Back to Journals » Adolescent Health, Medicine and Therapeutics » Volume 11
Association Between Irritable Bowel Syndrome and Sleep Disturbance in Adolescents
Authors Indah Kusumawati Noor L , Bakri A, Soejadhi R, Kesuma Y
Received 7 February 2020
Accepted for publication 24 April 2020
Published 11 June 2020 Volume 2020:11 Pages 73—77
DOI https://doi.org/10.2147/AHMT.S248711
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Alastair Sutcliffe
Laili Indah Kusumawati Noor,1 Achirul Bakri,2 Rismarini Soejadhi,2 Yudianita Kesuma2
1Specialist Study Program, Department of Pediatrics, Faculty of Medicine, Universitas Sriwijaya and Moh Hoesin Hospital, Palembang, Indonesia; 2Department of Pediatrics, Faculty of Medicine, Universitas Sriwijaya and Moh Hoesin Hospital, Palembang, Indonesia
Correspondence: Yudianita Kesuma
Department of Pediatrics, Faculty of Medicine, Universitas Sriwijaya and Moh. Hoesin Hospital, Palembang, Indonesia
Tel/Fax +62 711 376445
Email [email protected]
Introduction: Sleep disorder in adolescents is a problem that is rarely considered by both parents and healthcare professionals. Ignorance of sleep disorders is likely caused by the very rare occurrence of associated sporadic or emergency cases. Irritable bowel syndrome (IBS) is a functional gastrointestinal disorder characterized by abdominal pain and changes in the defecation pattern. Previous research has demonstrated IBS as one of the many causes of sleep disorders. Difficulty sleeping, frequent awakening, and difficulty returning to sleep after awakening are the symptoms often experienced by adolescents with IBS. The high incidence of IBS in adolescents and the large proportion of sleep disorders in IBS affect the quality of life and disrupt physical development, behaviour, and learning achievement. The relationship between IBS and sleep disorders in adolescents needs to be studied. This study aims to determine the relationship between sleep disorders and IBS in high school adolescents in Palembang.
Methods: This is a cross-sectional study conducted on 294 high school adolescents in Palembang in June 2018. Random sampling method was used and the presence of IBS and sleep disturbances were assessed using a questionnaire.
Results: Among all subjects, we found 113 subjects (38.4%) with IBS. Of these 113 subjects with IBS, only 60 subjects (53.1%) experienced sleep disorders.
Conclusion: No correlation found between sleep disorders and IBS in adolescents.
Keywords: irritable bowel syndrome, IBS, sleep disorders, adolescents
Introduction
Adolescence is a transitional phase where children become adults, characterized by hormonal, physical, psychological, and social adaptive changes. This phase is important in shaping the characteristics of an adult human being as the nation’s future generation, and therefore requires special attention from parents, teachers, healthcare workers, and the community. Failure in providing guidance and direction for the processes that occur in this phase will affect the teenagers themselves, their families, and the community greatly.1 With advances in technology and industry, most teenagers begin to have additional activities that can make them experience sleep disorders. Sleep disorders can have serious effects in the long term, such as causing behavioural disorders and growth.2 The first large-scale comprehensive study on sleep disorders and its effects in adolescents showed that 13% of adolescents experience emotional disturbances related to sleep disorders.4 Other research had shown the negative impacts of sleep disorders in adolescents on physical development and behaviour, including growth disorders, cardiovascular disorders, cognitive function, and daily behaviour.3
Irritable bowel syndrome (IBS) is a functional gastrointestinal disorder characterized by abdominal pain and changes in the pattern of defecation. Research conducted in Turkey demonstrated IBS as one of the causes of sleep disorders. Difficulty sleeping, frequent awakening, and difficulty returning to sleep after awakening are the symptoms often experienced by adolescents with IBS. This study showed that 36% of IBS patients had poor sleep quality compared to controls, and other studies showed that 71% of IBS patients had depression, which would certainly worsen sleep quality.5 The high incidence of IBS in adolescents and the large proportion of sleep disorders in IBS negatively affect quality of life, and disrupt physical development, behaviour, learning achievement, and sleep.7 This study aims to identify the relationship between IBS and sleep disorders in adolescent high school students in Palembang.
Methods
This is a qualitative and quantitative analytical study with a cross-sectional design. Quantitative measurement was conducted using a questionnaire. Qualitative measurement was conducted through in-depth interview and direct observation of IBS symptoms using ROME III criteria. The population in this study were adolescents enrolled in a senior high school. A total of 294 senior high school students were recruited with simple random sampling.
Data were collected after obtaining written informed consent from the subjects, and written informed consent must have been provided by a parent or legal guardian of the participant. The study was in accordance with the Declaration of Helsinki. Subjects who fulfilled the Rome III criteria for IBS were asked to complete a questionnaire and attend an in-depth interview.
Two partial statistical tests were performed for analysis. First, independent variables were converted into a ratio. There are two distributions of data collected from 2 questionnaires representing the criteria: the sleep disturbance scale for children (SDSC) and ROME III IBS criteria. Second, the independent variables were converted into categorical data and a chi-square test was performed. Simultaneous analysis was conducted to see the effects of independent variables on the dependent variables together, and to identify which independent variable had the greatest influence on the dependent variables. Linear logistic regression was also performed in the analysis. The study protocol was approved by the Health Research Review Committee (Institutional Review Board) at Faculty of Medicine Sriwijaya University School of Medicine and Mohammad Hoesin Central General Hospital, Palembang, Indonesia, under protocol number 327/kepkrsmhfkunsri/2018, date 12 December 2018.
Results
Categorical variables are presented in Table 1. The subjects’ mean age was 15.61±0.9 years. The boy-to-girl ratio was 1:1.69. Most of the subjects were well-nourished (211 subjects, 71.8%) and 59.9% slept alone. Sixty-seven per cent of subjects had a habit of taking naps, and only 13.6% of subjects had a smoking habit. A total of 249 subjects (84.7%) in this study used their smartphone for more than 2 hours a day. Most of the subjects had no extracurricular activities (54.8%) and 13.9% of subjects worked at a part-time job after school hours.
 |
Table 1 Characteristics of Subjects |
The distribution of score interpretation from the ROME III and SCDC questionnaires is presented in Table 2. ROME III criteria are the standard criteria used to determine the presence or absence of IBS. In this study, 113 of 294 subjects (38.4%) were found to have experienced IBS symptoms. ROME III criteria can also be used to determine IBS subtypes. Out of 294 subjects, the most common subtype of IBS was constipation, comprising 13.9% of the total sample, followed by unclassified IBS (9.5%), diarrhoea (6.5%), and mixed (8.5%).
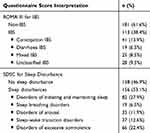 |
Table 2 Distribution of IBS ROME III and SDSC Questionnaire Score Interpretation (n=294) |
Table 3 presents the result of bivariate analysis on the risk factors for sleep disorders. In this study, there was no significant association between sleep disturbances and IBS but the use of a smartphone/screen contact and not having extracurricular activities were found to be associated with sleep disorders. This study also found that subjects who used a smartphone for >2 hours had a 0.350 times risk for experiencing sleep disturbances compared to subjects who used a smartphone for ≤2 hours (P=0.000; OR=0.350). We also found a lack of extracurricular activities to be related to sleep disorders (P=0.004; OR=0.456). In other words, students who do not partake in extracurricular activities have 0.456 times the risk for experiencing sleep disorders compared to those who partake in extracurricular activities.
 |
Table 3 Bivariate Analysis on Risk Factors for Sleep Disturbances |
Logistic regression analysis shows that IBS occurrence was associated with roommate status and napping habit. The following mathematical formula can be used to predict the probability of IBS by applying the formula  ; for example, suppose there is a teenager who had a napping habit (score=1 if does not have napping habit) and roommate status (score 0 if does not have a roommate), hence the probability he/she got IBS:
; for example, suppose there is a teenager who had a napping habit (score=1 if does not have napping habit) and roommate status (score 0 if does not have a roommate), hence the probability he/she got IBS:
YIBS = −4.82 + 1.6*roommate status + 2.6 * taking nap = −4.82, then 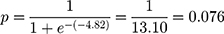 or 7.6%
or 7.6%
As given by that calculation, the probability that a teenager got IBS when he had a roommate and a napping habit was 7%.
Discussion
Our finding is in contrast with demographic research conducted on high school students in Bandung, which showed no significant difference between male and female students. Eighty-three students (28.2%) were malnourished, and this number is smaller compared to that found in research conducted by Padriyani et al on high school students in the Padang, where they found that 50.4% of high school students were malnourished.9
A study by Hyams et al identified IBS in 117 of 227 (51.54%) children and adolescents.9 Soares et al found a prevalence of 32.2% for IBS using ROME III criteria. Previous studies have identified several factors associated with the incidence of IBS in adolescents, including history of abuse, type of food, and diet.10,11
Of the 294 subjects, 156 students (53.1%) had sleep disorders. There were 82 subjects (27.9%) who had difficulties in falling asleep and maintaining the sleeping state, 66 subjects (22.4%) experienced excessive somnolence disorder, 35 subjects (11.9%) experienced impaired consciousness, and 38 subjects (12.9%) experienced a sleep–wake transition disorder. However, no subject experienced sleep hyperhidrosis.
In their study, Keefer et al found that between 11 and 27 IBS patients experienced sleep quality impairment, 3 to 29 IBS patients had difficulty falling asleep, about 11 to 25 IBS patients had reduced sleep duration, around 3 to 17 IBS patients experienced sleep transition disorders, and around 12 to 28 patients experienced sleep disruptions.8 Natalita’s study found 40 subjects (62.5%) suffering from sleep disturbances using the SDSC questionnaire, with the most frequent type being sleep–wake disorder (25%). Based on the examination performed in this study, there were 42 subjects (65.6%) who suffered from sleep disorders using the SDSC questionnaire, with 71.4% sensitivity and 54.5% specificity.12
Although other variables were found to have no significant relationship with sleep disturbances, we found that female students have a 1.010 times risk for experiencing sleep disturbances compared to male students, similar from study by Heitkemper, et al.6 Students who are at risk of malnutrition have a 0.876 times risk for experiencing sleep disorders and students who sleep alone have a 1.376 times risk for experiencing sleep disorders. Students who often take a nap have a 1.269 times risk for having sleep disturbances at night, students who smoke have a 0.720 times risk for experiencing sleep disturbances, and students who have part-time jobs have a 0.940 times risk for experiencing sleep disorders.
In this study, only 60 subjects (53%) experienced sleep disorders and IBS while 53 subjects (46.9%) did not have sleep disorders but experienced IBS. A study by Nachmiaz et al found that 21 of 41 patients (54%) experienced sleep disorders and irritable bowel diseases (IBD).16 Another study by Young et al found that 53.6% of patients experienced sleep disorders and IBD.14
This study found no significant relationship between IBS and sleep disorders. This might be due to the fact that the subjects in this study had sub-clinical complaints of IBS. The findings of this study are in line with that of Szigethy et al's study which found no significant association between IBS and sleep disorders.15
Zimmerman’s study found that IBS was more likely to have extraintestinal symptoms but did not have a significant relationship with sleep disorders. In his study, patients who had IBS with predominant symptoms of abdominal pain due to constipation were significantly associated with sleep disorders (p<0.001). It is important to note that IBS differs with IBD. Seventy per cent of patients diagnosed with IBD complain of abdominal pain accompanied by diarrhoea, constipation, and musculoskeletal disorders. This leads to the finding that IBD with diarrhoea and neurasthenia have a significant relationship with sleep disorders (p<0.025). Zimmerman concluded that sleep disorders in adolescents can be caused by a variety of risk factors, one of which is IBS, but it is not necessarily the main cause of sleep disorders in adolescents.17
The results of multivariate analysis showed that sleep disturbances in children are strongly associated with the use of a smartphone and lack of extracurricular activity. Students who use a smartphone for more than 2 hours a day have a 3.15 times increased risk for sleep disorder and students who take extracurricular activities have a 2.33 times increased risk for experiencing sleep disorders. Based on the results of probability calculations performed in this study, subjects who partake in extracurricular activities and use a smartphone ≤2 hours a day had a 1.1% probability of experiencing sleep disorders, while subjects who do not partake in extracurricular activities and use a smartphone >2 hours a day had a 7.5% probability of experiencing sleep disorders.
Conclusion
In this study, no significant relationship was found between sleep disorders and the incidence of IBS in high school adolescents.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Marcel A. Adolescent, growth, development, and behavior. In: Nelson Textbook of Pediatrics. Vol. 12.
2. Natalita C, Sekartini R, Poesponegoro H. The Sleep Disturbance for Children (SDSC) as a screening sleep diorders in junior high school student. Sari Pediatri. 2011;12:365–372. doi:10.14238/sp12.6.2011.365-72
3. Owens J, Opipari L, Nobile C, Spirito A. Sleep and daytime behavior in children with obstructive sleep apnea and behavioral sleep disorders. Pediatrics. 1998;102:1178–1184. doi:10.1542/peds.102.5.1178
4. Tanjung MC, Sekartini R. Sleep disturbance in children . Sari Pediatri. 2016;6(3):138–142. doi:10.14238/sp6.3.2004.138-42
5. Jochebed SR, Priya AJ. Common sleep disorders in adolescents-A survey. J Pharm Sci Res. 2015;7:381.
6. Heitkemper M, Jarrett M, Burr R, et al. Subjective and objective sleep indices in women with irritable bowel syndrome. Neurogastroenterol Motil. 2005;17:523–530. doi:10.1111/j.1365-2982.2005.00700.x
7. Canavan C, West J, Card T. The epidemiology of irritable bowel syndrome. Dove Press J. 2014;6:71–80.
8. Padriyani SO, Sulastri D, Syah NA. Association between nutritional status with academic performances among senior high school term 2013/2014 in Padang. Hubungan status gizi dengan prestasi belajar pada siswa SMA Negeri 1 Padang tahun ajaran 2013/2014. Jurnal Kesehatan Andalas. 2014;3:471–474. doi:10.25077/jka.v3i3.180
9. Baniasadi N, Dehesh MM, Mohebbi E, Hayatbakhsh AM, Oghabian Z. Assessing the sleep quality and depression-anxiety-stress in irritable bowel syndrome patients. Arq Gastroenterol. 2017;54:163–166. doi:10.1590/s0004-2803.201700000-08
10. Hyams JS, Burke G, Davis PM, et al. Characterization of symptoms in children with recurrent abdominal pain: resemblance to irritable bowel syndrome. J Pediatr Gastroenterol Nutr. 1995;20(2):209–214. doi:10.1097/00005176-199502000-00012
11. Kesuma Y. Hubungan masalah perilaku pada remaja dengan irritable bowel syndrome. Sari Pediatri. 2017;18:492–497. doi:10.14238/sp18.6.2017.492-7
12. Soares RL. Irritable bowel syndrome: a clinical review. World J Gastroenterol. 2014;20(34):121–144. doi:10.3748/wjg.v20.i34.12144
13. Keefer L, Stepanski EJ, Ranjbaran Z, et al. An initial report of sleep disturbance in inactive inflammatory bowel disease. J Clin Sleep Med. 2006;2(4):409–416. doi:10.5664/jcsm.26656
14. Young T, Peppard PE, Gottlieb DJ. Epidemiology of obstructive sleep apnea: a population health perspective. Am J Respir Crit Care Med. 2002;165:1217–1239. doi:10.1164/rccm.2109080
15. Szigethy E, Craig AE, Lobst EA, et al. Profile of depression in adolescents with inflammatory bowel disease: implications for treatment. Inflamm Bowel Dis. 2009;15(1):69–74. doi:10.1002/ibd.20693
16. Nachmias V, Sheinberg A, Weiss B, Fradkin A, Bujanover Y. Sleep disturbances among young patients with IBD in Israel. J Pediatr Gastroenterol Nutr. 2006;43:S48. doi:10.1097/01.mpg.0000256257.53363.40
17. Zimmerman J. Extraintestinal symptoms in irritable bowel syndrome and inflammatory bowel diseases: nature, severity, and relationship to gastrointestinal symptoms. Dig Dis Sci. 2003;48:743–749. doi:10.1023/A:1022840910283
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
