Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 15
Association Between Comorbid Chronic Obstructive Pulmonary Disease and Prognosis of Patients Admitted to the Intensive Care Unit for Non-COPD Reasons: A Retrospective Cohort Study
Authors Huang W, Xie R, Hong Y, Chen Q
Received 28 December 2019
Accepted for publication 21 January 2020
Published 7 February 2020 Volume 2020:15 Pages 279—287
DOI https://doi.org/10.2147/COPD.S244020
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Chunxue Bai
Wencheng Huang,1 Ruijie Xie,2 Yuancheng Hong,1 Qingui Chen2
1Department of Respiratory Medicine, The 910th Hospital of People’s Liberation Army, Quanzhou, People’s Republic of China; 2Department of Medical Intensive Care Unit, The First Affiliated Hospital, Sun Yat-Sen University, Guangzhou, People’s Republic of China
Correspondence: Qingui Chen
Department of Medical Intensive Care Unit, The First Affiliated Hospital, Sun Yat-Sen University, No. 58 Zhongshan Road 2, Guangzhou 510080, People’s Republic of China
Tel +86-135 8044 2523
Email [email protected]
Background and Aim: Chronic obstructive pulmonary disease (COPD) is a rather common comorbid condition among patients admitted to the intensive care unit (ICU), while evidence of how this comorbidity affects prognosis is limited. This study aimed to investigate the associations between COPD comorbidity and prognoses of patients who were admitted to the ICU for non-COPD reasons, and to examine whether the associations varied between different types of ICU.
Methods: A retrospective cohort study was performed using data extracted from a freely accessible critical care database (MIMIC-III). Adult (≥ 18 years) patients of first ICU admission in the database were enrolled as study participants but those with a primary diagnosis of COPD were excluded. The primary endpoint was 28-day mortality after ICU admission and multivariable Cox regression analyses were employed to assess the associations between COPD comorbidity and the study endpoints. Different adjusting models including a propensity score were used to adjust potential confounders.
Results: A total of 29,499 patients were enrolled finally, among which 3,332 patients (11.30%) were comorbid with COPD. A higher 28-day mortality was observed among patients with COPD than those without COPD (13.90% versus 8.07%, P< 0.001), but there was no statistically significant difference in the proportion of patients who needed mechanical ventilation on the first day after ICU admission between the two groups. Multivariable Cox regression analyses found a significant association between COPD comorbidity and 28-day mortality (adjusted hazard ratio=1.32, 95% confidence interval=1.19– 1.47, P< 0.0001). The associations were broadly consistent among patients admitted to different types of ICU, but a much higher estimate was observed in patients admitted to cardiac surgery recovery unit (adjusted hazard ratio=2.03, 95% confidence interval=1.44– 2.86, P< 0.0001).
Conclusion: Comorbid COPD increased the risk of 28-day mortality among patients admitted to the ICU for non-COPD reasons, especially for those admitted to the cardiac surgery recovery unit.
Keywords: chronic obstructive pulmonary disease, comorbidity, intensive care units, prognosis, risk factors
Introduction
Chronic obstructive pulmonary disease (COPD) is the third leading cause of death worldwide, with a global prevalence of 10.1% in 2017.1 As the prevalence of COPD increases globally2,4 and the size of the aging population grows resulting from improvements in healthcare and social circumstances,5 it is not surprising to find that COPD becomes a rather common comorbid condition among patients admitted to the intensive care unit (ICU). According to a study from Austria,6 8.6% of ICU patients had COPD and they had higher risk-adjusted mortality when compared with those without COPD. To the best of our knowledge, however, evidence of how comorbid COPD affects prognosis of critically ill patients is still very limited, especially for patients admitted to the ICU for non-COPD reasons. Available research mainly focused on patients admitted to the ICU due to COPD and investigated relevant risk factors or interventions associated with clinical outcomes.7,10 Considering that COPD is usually associated with other comorbidities, it might be worthy to investigate whether the impact of comorbid COPD on the prognosis of critically ill patients is consistent for those admitted to the ICU but not for a COPD reason. In this study, we aimed to evaluate the associations between comorbid COPD and prognoses of patients admitted to the ICU for non-COPD reasons, and to examine whether the associations varied between different types of ICU.
Methods
Study Design and Data Source
The study used a retrospective cohort study design. Data from a freely accessible critical care database, Medical Information Mart for Intensive Care III (MIMIC-III),11 were analyzed retrospectively. In brief, the database consisted of clinical data of patients who stayed in the ICU of Beth Israel Deaconess Medical Center between 2001 and 2012. Access to the database was approved by the institutional review boards of both Beth Israel Deaconess Medical Center and Massachusetts Institute of Technology Affiliates. No informed consent was required since all the data were de-identified.
Study Population
All the adult (≥18 years) patients were considered to be enrolled as study participants, but only those of the first ICU admission in the first hospitalization were chosen if they had more than one admission record in the database. We excluded patients whose lengths of first ICU stay were less than 24 hours and whose primary diagnosis were COPD. To avoid potential typos in the original data, we excluded patients whose lengths of hospital stay were shorter than the lengths of ICU stay. The detailed procedure for study participants selection was presented in Figure 1.
 |
Figure 1 Flow chart of the study participants. Abbreviations: ICU, intensive care unit; COPD, chronic obstructive pulmonary disease. |
Data Extraction
As previously described,12,13 data extraction was performed using Structured Query Language and codes from the MIMIC Code Repository (https://github.com/MIT-LCP/mimic-code).14 COPD was identified using International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes (490, 4910, 4911, 4912, 49,120, 49,121, 49,122, 4918, 4919, 4920, 4928, 494, 4940, 4941, 496).15 Apart from the exposure (comorbid with COPD or not) and clinical outcome variables, the following variables were extracted or calculated: age, sex, types of ICU admission (urgent or not), types of ICU, Simplified Acute Physiology Score II (SAPS II) on ICU admission,16 and the Elixhauser Comorbidity Index (SID30).17 Sepsis, and some other specific comorbidities, were also identified using ICD-9-CM codes. Variables about therapies including mechanical ventilation and renal replacement therapy on the first day after ICU admission were also extracted.
Outcome Variables
The following outcome variables were extracted: 28-day mortality (after ICU admission), ICU mortality, hospital mortality, length of ICU stay, length of hospital stay. Among them, 28-day mortality was chosen as the primary endpoint of the study, and ICU mortality was chosen as the second endpoint, while other outcomes were extracted for descriptive purposes only. Since a patient might have more then one ICU admission during one hospitalization, ICU mortality and length of ICU stay were determined only by the first ICU admission.
Calculation of Propensity Scores
Patients were categorized as comorbid COPD or not according to whether they had any COPD diagnosis codes mentioned above, and a propensity score for each patient was calculated to estimate their probability of being comorbid COPD or not using multivariable logistic regression models given the following covariates: sex, age (years), type of admission, SAPS II on admission, sepsis, mechanical ventilation on first day, renal replacement therapy on first day, congestive heart failure, cardiac arrhythmias, valvular disease, pulmonary circulation disorder, peripheral vascular disorder, hypertension, paralysis, other neurological disease, uncomplicated diabetes, complicated diabetes, hypothyroidism, renal failure, liver disease, peptic ulcer, acquired immune deficiency syndrome (AIDS), lymphoma, metastatic cancer, solid tumor, rheumatoid arthritis, coagulopathy, obesity, weight loss, fluid and electrolyte disorders, blood loss anemia, deficiency anemia, alcohol abuse, drug abuse, psychoses, and depression.
Statistical Analysis
Data were presented as mean±standard deviation, median (25th–75th percentiles), or numbers (percentages) according to types and distributions of variables. Kruskal Wallis and Chi-square (or Fisher’s exact) tests were used for comparisons between groups. Kaplan-Meier method and Log rank tests were used to compare survival distributions among patients with comorbid COPD or not. Associations of comorbid COPD with primary endpoint and second endpoint were assessed using Cox regression models and logistic regression models, respectively. We used three different models to adjust potential confounders: (1) model 1, including sex, age (years), type of admission, SAPS II on admission, sepsis, mechanical ventilation on first day, renal replacement therapy on first day, and Elixhauser comorbidity index (SID30); (2) model 2, the same as model 1, but Elixhauser comorbidity index (SID30) was replaced with specific comorbidities, including congestive heart failure, cardiac arrhythmias, valvular disease, pulmonary circulation disorder, peripheral vascular disorder, hypertension, paralysis, other neurological disease, uncomplicated diabetes, complicated diabetes, hypothyroidism, renal failure, liver disease, peptic ulcer, AIDS, lymphoma, metastatic cancer, solid tumor, rheumatoid arthritis, coagulopathy, obesity, weight loss, fluid and electrolyte disorders, blood loss anemia, deficiency anemia, alcohol abuse, drug abuse, psychoses, and depression; (3) Model 3, a propensity score as mentioned above. P-values of less than 0.05 were considered to indicate statistical significance. Empower(R) (www.empowerstats.com; X&Y solutions, Inc., Boston, MA) and R software, version 3.6.1 (http://www.r-project.org) were used for statistical analyses.
Results
Baseline Characteristics of the Study Population
A total of 29,499 patients were enrolled finally, among which 3,332 patients (11.30%) had COPD comorbidity. The average age of the study population was 63.88±17.07 years, and patients with COPD comorbidity had a significantly higher average age than that of patients without COPD (71.66±11.50 versus 62.89±17.40 years, P<0.001). More patients with COPD were male, but the difference between groups was small (54.47% versus 57.24%, P=0.002). Patients with COPD comorbidity accounted for a higher percentage of patients admitted to the medical intensive care unit (MICU) and coronary care unit (CCU). No statistically significant difference was observed in the types of admission, proportions of patients who suffered from sepsis, or those who needed mechanical ventilation or renal replacement therapy on the first day after ICU admission between the two groups. However, when compared with patients without COPD, patients with COPD had higher SAPS II on admission, and a higher percentage of them suffered from most of the other comorbidities. Detailed results are presented in Table 1.
 |
Table 1 Comparison of Baseline Characteristics and Prognosis Between Patients in the Intensive Care Unit with and without COPD |
Clinical Outcomes of the Study Population
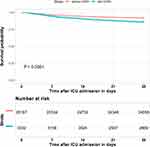
In total, 2,574 patients (8.73%) of the study population died within 28 days after ICU admission, while a higher 28-day mortality rate (13.90% versus 8.07%, P<0.001) was observed among patients with COPD than those without COPD, and similar results were found for ICU mortality (4.47% versus 2.86%, P<0.001) and hospital mortality (9.33% versus 6.37%, P<0.001). The median lengths of ICU stay and hospital stay were close between the two groups, though the differences were significant. Detailed results are also presented in Table 1. The Kaplan-Meier survival curves presented in Figure 2 depictthe survival distributions of patients with or without COPD within 28 days after ICU admission, and the comparison between the two groups revealed significantly better survival of patients without COPD comorbidity (Log rank test; P<0.0001).
Associations Between Comorbid COPD and Clinical Outcomes
Results of multivariable Cox regression analyses indicated that comorbid COPD was a risk factor for 28-day mortality with a crude hazard ratio (HR) of 1.77 [95% confidence interval (CI)=1.60–1.96], and the association was still significant and consistent after being adjusted by the three different models (HR=1.32, 95% CI=1.19–1.47, adjusted by model 3; results of the other two models were presented in Table 2). Analyses of the second endpoint indicated that comorbid COPD also increased the risk of ICU mortality [odds ratio (OR)=1.24, 95% CI=1.03–1.49, adjusted by model 3; the results of the other two models are also presented in Table 2].
 |
Table 2 Association between Comorbid COPD and Prognosis |
After being stratified by types of ICU, as presented in Table 3, estimates of the association between comorbid COPD and 28-day mortality among patients admitted to different types of ICU were broadly consistent, but a much higher estimate was observed in patients admitted to the cardiac surgery recovery unit (CSRU) (HR=2.03, 95% CI=1.44–2.86, adjusted by model 3). However, estimates of the association between comorbid COPD and ICU mortality after being stratified by types of ICU varied, and a significant inverse association (OR=0.46, 95% CI=0.23–0.91) was observed in patients admitted to the surgical intensive care unit (SICU).
 |
Table 3 Association of Comorbid COPD with Prognosis Stratified by Types of ICU |
Discussion
The study selected patients who were admitted to the ICU for non-COPD reasons as the study population and investigated the associations between comorbid COPD and clinical outcomes. Data from a large critical care database were analyzed retrospectively, which made a large sample size available. Results of the study indicated that comorbid COPD was an independent risk factor for critically ill patients admitted to the ICU for non-COPD reasons, which would increase the risk of 28-day mortality after ICU admission by about 30%, and even higher for patients admitted to the CSRU.
Compared with Funk et al,6 which seems to be the only one study currently available that includes a large sample size and also investigates the impact of comorbid COPD on clinical outcomes for critically ill patients admitted to the ICU for non-COPD reasons, the results of our study are different in several aspects. Our study found a higher prevalence of COPD comorbidity in ICU patients (11.30% versus 8.6%), which might be related to the fact that the prevalence of COPD was higher in the United State than in Austria18,19 and that Funk et al’s study also included patients admitted to the ICU for COPD reasons. It is noteworthy that in our study patients with a primary diagnosis of COPD accounted for a much lower proportion of patients with COPD [3.48% (120/3,452), see Figure 1, compared with 29.02% (4,868/16,774) in Funk et al’s study]. This might be attributed to potential measurement error which will be discussed below. However, in our study there was no statistically significant difference in the proportion of patients who needed mechanical ventilation on the first day after ICU admission between patients with COPD and without COPD, so the identification of patients with COPD but not admitted for COPD in our study was still reliable. Conclusions on the associations of COPD comorbidity with mortality between the two studies were similar, but we did not analyze outcomes such as prolonged mechanical ventilation, tracheotomy, or prolonged weaning, since evaluating these outcomes might be essential only when patients admitted to the ICU for COPD were investigated. One strength of our study was that different models including a propensity score were employed to adjust potential confounders, especially in the stratified analyses when sample sizes of each strata were limited.20
Some results we found in the study are also worth discussion. A much higher HR was observed in patients admitted to the CSRU in our study, which supported that comorbid COPD might influence the outcomes of patients who underwent cardiac surgery. Results from other studies were not consistent in this issue. Efird et al21 found that COPD was a risk factor of long-term survival after coronary artery bypass grafting surgery with a HR of 1.8, while Manganas et al22 concluded that mortality associated with coronary artery bypass grafting surgery was not influenced by COPD. Another result that needs to be discussed was the inverse association between comorbid COPD and ICU mortality for SICU patients, which seems counter-intuitive. We thought this was related to the definition of ICU mortality in the study, because we determined ICU mortality only according to the first ICU admission (if a patient had more than one ICU admission during his/her first hospitalization). It was reasonable that a patient was first admitted to a SICU and got prepared for a surgery and then was transferred out of the ICU for the surgery. In this situation, using hospital mortality would be more reasonable to assess the association and, indeed, the OR became not significant when hospital mortality was used as the clinical outcome (OR=0.84, 95% CI=0.59–1.21) for the same patients admitted to SICU (data not shown).
There were some limitations of the study. Measurement error caused by identifying COPD or other comorbidities using ICD-9-CM codes might be the most important one. Due to the retrospective study design and limitation of the data, we only used ICD-9-CM codes to identify COPD as previously reported,15 however, this method was found to misclassify the majority of patients who had COPD.22 Other limitations of the study included other intrinsic defects in a retrospective cohort study, unavailability of data on severity of COPD which might be a confounder, single unit design, and the inability to investigate time trends due to blindness to time information in the database for privacy reasons. Therefore, prospective studies are still needed to further confirm our results.
Conclusion
Comorbid COPD increased the risk of 28-day mortality among patients admitted to the ICU for non-COPD reasons, especially for those admitted to the cardiac surgery recovery unit.
Abbreviations
COPD, Chronic obstructive pulmonary disease; ICU, intensive care unit; MIMIC-III, Medical Information Mart for Intensive Care III; ICD-9-CM, International Classification of Diseases, Ninth Revision, Clinical Modification; SAPS II, Simplified Acute Physiology Score II; AIDS, acquired immune deficiency syndrome; MICU, medical intensive care unit; CCU, coronary care unit; HR, hazard ratio; CI, confidence interval; OR, odds ratio; CSRU, cardiac surgery recovery unit; SICU, surgical intensive care unit; TSICU, trauma/surgical intensive care unit.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Celli BR, Wedzicha JA. Update on clinical aspects of chronic obstructive pulmonary disease. N Engl J Med. 2019;381(13):1257–1266. doi:10.1056/NEJMra1900500
2. Collaborators GBDCRD. Global, regional, and national deaths, prevalence, disability-adjusted life years, and years lived with disability for chronic obstructive pulmonary disease and asthma, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet Respir Med. 2017;5(9):691–706. doi:10.1016/S2213-2600(17)30293-X
3. Fang L, Gao P, Bao H, et al. Chronic obstructive pulmonary disease in China: a nationwide prevalence study. Lancet Respir Med. 2018;6(6):421–430. doi:10.1016/S2213-2600(18)30103-6
4. India State-Level Disease Burden Initiative CRDC. The burden of chronic respiratory diseases and their heterogeneity across the states of India: the Global Burden of Disease Study 1990–2016. Lancet Glob Health. 2018;6(12):e1363–e1374. doi:10.1016/S2214-109X(18)30409-1
5. The Lancet Public H. Ageing: a 21st century public health challenge? Lancet Public Health. 2017;2(7):e297. doi:10.1016/S2468-2667(17)30125-1
6. Funk GC, Bauer P, Burghuber OC, et al. Prevalence and prognosis of COPD in critically ill patients between 1998 and 2008. Eur Respir J. 2013;41(4):792–799. doi:10.1183/09031936.00226411
7. Berk Takir H, Kargin F, Salturk C, et al. Reasons of intensive care unit admission in COPD patients. Eur Respir J. 2013;42.
8. Daubin C, Valette X, Thiolliere F, et al. Procalcitonin algorithm to guide initial antibiotic therapy in acute exacerbations of COPD admitted to the ICU: a randomized multicenter study. Intensive Care Med. 2018;44(4):428–437. doi:10.1007/s00134-018-5141-9
9. Ongel EA, Karakurt Z, Salturk C, et al. How do COPD comorbidities affect ICU outcomes? Int J Chron Obstruct Pulmon Dis. 2014;9:1187–1196. doi:10.2147/COPD.S70257
10. Wildman MJ, Sanderson CF, Groves J, et al. Survival and quality of life for patients with COPD or asthma admitted to intensive care in a UK multicentre cohort: the COPD and Asthma Outcome Study (CAOS). Thorax. 2009;64(2):128–132. doi:10.1136/thx.2007.091249
11. Johnson AE, Pollard TJ, Shen L, et al. MIMIC-III, a freely accessible critical care database. Sci Data. 2016;3:160035. doi:10.1038/sdata.2016.35
12. Chen Q, Zhang L, Ge S, He W, Zeng M. Prognosis predictive value of the Oxford acute severity of illness score for sepsis: a retrospective cohort study. PeerJ. 2019;7:e7083. doi:10.7717/peerj.7083
13. Chen Q, Huang K, Li L, et al. Serum uric acid on admission cannot predict long-term outcome of critically ill patients: a retrospective cohort study. Ther Clin Risk Manag. 2018;14:1347–1359. doi:10.2147/TCRM
14. Johnson AE, Stone DJ, Celi LA, Pollard TJ. The MIMIC code repository: enabling reproducibility in critical care research. J Am Med Inform Assoc. 2018;25(1):32–39. doi:10.1093/jamia/ocx084
15. Tsugawa Y, Jha AK, Newhouse JP, Zaslavsky AM, Jena AB. Variation in physician spending and association with patient outcomes. JAMA Intern Med. 2017;177(5):675–682. doi:10.1001/jamainternmed.2017.0059
16. Le Gall JR, Lemeshow S, Saulnier F. A new Simplified Acute Physiology Score (SAPS II) based on a European/North American multicenter study. JAMA. 1993;270(24):2957–2963. doi:10.1001/jama.1993.03510240069035
17. Steiner C, Elixhauser A, Schnaier J. The healthcare cost and utilization project: an overview. Eff Clin Pract. 2002;5(3):143–151.
18. Schirnhofer L, Lamprecht B, Vollmer WM, et al. COPD prevalence in Salzburg, Austria: results from the Burden of Obstructive Lung Disease (BOLD) study. Chest. 2007;131(1):29–36. doi:10.1378/chest.06-0365
19. Biener AI, Decker SL, Rohde F. Prevalence and treatment of Chronic Obstructive Pulmonary Disease (COPD) in the United States. JAMA. 2019;322(7):602. doi:10.1001/jama.2019.10241
20. Pirracchio R, Resche-Rigon M, Chevret S. Evaluation of the propensity score methods for estimating marginal odds ratios in case of small sample size. BMC Med Res Methodol. 2012;12:70. doi:10.1186/1471-2288-12-70
21. Efird JT, Griffin W, O’Neal WT, et al. Long-term survival after cardiac surgery in patients with chronic obstructive pulmonary disease. Am J Crit Care. 2016;25(3):266–276. doi:10.4037/ajcc2016119
22. Manganas H, Lacasse Y, Bourgeois S, Perron J, Dagenais F, Maltais F. Postoperative outcome after coronary artery bypass grafting in chronic obstructive pulmonary disease. Can Respir J. 2007;14(1):19–24. doi:10.1155/2007/378963
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.