletal muscle composition and transmembrane potential.
In addition, a few recent clinical studies suggest an association between s-phosphate levels and sarcopenia or frailty in older patients. A study by Veilleux et al23 found abnormalities in muscle density and muscle function in patients with hypophosphatemic rickets (HPR). Compared with age-matched and sex-matched controls, patients with HPR had similar muscle size (p = 0.58) but lower muscle density (p = 0.008) and lower peak muscle force and power (both p = 0.001). However, the biologic mechanistic study wherein the s-phosphate level is associated with the risk of falls requires further research. In addition, studies should be conducted to evaluate whether phosphate supplementation to increase the s-phosphate level can reduce the risk of falls.
This study has some limitations. First, this was an observational retrospective study that used routinely available data; therefore, parameters not routinely measured (phosphate-regulating hormones, such as serum vitamin D, parathyroid hormone, and fibroblast growth factor-23) were not included in the analysis. Second, owing to the heterogeneity of the EHR data, the use of drugs or underlying comorbidities that might affect the level of s-phosphate were not included in the analysis. However, this study also has several strengths. It had a relatively large sample size and multiple laboratory measures were included as covariates in the multivariable logistic regression analyses. Furthermore, all hospitalized patients were evaluated for fall risk on admission using one of the most commonly used fall risk assessment tools, in addition to being questioned about their history of falls.
Conclusions
A lower level of s-phosphate on admission was associated with a significantly higher risk of falls among hospitalized patients over 50 years of age. Patients with low s-phosphate levels on admission should be carefully monitored for fall risk to prevent falls. Further studies are warranted to assess the effect of monitoring and interventions to increase the s-phosphate level on the risk of in-hospital falls in patients with low s-phosphate levels.
Ethics Approval and Informed Consent
The protocol was approved by the Institutional Review Board of Yongin Severance Hospital (IRB number: 9-2021-0037). The requirement for informed consent was waived because of the retrospective nature of the study.
Author Contributions
All authors made a significant contribution to the work reported, in one or more of the following areas: KMK conception of the study. SAJ, SJK and KMK acquisition and analysis of the data, SAJ, SJK, CSK, SWP and KMK interpretation of the results. SAJ and KMK drafting the manuscript. All authors critically reviewing the manuscript. All authors gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This research was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education (2021R1I1A1A01060333). The funder had no role in the creation of the research question, design of the study, data collection, analysis, interpretation, or the writing of this manuscript.
Disclosure
The authors report no conflicts of interest in this work.
References
1. World Health Organization. Falls: fact sheet; 2018:25.
2. Deandrea S, Lucenteforte E, Bravi F, Foschi R, La Vecchia C, Negri E. Risk factors for falls in community-dwelling older people: “a systematic review and meta-analysis”. Epidemiology. 2010;21:658–668. doi:10.1097/EDE.0b013e3181e89905
3. Gosney M, Harper A, Conroy S. Oxford Desk Reference: Geriatric Medicine. OUP Oxford; 2012.
4. Tinetti ME. Where is the vision for fall prevention? J Am Geriatr Soc. 2001;49(5):676–677. doi:10.1046/j.1532-5415.2001.49132.x
5. Rubenstein LZ. Falls in older people: epidemiology, risk factors and strategies for prevention. Age Ageing. 2006;35(suppl_2):ii37–ii41. doi:10.1093/ageing/afl084
6. Najafpour Z, Godarzi Z, Arab M, Yaseri M. Risk factors for falls in hospital in-patients: a prospective nested case control study. Int J Health Policy Manag. 2019;8(5):300. doi:10.15171/ijhpm.2019.11
7. Pérez-Ros P, Martinez-Arnau FM, Malafarina V, Tarazona-Santabalbina FJ. A one-year proprioceptive exercise programme reduces the incidence of falls in community-dwelling elderly people: a before–after non-randomised intervention study. Maturitas. 2016;94:155–160. doi:10.1016/j.maturitas.2016.09.007
8. Terroso M, Rosa N, Torres Marques A, Simoes R. Physical consequences of falls in the elderly: a literature review from 1995 to 2010. Eur Rev Aging Phys Act. 2014;11(1):51–59. doi:10.1007/s11556-013-0134-8
9. Gelbard R, Inaba K, Okoye OT, et al. Falls in the elderly: a modern look at an old problem. Am J Surg. 2014;208(2):249–253. doi:10.1016/j.amjsurg.2013.12.034
10. Boyé ND, Van Lieshout EM, Van Beeck EF, Hartholt KA, der Cammen TJ V, Patka P. The impact of falls in the elderly. Trauma. 2013;15(1):29–35. doi:10.1177/1460408612463145
11. Gillespie LD, Robertson MC, Gillespie WJ, et al. Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2012;2012(9):1.
12. Balzer K, Bremer M, Schramm S, Lühmann D, Raspe H. Falls prevention for the elderly. GMS Health Technol Assess. 2012;8. doi:10.3205/hta000099
13. Tricco AC, Thomas SM, Veroniki AA, et al. Comparisons of interventions for preventing falls in older adults: a systematic review and meta-analysis. JAMA. 2017;318(17):1687–1699. doi:10.1001/jama.2017.15006
14. Sherrington C, Michaleff ZA, Fairhall N, et al. Exercise to prevent falls in older adults: an updated systematic review and meta-analysis. Br J Sports Med. 2017;51(24):1750–1758. doi:10.1136/bjsports-2016-096547
15. Ambrose AF, Paul G, Hausdorff JM. Risk factors for falls among older adults: a review of the literature. Maturitas. 2013;75(1):51–61. doi:10.1016/j.maturitas.2013.02.009
16. Gale CR, Cooper C, Aihie Sayer A. Prevalence and risk factors for falls in older men and women: the English longitudinal study of ageing. Age Ageing. 2016;45(6):789–794. doi:10.1093/ageing/afw129
17. Van Schooten KS, Pijnappels M, Rispens SM, Elders PJ, Lips P, van Dieën JH. Ambulatory fall-risk assessment: amount and quality of daily-life gait predict falls in older adults. J Gerontol a Biol Sci. 2015;70(5):608–615. doi:10.1093/gerona/glu225
18. Callis N. Falls prevention: identification of predictive fall risk factors. Appl Nurs Res. 2016;29:53–58. doi:10.1016/j.apnr.2015.05.007
19. Lambert M, Witham M, Sumukadas D. Serum phosphate in older people. Rev Clin Gerontol. 2009;19(4):263–270. doi:10.1017/S0959259809990359
20. Cheungpasitporn W, Thongprayoon C, Mao MA, Kittanamongkolchai W, Sakhuja A, Erickson SB. Admission serum phosphate levels predict hospital mortality. Hosp Pract. 2018;46(3):121–127. doi:10.1080/21548331.2018.1483172
21. Haider DG, Lindner G, Wolzt M, et al. Hyperphosphatemia is an independent risk factor for mortality in critically ill patients: results from a cross-sectional study. PLoS One. 2015;10(8):e0133426. doi:10.1371/journal.pone.0133426
22. Hoffmann M, Zemlin A, Meyer W, Erasmus R. Hypophosphataemia at a large academic hospital in South Africa. J Clin Pathol. 2008;61(10):1104–1107. doi:10.1136/jcp.2007.054940
23. Veilleux L-N, Cheung M, Ben Amor M, Rauch F. Abnormalities in muscle density and muscle function in hypophosphatemic rickets. J Clin Endocrinol Metab. 2012;97(8):E1492–E1498. doi:10.1210/jc.2012-1336
24. Amanzadeh J, Reilly RF. Hypophosphatemia: an evidence-based approach to its clinical consequences and management. Nat Clin Pract Nephrol. 2006;2(3):136–148. doi:10.1038/ncpneph0124
25. Ravid M, Robson M. Proximal myopathy caused by latrogenic phosphate depletion. JAMA. 1976;236(12):1380–1381. doi:10.1001/jama.1976.03270130042026
26. World Health Organization, Ageing World Health Organization, Unit LC. WHO global report on falls prevention in older age: World Health Organization; 2008.
27. Poe SS, Dawson PB, Cvach M, et al. The Johns Hopkins fall risk assessment tool. J Nurs Care Qual. 2018;33(1):10–19. doi:10.1097/NCQ.0000000000000301
28. Park S-H. Tools for assessing fall risk in the elderly: a systematic review and meta-analysis. Aging Clin Exp Res. 2018;30(1):1–16. doi:10.1007/s40520-017-0749-0
29. Gade GV, Jørgensen MG, Ryg J, et al. Predicting falls in community-dwelling older adults: a systematic review of prognostic models. BMJ open. 2021;11(5):e044170. doi:10.1136/bmjopen-2020-044170
30. O’Connell B, Myers H. A failed fall prevention study in an acute care setting: lessons from the swamp. Int J Nurs Pract. 2001;7(2):126–130. doi:10.1046/j.1440-172X.2001.00300.x
31. Fhon JRS, Rosset I, Freitas CP, Silva AO, Santos JLF, Rodrigues RAP. Prevalence of falls among frail elderly adults. Rev Saude Publica. 2013;47:266–273. doi:10.1590/S0034-8910.2013047003468
32. Fuller TJ, Carter NW, Barcenas C, Knochel JP. Reversible changes of the muscle cell in experimental phosphorus deficiency. J Clin Invest. 1976;57(4):1019–1024. doi:10.1172/JCI108343
33. Geerse DA, Bindels AJ, Kuiper MA, Roos AN, Spronk PE, Schultz MJ. Treatment of hypophosphatemia in the intensive care unit: a review. Critic Care. 2010;14(4):1–8. doi:10.1186/cc9215
34. Soyoral Y, Aslan M, Ebinc S, Dirik Y, Demir C. Life-threatening hypophosphatemia and/or phosphate depletion in a patient with acute lymphoblastic leukemia: a rare case report. Am J Emerg Med. 2014;32(11):
35. Schubert L, DeLuca HF. Hypophosphatemia is responsible for skeletal muscle weakness of vitamin D deficiency. Arch Biochem Biophys. 2010;500(2):157–161. doi:10.1016/j.abb.2010.05.029
36. Pesta DH, Tsirigotis DN, Befroy DE, et al. Hypophosphatemia promotes lower rates of muscle ATP synthesis. FASEB J. 2016;30(10):3378–3387. doi:10.1096/fj.201600473R
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
