Back to Journals » Journal of Multidisciplinary Healthcare » Volume 14
Association Between Caregivers’ Burden and Neuropsychiatric Symptoms in Female Patients with Alzheimer’s Disease with Varying Dementia Severity
Authors Chen YA, Chang CC , Wang WF, Lin YS, Jhang KM, Lo TY, Wu HH
Received 22 December 2020
Accepted for publication 11 March 2021
Published 28 April 2021 Volume 2021:14 Pages 929—940
DOI https://doi.org/10.2147/JMDH.S298196
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Yu-An Chen,1,* Cheng-Chen Chang,1,2,* Wen-Fu Wang,3,4,* Ya-Sian Lin,5 Kai-Ming Jhang,3 Tzu-Ying Lo,5 Hsin-Hung Wu5– 7
1Department of Psychiatry, Changhua Christian Hospital, Changhua, Taiwan; 2School of Medicine, Chung Shan Medical University, Taichung City, Taiwan; 3Department of Neurology, Changhua Christian Hospital, Changhua, Taiwan; 4Department of Holistic Wellness, Ming Dao University, Changhua, Taiwan; 5Department of Business Administration, National Changhua University of Education, Changhua, Taiwan; 6Department of M-Commerce and Multimedia Applications, Asia University, Taichung City, Taiwan; 7Faculty of Education, State University of Malang, Malang, East Java, Indonesia
*These authors contributed equally to this work
Correspondence: Hsin-Hung Wu
National Changhua University of Education, No. 2 Shida Road, Changhua City, 500, Taiwan
Tel +886 4 7232105 ext. 7412
Fax +886 4-7211292
Email [email protected]
Purpose: This study examined the attributes causing higher burdens for caregivers caring for female patients with Alzheimer’s disease by analyzing a combination of various variables, including demographic data, dementia severity, and neuropsychiatric symptoms.
Patients and Methods: This study included 99 female patients with Alzheimer’s disease who were cared for by the dementia collaborative care team at Changhua Christian Hospital, Taiwan. Neuropsychiatric symptoms used in this study included affections (9 types), behavior symptoms (9 symptoms), and psychological symptoms (3 symptoms). The Apriori algorithm was employed to identify association rules that reveal the relationships among demographic data, dementia severity, neuropsychiatric symptoms, and caregivers’ burden.
Results: A total of 185 rules were determined, including 51 rules with little or no burden, 108 rules with mild to moderate burden, and 26 rules with moderate to severe burden. The major findings are as follows. Neuropsychiatric symptoms were associated with varying degrees of caregivers’ burden among female patients aged 75 to 84 years with mild dementia. Crying spells and aggression were specifically associated with a moderate to severe burden. Delusion was associated with a mild to moderate and moderate to severe burden. Dysthymia and depression were associated with little or no burden to moderate to severe burden.
Conclusion: Clinicians can provide early interventions to reduce the burden of caregivers caring for female patients with Alzheimer’s disease and can refer caregivers for timely assistance to reduce their burden.
Keywords: Alzheimer’s disease, female patients, female patients with Alzheimer’s disease, neuropsychiatric symptom, Apriori algorithm, caregiving burden
Introduction
The global incidence of dementia is increasing annually, and this trend is also observed in Taiwan. According to the epidemiology data from the Ministry of the Interior in 2018, the prevalence of dementia in individuals aged 65 years and older was approximately 7.86% in Taiwan, and the dementia population in Taiwan is expected to grow at an average rate of 36 people per day in the ensuring 47 years. Alzheimer’s disease (AD) is the most common cause of dementia, and more women than men have Alzheimer’s or other dementias.1,2 In addition to cognitive deficit, neuropsychiatric symptoms (NPS) are commonly observed in patients with AD. Notably, NPS include agitation, irritability, depression, apathy, delusions, hallucinations, and sleep impairment. A previous review indicated that NPS are predictors of caregivers’ burden regardless of dementia diagnosis, and the effects are manifested by disruptive behaviors (eg, agitation, aggression, disinhibition), delusions, and mood disturbance.3 Moreover, another review concluded that irritability, agitation, sleep disturbances, anxiety, apathy, and delusion affect caregivers’ burden the most.4 Furthermore, a 3-year longitudinal study observed that patient characteristics, including greater NPS, lower functional ability, fewer medications, lack of driving ability, and female caregivers, were associated with a greater burden.5
To date, most researches have focused on caregiving burden related to gender differences among caregivers of patients with AD, the burden of caregivers caring exclusively for female patients with AD has scarcely been discussed. The prevalence of AD is higher in females than in males, and several biological underpinnings regarding gender differences were established, such as variances in age-related sex hormone reduction, genetic risks, and age-related declines in brain volumes.6 In addition, the gender-based differences related to the clinical and pathological manifestations of the disease have been described. Previous studies have reported that females with AD were more likely to exhibit a broader range of NPS than males with AD.7,8 One observational study investigating outpatients with AD observed reclusiveness and emotional lability to be related to the female gender, while apathy and vegetative signs were highly related to the male gender.9 Moreover, evidence has revealed that women with AD experience significantly greater cognitive impairments across a wide range of cognitive domains, including both visual and verbal processing, as well as semantic and episodic memory.10
Furthermore, few studies have provided a comprehensive viewpoint by combining various variables, such as demographic data, dementia severity, and NPS, to identify the attributes possibly related to a higher caregiving burden.5,11–15 Nevertheless, grouping care needs for particular conditions, such as the severity or subtype of dementia, would facilitate more efficient and holistic care.
Therefore, this study aims to identify the attributes that could result in the severe caregiving burden from a comprehensive viewpoint of female patients with Alzheimer’s disease and their caregivers by applying the Apriori algorithm. The Apriori algorithm is one of the data mining approaches to identify association rules that effectively reveal relationships among different items from a large database.16
Patients and Methods
This study enrolled 99 female patients diagnosed with Alzheimer’s disease per the criteria of the National Institute on Aging-Alzheimer’s Association17,18 from January 2014 to May 2018 at memory clinic of Changhua Christian Hospital, Changhua, Taiwan. The clinical trial was approved by the Institutional Review Board of Changhua Christian Hospital (CCH IRB 160165). The need for informed consent was waived by the Institutional Review Board of Changhua Christian Hospital because the design of the study was a retrospective data analysis. All data were recorded in the electronic medical chart with the highest confidentiality and compliance with the Declaration of Helsinki. All data needed in the present study were extracted by our information technology department after deleting any personalized information. The demographic variables including age, clinical dementia rating (CDR), and the caregiving burden evaluated by Zarit’s Burden Interview (ZBI) are summarized in Table 1. A majority of the female patients with Alzheimer’s disease aged 75–84 years (60.6%) who had mild dementia (43.4%) followed by very mild dementia (39.4%). The majority of the caregiving burden were mild to moderate burden (48.5%).
 |
Table 1 Information of Female Patients with Alzheimer’s Disease |
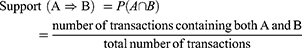
The Apriori algorithm has been proven to be a very useful approach to discover the previously unknown relationships in data sets by finding rules and associations between any of the attributes.16,19 Each rule is generated through establishing support, confidence, and lift. The definitions are as follows.16,19,20 The support of A ⇒ B is evaluated by calculating the percentage of transactions in the database containing both A and B:
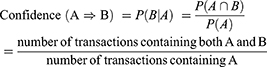
The confidence of A ⇒ B is to evaluate the accuracy of the rule based on the computation of the percentage of transactions in the database containing A and also containing B simultaneously:
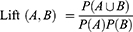
Lift measures whether A and B are independent or dependent and correlated events as shown in Equation (3). If a rule has a lift of one, A and B are independent and no rule will be generated containing either event. If a rule has a lift greater than one, A and B are dependent and correlated positively. In practice, Larose21 pointed out that analysts prefer rules with either high support or high confidence, and usually both. In fact, strong rules will be found when certain minimum support and confidence conditions have been met.
The notations of data types are defined as follows. The notations of 1, 2, 3, and 4 represent the age groups of less than 65, 65–74, 75–84, and 85 years old and above, respectively, for female patients with AD. Very mild dementia, mild dementia, moderate dementia, and severe dementia of CDR are defined as 0, 1, 2, and 3, respectively. Affections include crying spells, dysthymia, depression, anxiety, worry, anger, irritability, emotional liability, and apathy. Behavior symptoms consist of agitation, akathisia, wandering, curse, shadowing, aggression, akinesia, sleep change, and aberrant motor behavior (stereotype). Psychological symptoms are composed of delusion, hallucination, and misidentification. The notation for each affection, behavior symptom, or psychological symptom is 1 or 0. If a patient has a particular affection, behavior symptom, or psychological symptom, a value of 1 is assigned. If not, a value of zero is applied. For the caregiving burden, little or no burden, mild to moderate burden, moderate to severe burden, and severe burden are classified into four types of variables, namely Zarit 1, Zarit 2, Zarit 3, and Zarit 4. If a caregiving burden belongs to little or no burden, a value of 1 is assigned to Zarit 1, while Zarit 2, Zarit 3, and Zarit 4 will be given a value of 0.
The Apriori algorithm in the IBM SPSS Modeler 18 was employed in this study. The input variables for antecedents were age, CDR, affections (nine variables), behavior symptoms (nine variables), and psychological symptoms (three variables). The input variable for consequents was the caregiving burden. This study intended to find how specific combinations of the patients’ age, CDR, affections, behavior symptoms, and psychological symptoms result in different levels of caregivers’ burden for female patients with AD. Minimum support, minimum confidence, and lift were set to 2%, 90%, and greater than one, respectively.
Results
A total of 185 rules were identified by the Apriori algorithm (Table 2 lists three rules). Antecedents represent “the reasons” to result in the consequent. That is, antecedents appearing in rules are considered to be critical variables. Besides, if there are two or more antecedents in a rule, these antecedents should be incurred simultaneously. For instance, Rule 1 indicates that a female patient with AD whose age is 75–84 years has anxiety would result in a moderate to severe caregiving burden. To further categorize the rules effectively, 185 rules were divided into three categories in terms of little or no burden (Zarit 1) with 51 rules, mild to moderate burden (Zarit 2) with 108 rules, and moderate to severe burden (Zarit 3) with 26 rules. Because some rules have similarities, it is better to present the rules into the generalized rules in practice. In addition, this study focused on mild to moderate burden (Table 3) and moderate to severe burden (Table 4).
 |
Table 2 Partial Rules of 185 Rules |
 |
Table 3 Five Generalized Rules with Mild to Moderate Burden (Zarit 2) |
 |
Table 4 Ten Generalized Rules with Moderate to Severe Burden (Zarit 3) |
In Table 3, five generalized rules were found for caregivers with a mild to moderate burden. The first generalized rule depicts that a mild to moderate caregiving burden comes from female patients with mild AD who have dysthymia and might combine some major symptoms from affections and psychological symptoms. The second generalized rule indicates female patients with AD aged 75–84 years with major symptoms from affections followed by psychological symptoms. Third generalized rule shows female patients with AD aged 85 years and older with a combination of hallucination and emotional liability, depression and delusion, or both. In the fourth generalized rule, a mild to moderate caregiving burden comes from female patients with mild AD aged 75–84 years who have depression and delusion simultaneously. The fifth generalized rule has only one rule indicating female patients with mild AD aged 85 years and older with depression resulting in a mild to moderate caregiving burden.
Table 4 summarizes ten generalized rules for moderate to severe caregiving burden (Zarit 3) based on 26 rules. The first generalized rule with four rules reveals that female patients with mild AD who have akinesia and hallucination simultaneously might present with delusion, dysthymia or both. The second generalized rule indicates the moderate to severe burden results from female patients with mild AD together with akinesia and delusion. The third generalized rule depicts female patients with AD aged 75–84 years who have major symptoms from affections (anxiety, anger, and crying spells) followed by aggression and delusion. There is a single rule in the fourth generalized rule indicating a moderate to severe burden because of female patients with AD aged 85 years and older who have akinesia and dysthymia simultaneously. The fifth generalized rule depicts female patients with mild AD aged 75–84 years who have aggression, crying spells, aggression and anger, or crying spells and delusion. A single rule in the sixth generalized rule describes female patients with mild AD together with crying spells and delusion would result in a moderate to severe caregiving burden. Female patients with AD who have akinesia and crying spells simultaneously in the seventh generalized rule would result in a moderate to severe burden. The eighth generalized rule identifies female patients with AD who have akinesia and hallucination and might present a combination of delusion, dysthymia, or both. The ninth generalized rule shows female patients with AD who have both akinesia and delusion. The tenth generalized rule depicts female patients with AD who have both crying spells and delusion.
To further summarize the rules found in this study, Table 5 presents three types of caregiving burdens based on the 185 rules for female patients with mild AD (CDR = 1). A notation (√) indicates the relationships between symptoms and the caregivers’ burden. Female patients who have several affective symptoms (including dysthymia, depression, anger, irritability, and emotional liability), sleep change, and two psychotic symptoms (ie, delusion and hallucination) would result in a mild to moderate burden for caregivers. In addition, a moderate to severe burden might come from three affective symptoms (including crying spells, dysthymia, and anger), two behavioral symptoms (ie, aggression and akinesia), and two psychotic symptoms (ie, delusion and hallucination). That is, an increase in a caregivers’ burden might come from crying spells, aggression, and akinesia.
 |
Table 5 Caregivers’ Burden for Female Patients with Mild AD |
Table 6 summarizes the relationships between symptoms and caregivers’ burdens for female patients with AD aged 75–84 years. A mild to moderate burden for caregivers might come from four major affective symptoms (ie, dysthymia, depression, anger, and irritability), curse (behavioral symptom), and two psychotic symptoms (ie, delusion and hallucination). Furthermore, a moderate to severe burden for caregivers might come from three major affective symptoms (including crying spells, anxiety, and anger), aggression (behavioral symptom), and delusion and hallucination (psychotic symptoms). That is, the symptoms of crying spells, anxiety, and aggression could be the indicators to increase a caregivers’ burden for female patients with AD aged 75–84 years.
 |
Table 6 Caregivers’ Burden for Female Patients with AD Aged 75–84 Years |
By combining age = 3 and CDR = 1, Table 7 provides the relationships between symptoms and caregivers’ burdens. A mild to moderate burden for caregivers might come from two affective symptoms (ie, dysthymia and depression) and delusion (psychotic symptom). Moreover, a moderate to severe burden for caregivers would result from two affective symptoms (ie, crying spells and anger), aggression (behavioral symptom), and delusion (psychotic symptom). The symptoms of crying spells, anger, and aggression could be the indicators to increase a caregivers’ burden for female patients with mild AD aged 75–84 years.
 |
Table 7 Caregivers’ Burden for Female Patients with Mild AD Aged 75–84 Years |
Discussion
To the best of our knowledge, this is the first study applying the Apriori algorithm to investigate the association between caregivers’ burdens and female patients with AD. The major findings are as follows: (1) NPS were associated with the caregivers’ burden to varying degrees among female patients aged 75–84 years with mild dementia (CDR=1); (2) crying spells and aggression were specifically associated with a moderate to severe burden; (3) delusion was associated with a mild to moderate and moderate to severe burden; and (4) dysthymia and depression were associated with little or no burden to moderate to severe burden.
When comparing the results of Tables 5–Table 7, we found that crying spells, dysthymia, anger, aggression, akinesia, delusion, and hallucination were associated with a moderate to severe caregivers’ burden for female patients with mild AD (CDR = 1). In female patients aged 75–84 years, crying spells, anxiety, anger, aggression, delusion, and hallucination were associated with a moderate to severe caregiving burden regardless of dementia severity. Moreover, crying spells, anxiety, and aggression were the indicators of a higher caregiving burden. If we take into consideration the dementia severity (CDR=1), crying spells, anger, aggression, and delusion were associated with a moderate to severe burden, and crying spells, anger, and aggression were the indicators of a higher caregiving burden.
A previous review indicated that NPS in patients with AD, such as anxiety, agitation, disinhibition, and aggressive behaviors, were more closely related to the caregivers’ burden,22 but there is a lack of studies investigating how dementia stages and patients’ ages might add to a caregivers’ burden other than NPS. Some studies have revealed that dementia stages and ages were associated with NPS in patients with AD. Two cross-sectional studies have observed significant increases in neuropsychiatric inventory (NPI) total scores with dementia stages in patients with AD.23,24 Regarding symptom manifestations, one study demonstrated that agitation, aggression, and psychosis were more frequent in late stages of the patients with AD.25 However, another study revealed that patients with mild AD (CDR = 0 or 1 per our study’s notations) had delusion, hallucination, agitation, dysphoria, anxiety, apathy, and irritability as frequently as patients with moderate or severe AD (CDR = 2 or 3 per our study’s notations). It is suggested that psychosis and emotional symptoms are crucial in patients with mild AD as well as in those with moderate or severe AD.5 Regarding the association between age and NPS in patients with AD, age could affect the prevalence of aggression, disinhibition, irritability, euphoria, delusion, depression, and anxiety.26 Based on the aforementioned findings, patients with mild AD might start to develop NPS, which might cause caregivers’ burden. Because patients with mild AD (CDR=1) and those aged 75–84 years account for the majority of our subjects, the association between NPS of this population group and the corresponding caregivers’ burden was more significant.
In this study, crying spells and aggression were specifically associated with a moderate to severe burden. Notably, several reasons can cause crying spells in patients with AD, including depression, fear, psychosis, and physical discomfort. However, limited communication abilities make it difficult for caregivers to identify the definite cause, which might delay proper management of these issues, causing a higher caregivers’ burden. Anger and aggression were the most problematic and disruptive symptoms in patients with AD. Moreover, a recent research also suggested that caregivers’ distress was more closely connected to aggression than other key symptoms of patients with AD.27 Our results revealed that delusion and hallucination were generally associated with a mild to moderate and moderate to severe burden. Previous studies have reported that high levels of caregivers’ burden were associated with psychotic symptoms, and that psychotic symptoms also predicted institutionalization.28,29 In addition, Alzheimer’s disease with psychosis was associated with greater functional impairments,30 worsened general health,31 and increased mortality.32
Nonetheless, our study has several limitations. First, it was a cross-sectional study; therefore, we could not reach conclusions regarding the causality. Second, our study had a relatively small sample of size after excluding incomplete data. Third, these results might not be generalized to populations in other settings, such as primary care or residential care. Fourth, we evaluated NPS using the questionnaire instead of NPI, which is the most widely used instrument for assessing NPS. Finally, we did not measure other factors that would affect caregivers’ burden, such as physical and psychiatric comorbidities, daily functional status, socioeconomic conditions, and demographic information of caregivers. Despite these limitations, it is worth noting that our study focused on female patients with AD. As was pointed out in the introduction, females were more likely to exhibit a broader range of NPS and greater cognitive impairments than male patients with AD. This study implied that clinicians should provide early interventions to reduce the burden of caregivers caring for female patients with mild AD and should refer the caregivers for timely assistance to reduce their burden.
Conclusion
This study revealed that the caregivers’ burden was associated with specific neuropsychiatric symptoms for female patients with AD aged 75 to 84 years with mild dementia, and crying spells, anger, and aggression were associated more with a higher level of burden. Delusion was associated with a mild to moderate and moderate to severe burden. Dysthymia and depression were associated with little or no burden to mild to moderate burden. Grouping care needs according to the patients’ ages and dementia severity may allow for more efficient and holistic care to be provided as well as provide timely assistance for caregivers to reduce their burden. Multidimensional interventions, including skills training in problem-solving to manage dementia-related symptoms, such as NPS and cognitive impairment, resolving pre-existing relational problems between caregivers and patients, enhancing social support for caregivers, and avoiding social isolation, should be provided to caregivers. In addition, non-pharmacological and pharmacological treatments of NPS are also important to reduce caregiver’s stress. With our findings, interventions could be appropriately tailored to individualized situation, including caregiver’s needs and NPS in different age or dementia severity.
Disclosure
Yu-An Chen, Cheng-Chen Chang, and Wen-Fu Wang are co-first authors for this study. The authors report no conflicts of interest in this work.
References
1. Plassman BL, Langa KM, Fisher GG, et al. Prevalence of dementia in the United States: the aging, demographics, and memory study. Neuroepidemiology. 2007;29(1–2):125–132. doi:10.1159/000109998
2. Hebert LE, Weuve J, Scherr PA, et al. Alzheimer disease in the United States (2010–2050) estimated using the 2010 census. Neurology. 2013;80(19):1778–1783. doi:10.1212/WNL.0b013e31828726f5
3. Cheng ST. Dementia caregiver burden: a research update and critical analysis. Curr Psychiatry Rep. 2017;19(9):64. doi:10.1007/s11920-017-0818-2
4. Terum TM, Andersen JR, Rongve A, et al. The relationship of specific items on the Neuropsychiatric Inventory to caregiver burden in dementia: a systematic review. Int J Geriatr Psychiatry. 2017;32(7):703–717. doi:10.1002/gps.4704
5. Connors MH, Seeher K, Teixeira-Pinto A, et al. Dementia and caregiver burden: a three-year longitudinal study. Int J Geriatr Psychiatry. 2020;35(2):250–258. doi:10.1002/gps.5244
6. Li R, Singh M. Sex differences in cognitive impairment and Alzheimer’s disease. Front Neuroendocrinol. 2014;35(3):385–403.
7. Cohen D, Eisdorfer C, Gorelick P, et al. Sex differences in the psychiatric manifestations of Alzheimer’s disease. J Am Geriatr Soc. 1993;41(3):229–232. doi:10.1111/j.1532-5415.1993.tb06697.x
8. Tao Y, Peters ME, Drye LT, et al. Sex differences in the neuropsychiatric symptoms of patients with Alzheimer’s disease. Am J Alzheimers Dis Other Demen. 2018;33(7):450–457. doi:10.1177/1533317518783278
9. Ott BR, Tate CA, Gordon NM, et al. Gender differences in the behavioral manifestations of Alzheimer’s disease. J Am Geriatr Soc. 1996;44(5):583–587. doi:10.1111/j.1532-5415.1996.tb01447.x
10. Laws KR, Irvine K, Gale TM. Sex differences in Alzheimer’s disease. Curr Opin Psychiatry. 2018;31(2):133–139. doi:10.1097/YCO.0000000000000401
11. Mohamed S, Rosenheck R, Lyketsos CG, Schneider LS. Caregiver burden in Alzheimer disease: cross-sectional and longitudinal patient correlates. Am J Geriatr Psychiatry. 2010;18(10):917–927. doi:10.1097/JGP.0b013e3181d5745d
12. Huang SS, Liao YC, Wang WF, Lai TJ. The factors associated with burden of caring patients with dementia: a memory clinic based study. Taiwan J Psychiatry. 2012;26(2):96–104.
13. Brodaty H, Woodward M, Boundy K, et al. Prevalence and predictors of burden in caregivers of people with dementia. Am J Geriatr Psychiatry. 2014;22(8):756–765. doi:10.1016/j.jagp.2013.05.004
14. Kang HS, Myung W, Na DL, et al. Factors associated with caregiver burden in patients with Alzheimer’s disease. Psychiatry Investig. 2014;11(2):152–159. doi:10.4306/pi.2014.11.2.152
15. Lee SM, Lee Y, Choi SH, et al. Clinical and demographic predictors of adverse outcomes in caregivers of patients with dementia. Dement Neurocogn Disord. 2019;18(1):10–18. doi:10.12779/dnd.2019.18.1.10
16. Yan GJ, Wang WF, Jhang KM, Lin CW, Wu HH. Association between patients with dementia and high caregiving burden for caregivers from a medical center in Taiwan. Psychol Res Behav Manag. 2019;12:55–65. doi:10.2147/PRBM.S187676
17. Albert MS, DeKosky ST, Dickson D, et al. The diagnosis of mild cognitive impairment due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011;7(3):270–279. doi:10.1016/j.jalz.2011.03.008
18. McKhann GM, Knopman DS, Chertkow H, et al. The diagnosis of dementia due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011;7(3):263–269. doi:10.1016/j.jalz.2011.03.005
19. Jhang KM, Chang MC, Lo TY, et al. Using the Apriori algorithm to classify the care needs of patients with different types of dementia. Patient Prefer Adherence. 2019;13:1899–1912. doi:10.2147/PPA.S223816
20. Jhang KM, Wang WF, Chang HF, et al. Care needs of community-residing male patients with vascular cognitive impairment. Neuropsychiatr Dis Treat. 2020;16:2613–2621, 2020. doi:10.2147/NDT.S277303
21. Larose DT. Discovering Knowledge in Data: An Introduction to Data Mining. Hoboken, NJ: John Wiley & Sons; 2005.
22. Isik AT, Soysal P, Solmi M, Veronese N. Bidirectional relationship between caregiver burden and neuropsychiatric symptoms in patients with Alzheimer’s disease: a narrative review. Int J Geriatr Psychiatry. 2019;34(9):1326–1334. doi:10.1002/gps.4965
23. Shimabukuro J, Awata S, Matsuoka H. Behavioral and psychological symptoms of dementia characteristic of mild Alzheimer patients. Psychiatry Clin Neurosci. 2005;59(3):274–279. doi:10.1111/j.1440-1819.2005.01371.x
24. Hashimoto M, Yatabe Y, Ishikawa T, et al. Relationship between dementia severity and behavioral and psychological symptoms of dementia in dementia with Lewy bodies and Alzheimer’s disease patients. Dement Geriatr Cogn Dis Extra. 2015;5(2):244–252. doi:10.1159/000381800
25. Lopez OL, Becker JT, Sweet RA, et al. Psychiatric symptoms vary with the severity of dementia in probable Alzheimer’s disease. J Neuropsychiatry Clin Neurosci. 2003;15(3):346–353. doi:10.1176/jnp.15.3.346
26. Zhao QF, Tan L, Wang HF, et al. The prevalence of neuropsychiatric symptoms in Alzheimer’s disease: systematic review and meta-analysis. J Affect Disord. 2016;190:264–271. doi:10.1016/j.jad.2015.09.069
27. Maust DT, Kales HC, McCammon RJ, et al. Distress associated with dementia-related psychosis and agitation in relation to healthcare utilization and costs. Am J Geriatr Psychiatry. 2017;25(10):1074–1082. doi:10.1016/j.jagp.2017.02.025
28. Allegri RF, Sarasola D, Serrano CM, et al. Neuropsychiatric symptoms as a predictor of caregiver burden in Alzheimer’s disease. Neuropsychiatr Dis Treat. 2006;2(1):105–110.
29. Connors MH, Ames D, Woodward M, et al. Psychosis and clinical outcomes in Alzheimer disease: a longitudinal study. Am J Geriatr Psychiatry. 2018;26(3):304–313. doi:10.1016/j.jagp.2017.10.011
30. Scarmeas N, Brandt J, Albert M, et al. Delusions and hallucinations are associated with worse outcome in Alzheimer disease. Arch Neurol. 2005;62(10):1601–1608. doi:10.1001/archneur.62.10.1601
31. Bassiony MM, Steinberg MS, Warren A, et al. Delusions and hallucinations in Alzheimer’s disease: prevalence and clinical correlates. Int J Geriatr Psychiatry. 2000;15(2):99–107. doi:10.1002/(SICI)1099-1166(200002)15:2<99::AID-GPS82>3.0.CO;2-5
32. Wilson RS, Tang Y, Aggarwal NT, et al. Hallucinations, cognitive decline, and death in Alzheimer’s disease. Neuroepidemiology. 2006;26(2):68–75. doi:10.1159/000090251
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.