Back to Journals » OncoTargets and Therapy » Volume 10
Association between clinicopathological features and survival in patients with primary and paired metastatic colorectal cancer and KRAS mutation
Authors Pang X, Li Q, Ma Z, Shi Y, Ma Y , Li X, Cui W, Zhang W
Received 25 January 2017
Accepted for publication 31 March 2017
Published 19 May 2017 Volume 2017:10 Pages 2645—2654
DOI https://doi.org/10.2147/OTT.S133203
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr William C. Cho
Xue-Lian Pang,* Qiao-Xin Li,* Zhi-Ping Ma, Yi Shi, Yu-Qing Ma, Xin-Xia Li, Wen-Li Cui, Wei Zhang
Department of Pathology, The First Affiliated Hospital of Xinjiang Medical University, Urumqi, People’s Republic of China
*These authors contributed equally to this work
Abstract: The KRAS gene mutation is involved in several types of tumors. However, the potential role of the KRAS mutation in human primary and paired metastatic colorectal cancer (CRC) among different nationalities is poorly understood. In the present study, we assessed the relationship between KRAS mutation status and overall survival (OS) and disease-free survival (DFS) in 230 patients with primary and paired metastatic CRC. The KRAS mutation rate in primary CRC tissue was 43.0% (99/230), which was higher than in paired metastatic CRC, which was 31.9% (23/72; P<0.001). Clinicopathologically, the KRAS gene mutation rate was higher in tumors that had infiltrated more deeply (T3, T4) and in lymph node (LN) metastases (N1/N2) (P=0.029 and P=0.010, respectively). The KRAS gene status did not differ between the Han and Uyghur nationalities in both primary and metastatic CRC. In 72 paired cases, the KRAS mutation rate in primary CRC was significantly higher than in metastatic CRC (P<0.001) and in metastatic CRC that had infiltrated more deeply (T3, T4) (P=0.034). In the metastatic cases, the KRAS gene mutation rate was higher in patients aged over 65 years (P=0.035). Specifically, KRAS mutation was correlated with a poorer OS and DFS (P=0.004 and P=0.029, respectively). In our study, 35 patients with wild-type KRAS who received cetuximab targeted therapy had a better DFS than patients with mutant KRAS (P=0.029). The results of the current study demonstrate that the KRAS status is significantly associated with infiltrating LN metastases and the TNM stage in primary CRC. In addition, the results show that the KRAS mutation is significantly more common in primary tumors than in paired metastatic CRC, and the KRAS mutation is correlated with a shorter OS and DFS, as patients with wild-type KRAS who received cetuximab experienced a longer DFS.
Keywords: CRC, KRAS, primary, metastatic, cetuximab, survival
Introduction
Colorectal cancer (CRC) is the most common tumor worldwide, and the World Health Organization (WHO) has declared that it is the third most frequent cancer in men and the second most frequent cancer in women. Epidemiological studies have found that the incidence rates of CRC correlate with geographic location. CRC is a heterogeneous disease evolving from the accumulation of genetic and epigenetic modifications,1 and KRAS homology from the mammalian ras gene family is considered a molecular switch that results in aberrant cell growth upon activation.2 Specifically, mutations within KRAS lead to the constitutive activation of the EGFR signaling pathway,3 and the cumulative survival rate of patients with wild-type KRAS is significantly higher than that of patients with mutations in this gene. A previous study has showed that the survival rate of patients with the wild-type KRAS gene receiving EGFR antibody therapy was significantly higher than that of patients harboring mutants.4 Moreover, a large phase III clinical study has showed that the codons 12 and 13 of exon 2 of the KRAS gene correlate with blocked EGFR gene monoclonal antibody status with cetuximab and panitumumab and that patients with wild-type KRAS benefit the most from EGFR antibody therapy.5
In recent years, reports on the heterogeneity and ethnic differences between individuals for the KRAS gene have been conflicting. Specifically, the KRAS gene has been shown to differ between primary cancers and metastases. Moreover, approximately 50% of patients harbor wild-type KRAS, but the efficacy of EGFR antibody treatment for these patients remains unclear, which may be related to the aforementioned heterogeneity in the KRAS gene between the primary tumor and metastatic lesions.6–8 In addition, KRAS mutations are less common in Asian populations than in black and Caucasian populations, but the KRAS gene status has not been delineated by nationality.9 The Xinjiang region in the People’s Republic of China is located in central Asia and is landlocked. The Uyghur people are the unique minority in Xinjiang, and we sought to identify possible differences in the KRAS gene status between Han and Uyghur people in that region. Furthermore, we investigated correlations between the KRAS gene status and the clinical characteristics and living conditions of patients with CRC.
Some studies have shown that KRAS mutations are associated with a poorer survival in patients with CRC,10 whereas other studies have reported that KRAS mutation does not have a prognostic value or any association with survival in patients with metachronous or synchronous metastatic CRC.11,12 We herein analyze the relationship between KRAS mutation and survival status in patients from Xinjiang with CRC.
Enrolled patients had histologically proven CRC and had not undergone previous chemotherapy, excluding adjuvant or targeted therapy. The following clinicopathological parameters were recorded: sex, age, ethnicity, differentiation, tumor infiltration, TNM stage, lymph node (LN) involvement, sites of metastasis, tumor location, KRAS mutation status in tumor tissue and chemotherapy regimen. All patients gave permission for the use of their serum and tumor tissue.
Materials and methods
Sampling of CRC cases
This study included 230 randomly selected patients with histologically proven CRC: 72 patients with primary CRC who had corresponding paired metastatic tissues, including 62 patients with LN metastases and 10 patients with distant metastases. The patients were chemotherapy-naïve, excluding adjuvant therapy, and were enrolled between March 2012 and July 2014. The study was approved by the Medical Ethics Committee of the First Affiliated Hospital of Xinjiang Medical University, and patients provided informed consent prior to surgery. The following variables were available for analysis: sex, age, ethnicity, differentiation, tumor infiltration, TNM stage, LN involvement, sites of metastasis and tumor location. The TNM classification was defined according to the 2010 WHO criteria. Inclusion criteria for patients with LN metastases were the following: the proportion of tumor should be 20%, and the tumor cells should be above 200. In this study, there were 83 cases who had LN metastases, but only about 72 cases met the requirements.
In this study, disease-free survival (DFS) was defined as the time from the first cetuximab or chemotherapy to death from any other cause. Overall survival (OS) was defined as the time from the first administration of cetuximab or chemotherapy to death from any cause.
Amplification-refractory mutation system (ARMS) analysis
The ARMS experiment was conducted on the European Molecular Genetics Quality Network quality certification platform. DNA was extracted from 5- to 8-μm-thick paraffin sections containing a representative portion of the tumor tissue (Qiagen DNA Mini Kit, 51304). The concentration of DNA was 20–50 ng/μL. Amplifications were performed using a 5-minute initial denaturation at 95°C, followed by 15 cycles of 25 seconds at 95°C, 20 seconds at 64°C, 20 seconds at 72°C, 31 seconds at 93°C, 35 seconds at 60°C and 20 seconds at 72°C. The Ya Kang Bo Gene mutation detection kit was used to analyze the PCR products in conjunction with the MxPro QPCR Software (Version 4.10). Sample channel fluorescein threshold cycle (Ct) values <28 were interpreted as positive (Figure 1).
  | Figure 1 (A) Internal control gene in HEX channel. (B) KRAS gene Wild-type in FAM channel. (C) KRAS gene mutant-type in FAM channel. (D) KRAS gene double mutant-type in FAM channel. |
Statistical analysis
All data were statistically analyzed using the Statistical Package for the Social Sciences, version 17.0 (SPSS17.0). The correlation between clinicopathological features and KRAS status was evaluated using a Chi-squared test. The Cox proportional hazards model was used for univariate and multivariate analyses to identify the independent prognostic factors for OS and DFS. OS and DFS were calculated with the Kaplan–Meier method, and differences in survival rates were analyzed with the log-rank test. Logistic regression models analyzed KRAS mutation-site predictors of OS and DFS. A P-value of <0.05 was considered to be significant.
Results
KRAS mutations in patients with CRC
In a total of 230 patients with CRC, the KRAS mutation rates were 42.6% (75/176) and 44.4% (24/54) for patients of Han and Uyghur descent, respectively. However, this difference was not significant. A total of 99 patients had the KRAS gene mutation, corresponding to a total mutation rate of 43.0% (99/230). Specifically, codon 12 was mutated in 84 of these patients (84.9%), whereas codon 13 was mutated in only 15 patients (15.2%). Most primary tumors had single mutations, and only 4 out of 99 tumors (4.0%) harbored a double mutation. The most common mutation site was G12D, which was mutated in 38.4% of tumors (38/99) (Figure 2). In a total of 122 patients with colon cancer, the KRAS mutation rates in the left and right sides were 44.0% (33/75) and 59.5% (22/37), respectively. However, the bilateral and transverse KRAS gene mutation rates did not significantly differ (Tables 1 and 2).
  | Figure 2 KRAS gene single mutation rate of codons 12 and 13 in primary and metastatic CRC. |
A comparison of patients having only a primary lesion with those having paired metastatic lesions showed that the KRAS gene mutation rate was higher in tumors that had infiltrated more deeply (T3, T4) and in LN metastases (N1/N2) and metastases (M1) (P<0.001) (Table 2). Among a total of 72 paired metastatic tissues, including 62 LN metastases and 10 liver or lung metastases, the KRAS mutation rates in the CRC tissues from the Han and Uyghur patients were 34.0% (17/50) and 27.3% (6/22), respectively, but this difference was not significant. All mutations were located at codon 12 (100.0%, 23/23), and the most common mutation site was G12D, which was mutated in 45.5% of all mutations (10/22). The mutation rate was 27.4% (17/62) in LN metastases and 60.0% (6/10) in non-metastatic LNs. Finally, the mutation rates were significantly higher in liver or lung metastases than in LN metastases (P=0.040) (Table 3).
Relationship between KRAS gene mutation and clinicopathological features
In the primary tumor, the KRAS gene mutation rate directly correlated with tumor infiltration (T3, T4) and LN metastasis (N1/N2) (47.8%, 76/159, P=0.029 and 54.2%, 45/83, P=0.010, respectively) but did not significantly correlate with gender, ethnicity, age, tumor differentiation, histological type and the presence of distant metastases. KRAS mutations were more common in individuals older than 65 years and were identified in 58.8% (13/28) (P=0.035) of patients with metastatic disease. Other clinical and pathological features did not correlate with KRAS status (Table 2).
A comparison of patients having only a primary lesion with those having paired metastatic lesions showed that the KRAS mutation rate was higher in tumors that had infiltrated more deeply (T3, T4) and in LN metastases (N1/N2) and metastases (M1) (P<0.001) (Table 2).
We also analyzed the relationship between codons 12 and 13 of the KRAS gene with relevant clinicopathological features and found that mutations in codon 12 were associated with advanced disease; mutations at codon 12 were identified in 84.8% of patients with advanced disease (84/99). Moreover, mutations in codon 13 were associated with poorly differentiated disease; they were identified in 66.7% of poorly differentiated tumors (10/15). Mutations in codon 12 were also associated with late TNM stage, which were identified in 46.4% of samples (39/84), whereas mutations in codon 13 were associated with early TNM stage, and were detected in 80.0% of tissues (12/15). The mutation rate of codon 12 was higher for LN metastases, accounting for 53.6% of all mutations (45/84), but did not include LN metastasis. The mutation rate of codon 13 was higher, accounting for 83.3% (13/15) (Table 3).
Comparison between primary and metastatic CRC
KRAS gene expression was not consistent in the 72 paired primary and metastatic tumors examined in this study. Specifically in the primary tumor, 36 primary tumors expressed mutant KRAS, and the other 36 expressed wild-type KRAS; in the paired metastases, 23 samples expressed mutant KRAS, whereas 49 expressed wild-type KRAS. Thirteen primary tumors expressed mutant KRAS but the paired metastases expressed wild-type KRAS. The mutation rate was significantly higher in the primary tumor than in the metastasis samples (P<0.001), and primary tumors and paired metastases showed the same KRAS expression (Tables 3 and 4).
KRAS gene status and patient survival analysis
The 30-month survival of the entire patient cohort is shown in Figure 3. Of the total number of patients, 156 (77.8%) were alive and 110 were alive and disease-free, and mutant KRAS was associated with a poor OS and DFS (P=0.004 and P=0.010, respectively). Moreover, 113 patients received chemotherapy, and OS and DFS were longer for patients with wild-type KRAS (P=0.014 and P=0.007, respectively). Among all 35 patients with wild-type KRAS and who received cetuximab targeting therapy, 2 patients relapsed and died within 6–10 months, and 5 patients were lost to follow-up. The remaining patients survived, and the targeting therapy improved DFS (P=0.029) (Figure 3). Based on the univariate Cox proportional hazards analysis results (Table 5), metastasis and the KRAS mutation correlated with a poor OS (P=0.037 and P=0.004). Furthermore, infiltrating tumors (T3/T4) and metastasis also correlated with a poor DFS (P=0.006 and P=0.001, respectively). However, we did not find a worse OS and DFS in patients with LN metastases than those without.
Logistic regression models found that G12V and G12D (odds ratio [OR] =6.049, P=0.001 and OR =4.853, P=0.001, respectively) were associated with OS, and G12V (OR =4.517, P=0.003) with DFS (Table 6).
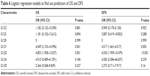  | Table 6 Logistic regression models to find out predictors of OS and DFS |
Discussion
KRAS mutations are important in the carcinogenesis of CRC and play a definitive role in the efficacy of anti-EGFR therapy.9,13 In recent years, the association between the KRAS gene and CRC has been widely studied, and these studies showed that 35%–40% of CRC tumors harbor mutant KRAS.9,14 The KRAS gene mutation occurs in codons 12 and 13, and mutations in codon 12 comprise 80% of all KRAS mutations. Our study showed that 43.0% of primary CRC tumors harbored mutants, which corroborated other studies. However, only 32.7% of metastatic tumors harbored mutant KRAS, and this incidence is lower than that found in a previous study. KRAS gene mutations often occur in codons 12 and 13; a single mutation of G12D is the most common mutation at codon 12. Specifically, Kodaz et al found that the G12D mutation comprised 42.4% of all mutations, with a multiple mutation rate of only 1.1%.15 Molecular analyses of the primary tumor in patients with metastases have been considered effective in the past because metastases are thought to maintain the biological features of the primary lesions. Specifically, primary and metastatic lesions have been shown to share numerous morphological and immunohistochemical features, allowing pathologists to obtain a diagnosis, and proliferation rates are generally similar in primitive and secondary neoplastic lesions.16
Yamauchi et al found that rectal cancer, a type of CRC, is more prone to KRAS mutations.17 However, the KRAS gene status in our study did not differ between tumors of the colon and rectum, and previous studies examining the KRAS gene mutation status in the colon have also reported inconsistencies. For example, Bleeker et al found that the KRAS mutation rate is higher in the right side of the colon, whereas Zulhabri et al reported a higher rate in the left side. In this study, the KRAS status did not differ between the left, right and transverse colon. In Bleeker et al’s study of 55 colon cancer specimens, the KRAS gene mutation rates in the left and right colon were 10% (3/29) and 38% (10/26), respectively, whereas in Zulhabri et al’s study of 70 colon cancer specimens, these rates were 36.8% (7/19) and 13.7% (7/51), respectively.18,19 In our study of 122 colon cancer specimens, the KRAS gene mutation rates in the left and right sides were 43.5% (27/62) and 60.0% (18/30), respectively. However, the KRAS gene mutation rates did not significantly differ between the bilateral and transverse colon. All previous studies examined a smaller sample, and the patients were from different geographical regions. Conversely, we collected large samples for multivariate analyses to clearly correlate the KRAS gene mutation status with the tumor site.
Many studies have examined the relationship between KRAS gene status and the clinicopathological features of patients with CRC. Specifically, the KRAS gene status has been correlated with patient age: the mutation rate is high in patients younger than 40 years. However, the KRAS gene status of primary CRC tumors did not correlate with age in this study. Nevertheless, KRAS mutations were more common in LN metastases, consistent with the findings of Velho et al.20 Tumor infiltration also directly correlated with the KRAS mutation rate, but previous studies reported that these parameters did not correlate.21 Specifically, previous studies reported that KRAS mutation did not correlate with the depth of invasion and LN metastasis in CRC.15 In our study, patients older than 65 years had a high KRAS gene mutation rate, and Kadowaki et al found that survival was low in patients aged older than 65 years.22 Thus, KRAS mutation is associated with a poor prognosis. In this study, the correlations between KRAS gene mutation status and clinicopathological features were not consistent between primary and metastatic CRC tumors, which may be related to tumor heterogeneity. However, limited amounts of tissue were available for some metastases examined in this study, which may have biased our data.
In our study, the KRAS gene mutation rate differed between paired primary tumors and metastases. Specifically, the mutation rates were higher in primary tumors than in metastases, and metastases that harbored KRAS mutations were associated with primary tumors that also harbored this mutation, whereas primary tumors harboring this mutation were not necessarily associated with mutant metastases. This finding may be due to heterogeneity within the primary tumor or the acquisition of mutations during the process of metastasis. However, we examined fewer metastatic tumor cells than primary tumor cells, which may have resulted in false negatives. Many current studies have identified KRAS heterogeneity between primary tumors and metastases. For example, Siyar Ekinci et al found that the KRAS mutation rate is inconsistent between liver or lung metastases and primary tumors; both the primary tumor mutant and paired metastases wild-type also have primary tumor wild-type and paired metastases mutant.21,23 Moreover, KRAS gene consistency has been reported between primary tumors and metastases, especially non-metastatic LNs.16 In our study, the KRAS gene status was not consistent between primary tumors and LN metastases but identical between primary tumors and liver or lung metastases. Samples of LN metastases are usually small and contain few tumor cells, which may cause false-negative results. However, the LN metastasis specimens in our study were subjected to rigorous screening, and samples containing an insufficient number of tumor cells were excluded. Therefore, the possibility of a false negative is relatively small. Nevertheless, lymphocytes may affect the expression of KRAS gene in the ras signaling pathway,24 which suggests that an autoimmune lymphocyte response may inhibit KRAS gene mutation.
Previous studies have found that KRAS mutations were associated with a poorer survival. In a Japanese study by Kadowaki et al, KRAS and BRAF mutations were associated with a shorter survival,22 whereas another Japanese study revealed that the prognostic impact of KRAS mutations on recurrence-free survival was limited in patients with stage II CRC, and KRAS mutations were not associated with OS.25 Conversely, our analysis showed that the KRAS status affects OS and DFS in patients with CRC: KRAS mutations were associated with a shorter OS and DFS compared with wild-type KRAS. These results suggest that constitutive KRAS mutations may be associated with clinical prognosis in CRC. In our study, cetuximab therapy prolonged DFS but not OS in patients harboring wild-type KRAS. However, only 35 patients received the targeted therapy in our study, and 10 patients were lost to follow-up. Therefore, a larger sample is necessary to confirm these findings. Ocvirk et al also found that progression-free survival was significantly longer for patients harboring wild-type KRAS tumors than patients harboring mutant KRAS tumors.10
In addition, survival (OS and DFS) did not differ between groups when tumors were stratified by KRAS mutation type, that is, mutations in codons 12 and 13, which agrees with findings reported by Huang et al.11 However, the number of samples was limited in our study, and few samples harbored mutations in codon 13. Thus, additional research with larger samples is needed to confirm these findings. In our study, G12V and G12D were associated with a poor prognosis. Bournet et al found that KRAS G12D was an independent predictor of a worse prognosis within the entire series and in the subgroup of patients who received chemotherapy for advanced pancreatic adenocarcinoma, but G12V had no obvious effect.26
Conclusion
KRAS mutations were associated with shorter DFS times and more rapid disease progression in patients from Xinjiang, People’s Republic of China. Targeted therapy was able to prolong survival for these patients, but this effect was not associated with KRAS in Uyghur and Han patients.
Acknowledgments
This work was supported by the National Natural Science Foundation of China (No 81560035), The Xinjiang Uygur Autonomous Region Nature Science Foundation (No 2014211C032), Science and Technology Talents Training Project of Xinjiang Uyghur Autonomous Region (qn2015bs011) and the Post-doctor Project of Xinjiang Medical University.
Disclosure
The authors report no conflicts of interest in this work.
References
Li W, Qiu T, Ling Y, Guo L, Li L, Ying J. Molecular pathological epidemiology of colorectal cancer in Chinese patients with KRAS and BRAF mutations. Oncotarget. 2015;6(37):39607–39613. | ||
Fernández-Medarde A, Santos E. Ras in cancer and developmental diseases. Genes Cancer. 2011;2(3):344–358. | ||
Diersch S, Wirth M, Schneeweis C, et al. Kras(G12D) induces EGFR-MYC cross signaling in murine primary pancreatic ductal epithelial cells. Oncogene. 2016;35(29):3880–3886. | ||
Zocche DM, Ramirez C, Fontao FM, Costa LD, Redal MA. Global impact of KRAS mutation patterns in FOLFOX treated metastatic colorectal cancer. Front Genet. 2015;6:116. | ||
Sugaya A, Moriwaki T, Tajima D, et al. [A retrospective analysis of cetuximab or panitumumab monotherapy for KRAS wild-type metastatic colorectal cancer in clinical practice]. Gan To Kagaku Ryoho. 2015;42(2):189–193. Japanese [with English abstract]. | ||
Westwood M, van Asselt T, Ramaekers B, et al. KRAS mutation testing of tumours in adults with metastatic colorectal cancer: a systematic review and cost-effectiveness analysis. Health Technol Assess. 2014;18(62):1–132. | ||
Vignot S, Lefebvre C, Frampton GM, et al. Comparative analysis of primary tumour and matched metastases in colorectal cancer patients: evaluation of concordance between genomic and transcriptional profiles. Eur J Cancer. 2015;51(7):791–799. | ||
Vakiani E, Janakiraman M, Shen R, et al. Comparative genomic analysis of primary versus metastatic colorectal carcinomas. J Clin Oncol. 2015;30(24):2956–2962. | ||
Li W, Qiu T, Zhi W, et al. Colorectal carcinomas with KRAS codon 12 mutation are associated with more advanced tumor stages. BMC Cancer. 2015;15:340. | ||
Ocvirk J, Brodowicz T, Wrba F, et al. Cetuximab plus FOLFOX6 or FOLFIRI in metastatic colorectal cancer: CECOG trial. World J Gastroenterol. 2010;16(25):3133–3143. | ||
Huang CW, Tsai HL, Chen YT, et al. The prognostic values of EGFR expression and KRAS mutation in patients with synchronous or metachronous metastatic colorectal cancer. BMC Cancer. 2013;13:599. | ||
Roth AD, Tejpar S, Delorenzi M, et al. Prognostic role of KRAS and BRAF in stage II and III resected colon cancer: results of the translational study on the PETACC-3, EORTC 40993, SAKK 60-00 trial. J Clin Oncol. 2010;28(3):466–474. | ||
Bazan V, Migliavacca M, Zanna I, et al. Specific codon 13 K-ras mutations are predictive of clinical outcome in colorectal cancer patients, whereas codon 12 K-ras mutations are associated with mucinous histotype. Ann Oncol. 2002;13(9):1438–1446. | ||
Zhang K, Xu J, Yan L, Liu X, Xu F, Liu Y. [Detection of KRAS, NRAS and BRAF gene mutations in colorectal carcinoma]. Zhonghua Bing Li Xue Za Zhi. 2015;44(4):254–257. Chinese [with English abstract]. | ||
Kodaz H, Hacibekiroglu I, Erdogan B, et al. Association between specific KRAS mutations and the clinicopathological characteristics of colorectal tumors. Mol Clin Oncol. 2015;3(1):179–184. | ||
Paliogiannis P, Cossu A, Tanda F, Palmieri G, Palomba G. KRAS mutational concordance between primary and metastatic colorectal adenocarcinoma. Oncol Lett. 2014;8(4):1422–1426. | ||
Yamauchi M, Morikawa T, Kuchiba A, et al. Assessment of colorectal cancer molecular features along bowel subsites challenges the conception of distinct dichotomy of proximal versus distal colorectum. Gut. 2012;61(6):847–854. | ||
Bleeker WA, Hayes VM, Karrenbeld A, et al. Impact of KRAS and TP53 mutations on survival in patients with left- and right-sided Dukes’ C colon cancer. Am J Gastroenterol. 2000;95(10):2953–2957. | ||
Zulhabri O, Rahman J, Ismail S, Isa MR, Wan Zurinah WN. Predominance of G to A codon 12 mutation K-ras gene in Dukes’ B colorectal cancer. Singapore Med J. 2012;53(1):26–31. | ||
Velho S, Oliveira C, Seruca R. KRAS mutations and anti-epidermal growth factor receptor therapy in colorectal cancer with lymph node metastases. J Clin Oncol. 2009;27:158–159. | ||
Kleist B, Kempa M, Novy M, et al. Comparison of neuroendocrine differentiation and KRAS/NRAS/BRAF/PIK3CA/TP53 mutation status in primary and metastatic colorectal cancer. Int J Clin Exp Pathol. 2014;7(9):5927–5939. | ||
Kadowaki S, Kakuta M, Takahashi S, et al. Prognostic value of KRAS and BRAF mutations in curatively resected colorectal cancer. World J Gastroenterol. 2015;21(4):1275–1283. | ||
Siyar Ekinci A, Demirci U, Cakmak Oksuzoglu B, et al. KRAS discordance between primary and metastatic tumor in patients with metastatic colorectal carcinoma. J BUON. 2015;20(1):128–135. | ||
El-Jawhari JJ, El-Sherbiny YM, Scott GB, et al. Blocking oncogenic RAS enhances tumour cell surface MHC class I expression but does not alter susceptibility to cytotoxic lymphocytes. Mol Immunol. 2014;58(2):160–168. | ||
Nakanishi R, Harada J, Tuul M, et al. Prognostic relevance of KRAS and BRAF mutations in Japanese patients with colorectal cancer. Int J Clin Oncol. 2013;18(6):1042–1048. | ||
Bournet B, Muscari F, Buscail C, et al. KRAS G12D mutation subtype is a prognostic factor for advanced pancreatic adenocarcinoma. Clin Transl Gastroenterol. 2016;7:e157. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.






