Back to Journals » Diabetes, Metabolic Syndrome and Obesity » Volume 16
Association Between Depression, Diabetes Self-Care Activity and Glycemic Control in an Arab Population with Type 2 Diabetes
Authors Al-Ozairi A , Taghadom E, Irshad M , Al-Ozairi E
Received 24 June 2022
Accepted for publication 20 January 2023
Published 5 February 2023 Volume 2023:16 Pages 321—329
DOI https://doi.org/10.2147/DMSO.S377166
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Gian Paolo Fadini
Abdullah Al-Ozairi,1,2 Etab Taghadom,2,3 Mohammad Irshad,3 Ebaa Al-Ozairi3,4
1Department of Psychiatry, Faculty of Medicine, Kuwait University, Safat, Kuwait; 2Al-Amiri Hospital, Ministry of Health, Kuwait City, Kuwait; 3Dasman Diabetes Institute, Dasman, Kuwait; 4Department of Medicine, Faculty of Medicine, Kuwait University, Safat, Kuwait
Correspondence: Ebaa Al-Ozairi, Dasman Diabetes Institute, PO Box 1180, Dasman, 15462, Kuwait, Email [email protected]
Purpose: Poor self-care behavior and depression are associated with worse glycemic control, but the relationship between these variables is poorly reported. The present study aimed to describe self-care behaviors and explore the association between depression, self-care and glycemic control in people with type 2 diabetes in an Arab population.
Patients and Methods: This study recruited 446 patients with type-2 diabetes from an outpatient clinic in Kuwait and completed assessments of diabetes self-care using the Summary of Diabetes Self-Care Activities (SDSCA) questionnaire and depression using the Patients Health Questionnaire-9 (PHQ-9) scales. Multiple linear regression models were used to determine the associations between depression, self-care behaviors and glycemic control.
Results: Self-care behaviors were highest for medication taking (92.9%), an average for foot care (61.4%), blood glucose testing (60%) and healthy diet (55.7%), and lowest for exercise (27.1%). Depression, poor self-care activities and poor HbA1c levels were inter-correlated in univariate analysis (p< 0.03). In regression analysis, following healthful eating (B= − 0.27, p< 0.001), general eating plan (B= − 0.21, p= 0.01), more space carbohydrates evenly throughout the day (B= - 0.17, p= 0.03) and exercise at least 30 minutes (B= − 0.17, p= 0.02) behaviors were associated with better HbA1c levels. However, depression was associated with poor scores of following a general eating plan (B= − 0.20, p= 0.03), space carbohydrates evenly throughout the day (B= − 0.21, p= 0.05), and exercising at least 30 minutes (B= − 0.24, p= 0.03) behaviors. Depression scores were also associated with poor HbA1c levels (B= 0.32, p= 0.03). However, this association no longer persists after mutual adjustment with following a healthy diet (B= 0.14, p= 0.38) and exercise (B = 0.26, p = 0.08) behaviors.
Conclusion: Self-care activity was less than fifty percent in people with type 2 diabetes and higher activity was associated with better glycemic control. However, depression adversely affects self-care behaviors. To maintain and achieve glycemic control, diabetes educators might motivate people with type 2 diabetes to enhance their self-care activities, particularly those with depression symptoms and poor compliance with self-care activities.
Keywords: diabetes self-management education, self-care behavior, PHQ-9, SDSCA
Introduction
Arab populations have a very high prevalence of diabetes, with Kuwait having the highest prevalence with 24.9% of the population with diabetes (International Diabetes Federation 2021) and 40% with obesity.1 Depression is a common complication in individuals with type 2 diabetes.2 Studies have shown that depression is associated with poor adherence to diabetes self-care behaviors, such as monitoring blood sugar levels, eating a healthy diet, and taking medications as prescribed.3 This lead to poor glycemic control control4,5 and an increased risk of diabetes-related complications such as cardiovascular disease, neuropathy, nephropathy, and retinopathy.6,7
Medication regimens and self-care practices are two essential aspects of diabetes management.8 From the perspective of the patient, effective self-management of diabetes is beneficial to prevent the harmful effects of extremely low blood glucose levels (hypoglycemia) and the long-term development of any degenerative complications which have been shown to affect the quality of life.9 To prevent potential complications of diabetes, it is essential for people with diabetes to learn diabetes self-care skills and maintain a healthy lifestyle.5 People with diabetes can manage glycemic levels by consistently following the medication regimen and self-care practice.10 While difficulties in following medical advice are common and influenced by many factors.11 For example, a local study reported difficulties in following recommended dietary practices among patients with type 2 diabetes.12 Arab countries living standard has improved over the past four decades, which influenced dietary patterns, increased smoking behavior, and decreased physical activity.13 Depression, for instance, also leads to reduced motivation and difficulty following self-care tasks.14,15 It tends to unhealthy coping mechanisms, such as overeating or neglecting self-care activities.16
Successful diabetes self-care management requires lifestyle modification,11,17 which may be challenging to initiate and maintain.18 Therefore, regular screening of self-management advice received from their healthcare team and the extent to which they adhere to the self-management regimen are needed to identify where patients may strive to initiate and maintain behavior change.
To date, studies on diabetes self-care behaviors and depression in people with type 2 diabetes in the Arab populations are limited.19,20 Also, no study explored the association between self-care activities and depression in Arab people with type 2 diabetes.
This study aimed to describe diabetes self-care behaviors and explored the association between diabetes self-care behaviors and depression symptoms and HbA1c levels in people with type 2 diabetes in the Arab population. The result of this study may be helpful for healthcare providers to prepare a strategy for people with diabetes and depression in order to improve their self-care behaviors and glycemic control.
Materials and Methods
Study Population
This study was conducted at Dasman Diabetes Institute, Kuwait, from February 2018 to December 2019. The study was approved by Dasman Diabetes Institute Ethical Review Committee and followed the guidelines set out in the Declaration of Helsinki. The inclusion criteria were a diagnosis of type 2 diabetes based on the World Health Organization clinical criteria,21 21 years of age or over, and the ability to read and/or speak Arabic and Arab ethnicity. The exclusion criteria were diagnosed with severe mental disorders, schizophrenia, manic depression, depressive psychosis, active suicidal ideation, learning disability, dementia, alcohol and substance dependence, and severe personality disorders.
All participation was voluntary, and responses were kept anonymous and confidential. The research purpose, potential risks, and benefits, and the right to withdraw at any point without giving a reason for doing so, were all explained to the patients. The research assistant took full informed consent, distributed the questionnaire, and was available to answer all study-related queries.
Data Collection
The study data included gender, age, nationality (either Kuwaiti nationality or non-Kuwaiti Arabic), duration of diabetes, glucose-lowering medications, including insulin, and diagnosed complications. Body weight (kg) and height (measured to the closest 0.5 cm) were measured, and the body mass index (BMI) was calculated as weight/height2 (kg/m2). The values of glycated hemoglobin (HbA1c) and other clinical parameters were collected from the patient’s electronic health records.
Assessment of Diabetes Self-Care Behaviors
The Summary of Diabetes Self-Care Activities (SDSCA) scale was used to assess self-care behaviors during the past seven days.22,23 The English version of the revised SDSCA was forward translated into the Arabic language by two independent professional translators. The Arabic translation was then back-translated into English by two different bilingual, independent, professional translators. Once completed, the final version was reviewed by a panel of healthcare providers, including a diabetes nurse, diabetologist, and dietician. This was then piloted in a focus group of 15 patients with type 2 diabetes (10 females and 5 males; mean age of 45 years; and mean diabetes duration of 4 years) on two occasions, with a one-week interval. The original and back-translated versions were compared to assess the similarity of content.
For the assessment of self-care behaviors, 15 items of the SDSCA scale were used, and each item was rated according to how many days it was performed over the last week (0–7 days). A composite score was computed to represent the mean days of general self-care practices. Response of two items (on how many of last seven days “did you eat fat food such as red meat or full-fat dairy product” and “did you soak your fee”) were scored after reversing. Higher scores indicate greater self-care levels. The SDSCA items are categorized into five subscales: healthy diet (5 items; general diet (2 items), specific diet (3 items)), exercise (2 items), blood glucose testing (2 items), foot care (5 items) and medication (1 item).
The internal reliability (Cronbach’s α) of the Arabic-translated SDSCA scale in this study sample was 0.71, and the scale has a moderate level of reliability.24,25 The internal reliability for general diet (α= 0.87), specific diet (α= 0.28), physical activity (α= 0.85), blood glucose testing (α= 0.90), and foot care (α= 0.73) behaviors was also almost similar to the original studies25 and other published studies.26–29
Assessment of Depression Symptoms
The Patient Health Questionnaire-9 (PHQ-9) is a 9-item scale used to assess depression symptoms as per the Diagnostic and Statistical Manual for Mental Disorders- Edition IV. The score of each item ranges between 0 (not at all) and 3 (nearly every day), and the final score ranges between 0 and 27. A final score of ≥10 was defined as positive for depression (moderate to severe) symptoms.30 The internal reliability of PHQ-9 scale in this study was optimal (α = 0.84).31
Data Analysis
The collected data were analyzed using SPSS (version 25.0, IBM SPSS Statistics; IBM Corp., Armonk, NY). Individual items and subscales from the SDSCA were examined descriptively. Subscales scores were also converted to percentage scores. The depression symptoms were stratified between participants’ demographic and clinical characteristics and compared by Chi-square (χ2) or independent t-test. Bivariate correlation and multiple linear regression were used to explore the association between depression, self-care activities and HbA1c levels in the following models: unadjusted (Model 1) and adjusted for age, gender, BMI, and insulin medication (Model 2). The p≤ 0.05 was considered for the statistical significance of statistical analyses.
Results
Baseline Characteristics of Participants
The demographic and clinical characteristics of participants (n= 446) are displayed in Table 1. The mean age was 55.5 years, the proportion of males to females was almost equal. The mean duration of diabetes was 13 years (range 1 to 53 years). The mean BMI was 34 kg/m2, of which 106 (25%) participants were overweight and 287 (68%) were obese. Their mean HbA1c was 8.1%. The majority of the participants (79%) were prescribed oral glucose-lowering medication and 59% were also prescribed insulin. Depression symptoms were among 34% of the participants, more likely to be women (p< 0.001), were on insulin (p= 0.02), had higher body mass index (p= 001), and lower age groups (p= 0.03).
 |
Table 1 Participant Characteristics |
The majority of participants recall diabetes self-care recommendations received from their healthcare team. The participants received advice for the low-fat eating plan (61.8%), eat fewer sweets (46.2%), five portions of fruit and vegetables every day (34.4%), high-fiber diet (39.6%), and reduce energy intake to lose weight (31.4%). Participants also received advice for low-level exercise (such as walking) daily (63.8%), continuously exercising for at least 20 min at least three times per week (44.6%), fitting exercise into daily routines (31.4%), and engaging in a specific amount, type, duration, and level of exercise (10.9%) and test your blood sugar using a machine to read the results (75%) (data not shown in table).
Diabetes Self-Care Activities
Table 2 summarises participants’ responses to the SDSCA questions about self-care activities during the last seven days. The mean score of self-care behaviors on SDSCA was 3.4 (SD= 1.2) days/week. The highest scores were observed for taking medication (92.9%). The next highest scores were related to foot care (61.4%) and blood glucose testing (60.0%), and healthy eating (50.0%). The least commonly reported activity was engaging in exercise (27.1%).
 |
Table 2 Summary of Responses to Revised SDSCA Scale |
Association Analysis
The bivariate correlation result between diabetes self-care and depression shows a negative correlation (r = - 0.14, p = 0.004). Negative correlation was also found between self-care and Hba1c level (r = −0.10, p = 0.04), whereas a positive correlation was found between depression and HbA1c level (r = 0.11, p = 0.03).
Table 3 presents the statistical association between individual items of self-care behavior, depression and HbA1c level. In the unadjusted model, the individual followed a healthful eating plan (B = −0.24, p < 0.001), general eating plan (B= −0.20, p= 0.01), space carbohydrates evenly throughout the day (B= −0.15, p= 0.03), and participating in exercise sessions at least 30 minutes (B= −0.23, p< 0.001) were significantly associated with lower HbA1c (Model 1). The association remains significant even after adjustment with age, gender, body metabolic index, and insulin medication (Model 2). The items, “eat less high-fat food” (B= −0.12; p= 0.04) and “participating in specific exercise sessions” (B= −0.14, p= 0.04) were also significantly associated with better HbA1c results in unadjusted Model 1 but not in Model 2.
 |
Table 3 Regression Analysis Between Diabetes Self-Care Activities (Dependent Variable) and HbA1c |
Table 4 presents the statistical associations between depression and diabetes self-care activities. The higher PHQ-9 score was significantly associated with lower (ie worse) scores on following general eating (B= −0.22, p= 0.02), participating in exercise sessions at least 30 minutes (B= −0.34, p = 0.001) and specific exercise sessions (B= −0.32, p = 0.001) behaviors, in Model 1 and this association remains significant in Model 2. The PHQ-9 scores were also associated with an individual item “space carbohydrates evenly through the day” (B= −0.21, p= 0.05) in Model 2. The PHQ-9 scores were also associated with poorer HbA1c results (B= 0.32, p= 0.03) in Model 1. However, this association was not significant in Model 2. The association between the PHQ-9 and HbA1c also did not persist after the mutual adjustment with following a healthy diet plan (B= 0.14, p= 0.38) and exercise (B = 0.26, p = 0.08) behaviors (data not shown in table).
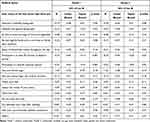 |
Table 4 Regression Analysis Between Depression (Dependent Variables), Diabetes Self-Care Activities and HbA1c |
Discussion
This study described self-care behavior and explored the association between depression and HbA1c levels in people with type 2 diabetes in an Arab population. The results of the current study evidence a high prevalence of depression symptoms among people with type 2 diabetes and negatively associated with diabetes self-care behaviors and glycemic control. The results found a positive relationship between self-care behaviors and glycemic control.
The participants reported high levels of self-care behavior for administering medication, followed by blood glucose testing, foot care, and healthy diet. The least reported behaviors were spacing carbohydrates evenly through the day and engaging in exercise. A similar study was conducted among Chinese people with type 2 diabetes, where the highest scores were for exercise and lower for foot care and blood glucose monitoring behaviors.32 The current results for self-care behavior are consistent with the revised SDSCA validation studies,26–29 and a systematic review by Toobert et al,23 who reported higher levels of self-care for blood glucose testing (60–82%) and general dietary (48–65%) rather than exercise (25–55%) behaviors.23 Regarding foot care, fairly high levels of foot care in the current study compared to these reports23,32 was due to Islamic religious practices. Islam is the dominant religion in Kuwait. People are expected to wash their feet five times a day before prayers; hence, the high positive response to these questions.19
In the current study, higher self-care activity was associated with better glycemic control. The self-care behaviors that contributed to glycemic control were healthy eating, more evenly spacing carbohydrates in meals and snacks, and exercise. The result was consistent with many studies, which reported a positive association between healthy diet and glycemic control.33,34 Another study also reported that the following recommended carbohydrate and fat balance diet improves glycemic levels and weight loss.35 Similarly, a significant reduction of HbA1c was observed with more intense exercise.36 On the other hand, those who did not follow healthy dietary behaviors and exercise activities lost their glycemic control.37 In addition, medication administration and self-monitoring of blood glucose behaviors are likely to help in glycemic control.34 However, this association was not found in the current study population.
In the current study, approximately one-third of people had depression symptoms, and the prevalence of depression symptoms in the Kuwaiti Arab population is higher than the other diabetes populations.38,39 Regarding the association between self-care and depression, healthy eating plans and exercise behaviors were low in people with depression symptoms. Many studies reported that depression was associated with problems engaging with exercise, diet, and medication self-care behaviors40,41 and markedly impaired the quality of diabetes self-care management.40,42 The relationship between depression and worse glycemic control is well documented in the literature.15,43 The present study supports the notion that the impact of depression on glycemic management is not necessarily culture bound. However, following healthy eating and exercise behaviors may protect against the worse association between depression and glycemic control. Furthermore, consistently engaging in self-care may prevent the negative effects of an illness from worsening. The present findings suggest that following healthy eating and exercise behaviors are more likely to help glycemic management. This particular area of behavior needs to improve for those with lower scores on self-care behavior, particularly for depressed people.
Conclusions
This study showed that diabetes self-care activities was less than fifty percent in people with type 2 diabetes. Depression was associated with low compliance with healthy diet and exercise behaviors. However, healthy eating and exercise behaviors were essential aspects of self-care behaviors and likely to help in glycemic control. The result suggests that diabetes educators might encourage people with type 2 diabetes to improve their self-care behaviors, especially for exercise and healthy diet plans.
Human and Animal Rights
No animals were used in this research. All participants were human and followed the research procedures in accordance with the ethical standards of the institute’s ethical committee for human experimentation. This study was conducted in accordance with the Declaration of Helsinki. The confidentiality of the information was assured and only used for scientific purposes.
Data Sharing Statement
Data will be available upon reasonable request from the corresponding author.
Ethics Approval and Consent to Participate
The Ethical Committee of Dasman Diabetes Institute, Kuwait, approved this study. Each participant signed the informed consent before enrolment in this study.
Acknowledgments
We would like to thank all the participants for giving up their time to participate in this study. The authors also thank to Dr Debbie Cooke and Dr Stuart Gray for editing and support. We gratefully acknowledge Dasman Diabetes Institute for its facility and support.
Funding
There is no funding to report.
Disclosure
The authors declared no conflicts of interest in this study.
References
1. International Diabetes Federation (IDF). IDF diabetes atlas, 10th Edition; 2021. Available from: https://diabetesatlas.org/idfawp/resource-files/2021/07/IDF_Atlas_10th_Edition_2021.pdf.
2. Al-Ozairi E, Al Ozairi A, Blythe C, Taghadom E, Ismail K. The epidemiology of depression and diabetes distress in type 2 diabetes in Kuwait. J Diabetes Res. 2020;2020:7414050. doi:10.1155/2020/7414050
3. Ciechanowski P, Russo J, Katon W, et al. Influence of patient attachment style on self-care and outcomes in diabetes. Psychosom Med. 2004;66(5):720–728. doi:10.1097/01.psy.0000138125.59122.23
4. Otieno CF, Kanu JE, Karari EM, Okech-Helu V, Joshi MD, Mutai K. Glucose-lowering therapies, adequacy of metabolic control, and their relationship with comorbid depression in outpatients with type 2 diabetes in a tertiary hospital in Kenya. Diabetes Metabol Syndr Obes. 2017;10:141. doi:10.2147/DMSO.S124473
5. Crispín-Trebejo B, Robles-Cuadros MC, Bernabé-Ortiz A. Association between depression and glycemic control among type 2 diabetes patients in Lima, Peru. Asia Pacific Psychiatr. 2015;7(4):419–426. doi:10.1111/appy.12190
6. Lustman PJ, Anderson RJ, Freedland KE, de Groot M, Carney RM, Clouse RE. Depression and poor glycemic control: a meta-analytic review of the literature. Diabetes Care. 2000;23(7):934–942. doi:10.2337/diacare.23.7.934
7. Egede LE, Zheng D, Simpson K. Comorbid depression is associated with increased health care use and expenditures in individuals with diabetes. Diabetes Care. 2002;25(3):464–470. doi:10.2337/diacare.25.3.464
8. Jannoo Z, Mamode Khan N. Medication adherence and diabetes self-care activities among patients with type 2 diabetes mellitus. Value Health Region Issues. 2019;18:30–35. doi:10.1016/j.vhri.2018.06.003
9. Hopkins R, Shaver K, Weinstock RS. Management of adults with diabetes and cognitive problems. Diabetes Spectr. 2016;29(4):224–237. doi:10.2337/ds16-0035
10. Association of Diabetes Care and Education Specialists, and Leslie Kolb. An effective model of diabetes care and education: the ADCES7 self-care behaviors™. Sci Diabetes Self Manage Care. 2021;47(1):30–53. doi:10.1177/0145721720978154
11. Reyes J, Tripp-Reimer T, Parker E, Muller B, Laroche H. Factors influencing diabetes self-management among medically underserved patients with type II diabetes. Glob Qual Nurs Res. 2017;4:2333393617713097. doi:10.1177/2333393617713097
12. Al-Kaabi J, Al-Maskari F, Saadi H, Afandi B, Parkar H, Nagelkerke N. Assessment of dietary practice among diabetic patients in the United Arab Emirates. Rev Diabet Stud. 2008;5(2):110–115. doi:10.1900/RDS.2008.5.110
13. Musaiger AO, Takruri HR, Hassan AS, Abu-Tarboush H. Food-based dietary guidelines for the Arab gulf countries. J Nutr Metab. 2012;2012:905303. doi:10.1155/2012/905303
14. Mut-Vitcu G, Timar B, Timar R, Oancea C, Citu IC. Depression influences the quality of diabetes-related self-management activities in elderly patients with type 2 diabetes: a cross-sectional study. Clin Interv Aging. 2016;11:471–479. doi:10.2147/CIA.S104083
15. Lin EH, Katon W, Von Korff M, et al. Relationship of depression and diabetes self-care, medication adherence, and preventive care. Diabetes Care. 2004;27(9):2154–2160. doi:10.2337/diacare.27.9.2154
16. Bădescu SV, Tătaru C, Kobylinska L, et al. The association between diabetes mellitus and depression. J Med Life. 2016;9(2):120–125.
17. Pfeiffer AFH, Klein HH. The treatment of type 2 diabetes. Dtsch Arztebl Int. 2014;111(5):69–82. doi:10.3238/arztebl.2014.0069
18. Rise MB, Pellerud A, Rygg LØ, Steinsbekk A. Making and maintaining lifestyle changes after participating in group based type 2 diabetes self-management educations: a qualitative study. PLoS One. 2013;8(5):e64009–e64009. doi:10.1371/journal.pone.0064009
19. Abdulghani HM, AlRajeh AS, AlSalman BH, et al. Prevalence of diabetic comorbidities and knowledge and practices of foot care among diabetic patients: a cross-sectional study. Diabetes Metab Syndr Obes. 2018;11:417–425. doi:10.2147/DMSO.S171526
20. Almomani MH, Al-Tawalbeh S. Glycemic control and its relationship with diabetes self-care behaviors among patients with type 2 diabetes in Northern Jordan: a cross-sectional study. Patient Prefer Adherence. 2022;16:449–465. doi:10.2147/PPA.S343214
21. American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2011;34(Suppl1):S62–S69. doi:10.2337/dc11-S062
22. Toobert DJ, Glasgow RE. Assessing diabetes self-management: the summary of diabetes self-care activities questionnaire. Handbook Psychol Diabetes. 1994;351:75.
23. Toobert DJ, Hampson SE, Glasgow RE. The summary of diabetes self-care activities measure: results from 7 studies and a revised scale. Diabetes Care. 2000;23(7):943–950. doi:10.2337/diacare.23.7.943
24. Schmitt A, Reimer A, Hermanns N, et al. Assessing diabetes self-management with the Diabetes Self-Management Questionnaire (DSMQ) can help analyse behavioural problems related to reduced glycaemic control. PLoS One. 2016;11(3):e0150774. doi:10.1371/journal.pone.0150774
25. Glasgow RE, Toobert DJ, Riddle M, Donnelly J, Mitchell DL, Calder D. Diabetes-specific social learning variables and self-care behaviors among persons with type II diabetes. Health Psychol. 1989;8(3):285–303. doi:10.1037/0278-6133.8.3.285
26. Glasgow RE, Toobert DJ, Hampson SE, Brown JE, Lewinsohn PM, Donnelly J. Improving self-care among older patients with type II diabetes: the “Sixty Something” Study. Patient Educ Couns. 1992;19(1):61–74. doi:10.1016/0738-3991(92)90102-O
27. Glasgow RE, Toobert DJ. Brief, computer-assisted diabetes dietary self-management counseling: effects on behavior, physiologic outcomes, and quality of life. Med Care. 2000;38(11):1062–1073. doi:10.1097/00005650-200011000-00002
28. Glasgow RE, Strycker LA, Toobert DJ, Eakin E. A social-ecologic approach to assessing support for disease self-management: the Chronic Illness Resources Survey. J Behav Med. 2000;23(6):559–583. doi:10.1023/A:1005507603901
29. Feil EG, Glasgow RE, Boles S, McKay HG. Who participates in Internet-based self-management programs? A study among novice computer users in a primary care setting. Diabetes Educ. 2000;26(5):806–811. doi:10.1177/014572170002600509
30. Reddy P, Philpot B, Ford D, Dunbar JA. Identification of depression in diabetes: the efficacy of PHQ-9 and Hads-D. Br J Gen Pract. 2010;60(575):e239–e245. doi:10.3399/bjgp10X502128
31. Al Ozairi A, Alsaeed D, Al-Ozairi E, Irshad M, Crane RS, Almoula A Effectiveness of virtual mindfulness-based interventions on perceived anxiety and depression of physicians during the COVID-19 pandemic: A pre-post experimental study. Front Psychiatry. 2023;13:1089147. doi:10.3389/fpsyt.2022.1089147
32. Yang J, Zhang Z, Zhang L, Su Y, Sun Y, Wang Q. Relationship between self-care behavior and cognitive function in hospitalized adult patients with type 2 diabetes: a cross-sectional study. Diabetes Metabol Syndr Obes. 2020;13:207. doi:10.2147/DMSO.S236966
33. American Diabetes Association. Standards of medical care in diabetes--2012. Diabetes Care. 2012;35(Suppl 1):S11–S63. doi:10.2337/dc12-s011
34. Houle J, Beaulieu MD, Chiasson JL, et al. Glycaemic control and self-management behaviours in Type 2 diabetes: results from a 1-year longitudinal cohort study. Diabet Med. 2015;32(9):1247–1254. doi:10.1111/dme.12686
35. Garbutt J, England C, Jones AG, Andrews RC, Salway R, Johnson L. Is glycaemic control associated with dietary patterns independent of weight change in people newly diagnosed with type 2 diabetes? Prospective analysis of the early-ACTivity-in-diabetes trial. BMC Med. 2022;20(1):161. doi:10.1186/s12916-022-02358-5
36. Kirwan JP, Sacks J, Nieuwoudt S. The essential role of exercise in the management of type 2 diabetes. Cleve Clin J Med. 2017;84(7 Suppl 1):S15–s21. doi:10.3949/ccjm.84.s1.03
37. Alaradi M, Ouagueni A, Khatib R, Attieh G, Bawadi H, Shi Z. Dietary patterns and glycaemic control among Qatari adults with type 2 diabetes. Public Health Nutr. 2021;24(14):4506–4513. doi:10.1017/S1368980020003572
38. Dinh Le T, Huy Duong H, Thi Nguyen L, Phi Thi Nguyen N, Tien Nguyen S, Van Ngo M. The relationship between depression and multifactorial control and microvascular complications in Vietnamese with type 2 diabetes mellitus aged 30–60 years. Diabetes Metabol Syndr Obes. 2022;1185–1195. doi:10.2147/DMSO.S354443
39. Ding X, Rong S, Wang Y, et al. The association of the prevalence of depression in type 2 diabetes mellitus with visual-related quality of life and social support. Diabetes Metabol Syndr Obes. 2022;15:535–544. doi:10.2147/DMSO.S343926
40. Jahan F, Jabbar A, Naqvi H, Awan S. Depression in patients with diabetes mellitus and its impact on diabetes self-care, medication adherence and glycemic control. Int J Diabetes Dev Ctries. 2011;31(3):154. doi:10.1007/s13410-011-0036-0
41. Devarajooh C, Chinna K. Depression, distress and self-efficacy: the impact on diabetes self-care practices. PLoS One. 2017;12(3):e0175096. doi:10.1371/journal.pone.0175096
42. Shrestha M, Al-Ghareeb A, Alenazi F, Gray R. Association between subthreshold depression and self-care behaviour in people with type 2 diabetes: a protocol for systematic review of observational studies. Syst Rev. 2019;8(1):167. doi:10.1186/s13643-019-1084-7
43. Łukasiewicz A, Kiejna A, Cichoń E, Jodko-Modlińska A, Obrębski M, Kokoszka A. Relations of well-being, coping styles, perception of self-influence on the diabetes course and sociodemographic characteristics with HbA1c and BMI among people with advanced type 2 diabetes mellitus. Diabetes Metabol Syndr Obes. 2022;15:407–418. doi:10.2147/DMSO.S320909
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
