Back to Journals » Journal of Asthma and Allergy » Volume 15
Assessment of Predictor Factors Associated with Multiple Emergency Department Attendance with Asthma Attack: A Qualitative and Multicentric Prospective Observational Study
Authors Vaittinada Ayar P , Taillé C, Vaittinada Ayar P , Gay M, Diallo A, Dara AF, Peyrony O, Chassany O , Casalino E
Received 1 September 2021
Accepted for publication 10 December 2021
Published 5 March 2022 Volume 2022:15 Pages 303—313
DOI https://doi.org/10.2147/JAA.S337072
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Amrita Dosanjh
Prabakar Vaittinada Ayar,1,2 Camille Taillé,2,3 Pradeebane Vaittinada Ayar,4 Matthieu Gay,1 Alhassane Diallo,2,5 Aïchata Fofana Dara,6 Olivier Peyrony,2,7 Olivier Chassany,2,6,8 Enrique Casalino2,9
1Emergency Department, Beaujon University Hospital-APHP, Paris, France; 2University of Paris, Paris, France; 3Respiratory Diseases Department, Bichat University Hospital-APHP, Paris, France; 4NORCE Norwegian Research Centre, Bjerknes Centre for Climate Research, Bergen, Norway; 5Epidemiology Department, Biostatistics and Clinical Research, Bichat University Hospital-APHP, Paris, France; 6UMR 1123, Inserm, Paris, France; 7Emergency Department, Saint-Louis University Hospital-APHP, Paris, France; 8Health Economics Clinical Trial Unit (URC-ECO), Hotel-Dieu Hospital-APHP, Paris, France; 9Emergency Department, Bichat University Hospital-APHP, Paris, France
Correspondence: Prabakar Vaittinada Ayar, Email [email protected]
Purpose: Identified factors associated with multiple emergency department (ED) visits (≥) for asthma, which is associated with death.
Patients and Methods: We first conducted a qualitative study. We invited French-speaking adults (≥ 18 years old) with a diagnosis of asthma for more than 6 months. The identified concepts were transcribed into items. A Delphi method allowed for selecting items for a self-reported questionnaire. In an observational multicentric cross-sectional quantitative study, the resulting 20-item questionnaire and 12-item General Health Questionnaire, exploring psychological distress, were administered to adults visiting an ED for asthma exacerbation. Multivariable logistic regression was used to assess factors associated with ED visits.
Results: Data saturation was obtained after 8 patient interviews. Patients who came to the ED seemed unfamiliar with their illness or treatments but were concerned by the disease. The questionnaire was administered to 182 patients. On multivariable logistic regression, multiple and systematic ED visits were associated with asthma exacerbation (adjusted odds ratio (aOR) = 6.89, 95% confidence interval [CI]: 2.25– 21.09), asthma perceived as a handicap (aOR=3.19, 95% CI: 1.55– 6.57) and reported atopy (OR=2.09, 95% CI: 1.03– 4.26). High educational level and lack of maintenance inhaled corticosteroids were protective for multiple ED visits.
Conclusion: Inadequate medical care is frequent in patients attending the ED for an asthma exacerbation, associated with strong psychological impact. Questioning the reasons for consulting the ED may help quickly identify patients requiring asthma education and improve their referral.
Keywords: asthma, emergency department, multiple attendance, psychological burden
Introduction
Asthma is a widespread chronic disease that affects 339 million people worldwide,1 3.5 million in France. Among Europeans between 15 and 64 years old, the total cost of asthma was 19.3 billion euros in 2011,2 mainly related to the severity and poor control of the disease.3–5 In France, the annual asthma mortality rate decreased from 2000 to 908 between 2000 and 20126,7 and simultaneously to the annual hospitalization rate for asthma decreased significantly. In contradiction, emergency department (ED) visits for asthma exacerbation remained stable, with 200,000 visits per year.8
Most of the time, ED visits reflect uncontrolled asthma and poor assessment and perception of symptoms severity,9 which leads patients to mismanage the asthma attack.10 In 2014, the National Review of Asthma Deaths in the United Kingdom identified many risk factors for asthma death:11 34% of patients had more than two ED visits during the year preceding the death. An ED visit for asthma should be considered a warning sign associated with poor asthma control. Thus, the ED may play a part in the primary care of asthma.
Reasons for attending the ED for an asthma attack are multiple; some are related to the severity of the exacerbation, but some may also reflect poor asthma education, leading to delayed or unnecessary ED attendance.12 Indeed, the illness severity is sometimes misjudged by the physician,13,14 but poor education can concern several aspects, including self-recognition and self-management of asthma15,16 or the effect of perceived control of asthma on health outcomes.17
This study aimed to identify causes of multiple ED visits (≥2) for asthma to define customized interventions for managing asthma before and after ED visits. First, we used mixed-methods research: a qualitative study to define the main concepts, then a cross-sectional study to quantify the concepts. Then, we develop a predictive model for frequent ED users.
Materials and Methods
Qualitative Study
We conducted a qualitative study based on semi-structured interviews to data saturation between March and June 2017. The principal investigator (PV) included all consecutive French-speaking adult patients (≥ 18 years old) who were admitted because of asthma exacerbation to the ED at Bichat hospital. Patients with a diagnosis of asthma for more than 6 months and medication for at least 3 months were selected. Patients were contacted after discharge and asked to take part in a face-to-face interview with the principal investigator in the respiratory disease department. An interview guide, exploring the patient’s asthma perception; its diagnosis, treatment, current and expected care; and collaborative management (Appendix 1) was developed based on a review of the literature and discussion among the authors. The interview guide was revised according to the findings of the first interviews. Each interview was audio-recorded. Patient characteristics were collected (demographics, asthma diagnosis and follow-up, smoking status, living environment, atopy, comorbidities, and medical fee exempt status).
Interviews were fully and anonymously transcribed verbatim and analyzed by thematic analysis with NVivo 10 software after data saturation18 (see definition in Supplementary Method) section. This step was necessary to refine research concepts. Concepts were classified into categories, and fell into 34 items (see definition Supplementary Method). A Delphi method19 (5 emergency physicians, 1 methodologist, 1 pulmonologist) was used to select the most important items. This step was necessary to choose most important concept to build a short and accurate questionnaire suitable for ED activity.
Cross-Sectional Study
We performed an observational multicentric cross-sectional quantitative study between January 2018 and March 2019 in 3 EDs in the Paris area. Emergency physicians included French-speaking adults (above 18 years old) visiting an ED for an asthma exacerbation; eligible patients had a diagnosis of asthma for more than six months and took asthma medications for at least three months. After acceptation, patients were invited to fill out two questionnaires before leaving the ED: the questionnaire resulting from the qualitative analysis on asthma, and the 12-item General Health Questionnaire (GHQ-12). The GHQ-12 is generally considered a unidimensional scale of psychological distress,20–22 consisting of items capturing symptoms of anxiety, depression, social dysfunction, and loss of confidence. Answers are rated according a 4-point Likert scale, from 0, no distress, to 4, high distress. A total GHQ-12 score above 4 indicates psychological distress.
An Ethics Committee (CPP Sud-Méditerranée I, Marseille, France) approved the study (no. IDRCB: 2016-A02028-43). Consent was obtained from all participants after information about the purpose of the study and anonymity of the responses in the publication. This study was conducted in accordance with the Declaration of Helsinki. The study was registered at ClinicalTrials.gov (NCT03099915).
Statistical Analysis
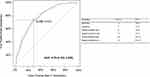
For the quantitative study, categorical data are described with ratios (in %) and continuous data with median and interquartile range (IQR). Characteristics of patients with multiple visits (≥2 ED visits during the 12 months before the day of visit) and patients who visited the ED no more than once during the last 12 months were compared by chi-square and Wilcoxon rank-sum tests as appropriate. Univariate logistic regression was used to quantify the magnitude of the association between factors and multiple visits, estimating odds ratios (ORs) and 95% confidence intervals (CIs). Variables with a p < 0.10 on univariate analysis were entered into the multivariable logistic regression model. We used a generalized linear model23 to obtain crude and adjusted ORs. The model selection was based on the Akaike Information Criterion24 to find the best compromise between the number of factors to keep and the accuracy of the logistic regression. To estimate the optimal discrimination cutoff, we used the receiver operating characteristic (ROC) curve with Youden’s index method.25 The Hosmer-Lemeshow test26 was used to assess the model’s calibration. Data analyses involved using R 4.0.3. Statistical significance was set at 95% and all tests were two-sided.
Results
Qualitative Analysis
Eleven patients were asked to participate, two patients refused, and one did not come to the appointment. Data saturation was obtained after interviewing 8 patients (6 women) because of very specific items. The median age of patients was 48 years (range 44–53). Five had a foreign home country, and 2 continued their study after high school. The median duration of the interview was 47 min (range 44–50). Asthma was initially diagnosed by the primary care physician (general practitioner or emergency physician) and confirmed a few years later by respiratory functional explorations. Asthma symptoms for all patients except one appeared after the age of 20. From the thematic analysis of verbatim, 3 main themes emerged:
1) Need for information on the disease, lack of knowledge and perception of asthma as disease (Table S1).
In general, the quality of the level of information on the disease was poor. Despite the fear, patients did not seek to improve their knowledge about the disease. They all felt that their family doctor had a low level of involvement in asthma care. Patients were resigned, isolated, and felt physically and socially handicapped. They presented moral distress.
2) Identification of asthma symptoms and management of asthma exacerbation (Table S2)
Patients reported difficulties in identifying symptoms of asthma exacerbation. None of the patients had an asthma action plan. Therefore, lack of relief treatment and medical advice to evaluate the severity of the exacerbation was frequently associated with stress and anxiety. Patients spontaneously avoided situations identified as associated with asthma symptoms, such as physical activities, pollen season or pollution peak.
3) Asthma treatments (Table S3)
Patients had poor knowledge of treatments. Maintenance and relief treatments were not identified. Self-reported adherence to asthma treatment was poor. Most patients felt that they took too many or inappropriate medications. They were sometimes embarrassed to take medication in front of people.
In summary, the qualitative analysis revealed that patients who came to the ED were unfamiliar with both the disease and associated treatments, related to insufficient medical follow-up. Asthma was experienced as a physical and/or social handicap, with a strong impact on quality of life. Difficulties in identifying symptoms of asthma exacerbation and their severity were linked to anxiety. After the Delphi process, 20 items were retained in the final questionnaire (Appendix 2).
Quantitative Analysis
A total of 182 patients were recruited for the study. Characteristics of patients are reported in Table 1. The median age was 43 (range 28–56); 69 (38%) were men, and the median duration of asthma was 19 years (range 10–26). Overall, 59% of participants had private insurance, and 51% were employed. For 54%, asthma was diagnosed after the age of 18.
 |
Table 1 Socio-Demographic Characteristics of Participants with Asthma by Emergency Department (EDs) Attendance (N=182) |
During the previous year, 43% of patients had visited the ED at least twice for asthma. Frequent ED users and others patients did not differ in characteristics, except frequent ED users who were less likely to have a university degree (Table 1). In most cases (81%), patients were aware of a potentially fatal issue during an asthma attack and a large part of the population had a feeling of loneliness (37%) and powerless (44%) to cope with illness. The proportion of complaints of physical handicap was higher for frequent ED users (72% vs 47%, p = 0.0007). However, only 55% had a respiratory function evaluation, and 38% had a consultation with a pulmonologist for asthma diagnosis (Table 2).
 |
Table 2 Questionnaire on Observance and Knowledge of Global Initiative for Asthma Criteria and General Health Questionnaire 12 (GHQ-12) by ED Attendance (N=182) |
Our study population believed for 67% of them to do the right therapeutic action in case of asthma attack. But only 8% had the knowledge of the right dosage of short-acting beta2 agonist before attending the ED. Moreover, only 20% had a written action plan (Table 2). In all, 24% of patients did not use beta2 agonists to relieve asthma symptoms. The proportion of patients without maintenance inhaled corticosteroids (ICS) was lower in frequent ED users group (17% vs 43%, p=0.0003). Self-reported adherence to treatments was low but similar between the 2 groups. When assessing reasons for attending an ED during an asthma attack, systematic visits to the ED during asthma symptoms was the most common answer among the frequent ED users (27% vs 7%, p<0.00002). However, 86% of patients with one visit reported an unusual asthma attack as a main reason. There were 28 patients who used ED as primary source of care, with a median age of 41 vs 44 years old for the rest of the study population (p=0.65). Among these 28 patients, they were 52% of men vs 36% of men for the rest of the study population (p=0.11). The main characteristic of patients who used ED as primary source of care was, they were frequent ED users in 75% of cases vs 37% for other patients (p=0.0002). However, only 14% suffered from an unusual asthma attack vs 89% for other patients (p<0.0001).
There were 96 patients reporting allergic history, they were younger than non-allergic patients (34 vs 48 years old; p= 0.004). There was no difference in proportion treated by ICS between allergic and no allergic patients. Among allergic patients, there were more frequent ED users compared to non-allergic patients (50% vs 35%; p=0.046). A high proportion of allergic patients were diagnosed for asthma before three years old (23% vs 8%, p=0.005) in contrast to other patients who were diagnosed after age of 18 in most of the cases (70% vs 45%; p=0.004). ICS use as maintenance treatment was not a protective factor for multiple attendance to ED, and this was similar for allergic patients.
The GHQ-12 score did not differ among the two groups: 47% of patients exhibited psychological suffering (score >3), and 22% of patients were highly symptomatic (score ≥ 7). Women had higher scores (> 3) than men (55% vs 38%; p=0.039).
On multivariable logistic regression analysis (Table 3), frequent visits were associated with systematic consultation for loss of asthma control (adjusted OR, aOR = 6.89, 95% CI: 2.25–21.09), perceived handicap (aOR = 3.19, 95% CI: 1.55–6.57) and atopy (aOR = 2.09, 95% CI: 1.03–4.26). No maintenance ICS and high educational level prevented from multiple ED visits (OR = 0.28, 95% CI: 0.14–0.58 and OR = 0.49, 95% CI: 0.26–0.93). The model calibration provided by the Hosmer and Lemeshow test was not significant (p=0.99). For predicting multiple attendance, the performance criteria for our model were sensitivity 74%, specificity 71%, and area under the ROC curve 0.79 (95% CI: 0.72–0.86) (Figure 1).
 |
Table 3 Multivariable Analysis of Risk Factors of Multiple Visits to the ED |
Discussion
In this multicentric prospective cohort study of 182 patients visiting an ED for an asthma exacerbation, 43% had visited the ED ≥ 2 times during the previous year. Inadequate asthma care was frequent in this population visiting the ED (lack of relief or maintenance treatment, lack of an action plan, poor adherence to treatments and poor education), as previously described,10,27 but was not associated with risk of multiple visits. Risk of multiple ED visits was more likely among patients receiving maintenance ICS. Psychological distress and handicap were frequently reported among patients visiting the ED for an asthma attack, especially those with multiple visits.
This study found psychological distress among asthma patients (GHQ-12 score > 3), most being symptomatic ([4–6]) or highly symptomatic ([7–12]). Asthma, even when non-severe, was considered a socio-professional handicapping disability, particularly for those with multiple ED visits. Asthma patients have more anxiety disorders (11% to 37%) and depressive disorders (11% to 18%) than the general population.28–33 Psychological problems in asthma patients are related to poor health outcomes, including increased asthma symptom severity, impaired asthma control, over-use of rescue medications and reduced quality of life.34,35 These problems must be addressed in asthma care, with psychological support and multidisciplinary team management.
In our study, most of the patients who came to the ED had a poor follow-up of their disease. They did not have an asthma action plan, or had a poor knowledge about asthma relief treatments and complained of poor involvement of their doctors in asthma care. A recent French qualitative study underlined the weakness of French asthma patient management.36 Such a lack of care has been repeatedly described in both adults and children attending the ED for asthma. Adams et al reported the factors associated with asthma and repeated visits to EDs over a 12-month period.10,12,37 In addition to revealing factors related to severity, the authors found the absence of a written asthma action plan, the avoidance of coping strategies, and poor attitudes about self-management. In our study, 27% of patients with multiple visits reported systematic visits to the ED when asthma symptoms occurred, regardless of the exacerbation severity.
Education and an action plan are clearly key points to improve asthma control and decrease unnecessary visits. Ensuring a regular follow-up appointment with the primary care physician can also decrease repeat ED visits. However, we found that patients attending the ED for asthma exacerbation are a heterogeneous population, with different needs. Most of those with maintenance ICS therapy visited multiple times, but whether some patients with severe asthma could be detected in this group is unknown. The identification of these different types of patients in the ED, along with the identification of flaws in their medical follow-up and educational needs, may allow for earlier referral to an adequate dedicated consultation.38–41 Regarding the patients with one or less visit at ED, ICS was not used in large proportion. It could be explained by a less severe asthma than frequent ED users or a mistake in diagnosis of asthma. Indeed, Aaron et al had shown after reassessment of asthma, the initial diagnosis was ruled out in 33.1% of asthmatic patients. These patients did not use daily asthma medications or had medications weaned.42
Whatever the cause, some reasons of ED attendance were already defined convenience, anxiety or as self-perceived urgency, need for hospital care, treatment, investigations or anxiety,43 Our discrimination model could be used to detect patients with risk of multiple visits to ED. The systematic visit gives us information about patient habits and how the patient copes with the situation. It could reflect at least a lack of knowledge or medical education about asthma, or lack of other medical resource. It could also mean that for some patient asthma was poorly controlled or in that the ED visit was inappropriate. The perception of asthma as handicap could reveal anxiety in asthma patient. These points were indicative of need for more attention about educational or therapeutic action for asthmatic patients.
Our study had several limitations. We included patients from 3 university hospital EDs in a large urban area, with a high proportion of low-income and/or immigrant patients. The study was not designed for ethnic cultural barriers analysis. Therefore, our findings may not be generalizable to other populations. Moreover, in other healthcare systems, patients are not able to come directly to an ED as in France. The questionnaires were answered by patients without oversight, we had few missing data. There was no follow-up after the ED visit. We did not assess asthma at baseline because we focused on why the patient came to the ED and not the consistency between severity and consultation. The age of the diagnosis of our patients may question the correctness of the diagnosis; only 55% of our patients had a respiratory function evaluation, in only 38% of the cases was the pneumologist involved in the diagnosis, and 31% of our patients did not have daily treatment. These patients may have milder asthma than those with multiple visits, but the design of the study did not allow for assessing asthma control or severity. All data were declarative; for example, the number of ED visits was not confirmed in our medical record software.
Conclusion
Inadequate medical care is frequent in patients attending the ED for an asthma exacerbation, with only a few differences between patients with multiple visits and only one visit in the past year, associated with strong psychological impact. Questioning the reasons for consulting the ED may help quickly identify patients requiring asthma education and improve their referral. Our discrimination model showed good performance and may help to screen patients in the ED who require close follow-up.
Data Sharing Statement
The whole deidentified data and other study documents will be shared simply by asking the corresponding author ([email protected]) during 10 years after the end of the study.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Funding
There is no funding to report.
Disclosure
Camille Taillé reports grants and personal fees from AstraZeneca, Novartis, and GSK, grants from Sanofi, and personal fees from Stallergenes, outside the submitted work. Olivier Peyrony reports personal fees from Bristol Myers Squibb, outside the submitted work. The authors report no other potential conflicts of interest in this work.
References
1. James SL, Abate D, Abate KH, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390(10100):1211–1259. doi:10.1016/S0140-6736(17)32154-2
2. The global asthma report; 2018. Available from: http://www.globalasthmareport.org.
3. Laforest L, Com-Ruelle L, Devouassoux G, Pison C, Van Ganse É. Enjeux économiques de l’asthme sévère [Economic issues in severe asthma]. Presse Méd. 2008;37(1):117–128. French. doi:10.1016/j.lpm.2007.06.019
4. Direction de la recherche, de l’évaluation, des études et des statistiques (Drees). L’état de Santé de La Population En France [Health status of the french population]. Edition 2015; 2015. Available from: http://drees.social-sante.gouv.fr/IMG/pdf/synthese_v7_05022015.pdf.
5. Afrite A, Allonier C, Com-Ruelle L, Le Guen N. L’asthme en France en 2006: prévalence, contrôle et déterminants [Asthma in France in 2006: prevalence, control and determinants]. IRDES report. 2011:1820. French. Available from: https://www.irdes.fr/Publications/Qes/Qes138.pdf.
6. Surveillance épidémiologique de l’asthme en France/Asthme/Maladies chroniques et traumatismes/Dossiers thématiques/Accueil [Epidemiological surveillance of asthma in France/Asthma/Chronic diseases and injuries/Thematic files/Home]. Available from: http://invs.santepubliquefrance.fr/fr./Dossiers-thematiques/Maladies-chroniques-et-traumatismes/Asthme/Surveillance-epidemiologique-de-l-asthme-en-France.
7. Delmas M, Boussac-Zarebska M, Houot M, Lauzeille D, Yuriko I, Fuhrman C. L’apport des bases médico-administratives dans la surveillance des maladies chroniques en France [The contribution of medico-administrative databases in the surveillance of chronic diseases in France]. Bull Epidemiol Hebd. 2013;(Hors–série):30–35. French.
8. Caserio-Schönemann C, Sanna A, Bousquet V, et al. Determinants of daily attendances in Emergency Departments for Asthma in the Paris area. Online J Public Health Inform. 2015;7(1). doi:10.5210/ojphi.v7i1.5780
9. Haughney J, Barnes G, Partridge M, Cleland J. The living & breathing study: a study of patients’ views of asthma and its treatment. Prim Care Respir J. 2004;13(1):28–35. doi:10.1016/j.pcrj.2003.11.007
10. Adams RJ, Smith BJ, Ruffin RE. Factors associated with Hospital admissions and repeat emergency department visits for adults with asthma. Thorax. 2000;55(7):566–573. doi:10.1136/thorax.55.7.566
11. Levy M, Andrews R, Buckingham R, et al. Why asthma still kills: the National Review of Asthma Deaths (NRAD); 2014. Available from: https://uwe-repository.worktribe.com/output/817751.
12. Al-Muhsen S, Horanieh N, Dulgom S, et al. Poor asthma education and medication compliance are associated with increased emergency department visits by asthmatic children. Ann Thorac Med. 2015;10(2):123–131. doi:10.4103/1817-1737.150735
13. Matsunaga K, Hamada K, Oishi K, Yano M, Yamaji Y, Hirano T. Factors associated with physician-patient discordance in the perception of Asthma control. J Allergy Clin Immunol Pract. 2019;7(8):2634–2641. doi:10.1016/j.jaip.2019.04.046
14. Crespo-Lessmann A, Plaza V, González-Barcala FJ, Fernández-Sánchez T, Sastre J. Concordance of opinions between patients and physicians and their relationship with symptomatic control and future risk in patients with moderate-severe asthma. BMJ Open Respir Res. 2017;4(1):e000189. doi:10.1136/bmjresp-2017-000189
15. Partridge MR, van der Molen T, Myrseth SE, Busse WW. Attitudes and actions of asthma patients on regular maintenance therapy: the INSPIRE study. BMC Pulm Med. 2006;6:13. doi:10.1186/1471-2466-6-13
16. Song WJ, Won HK, Lee SY, et al. Patient’s experience of asthma exacerbation and management: a qualitative study of severe asthma. ERJ Open Res. 2020:00528–02020. doi:10.1183/23120541.00528-2020
17. Calfee CS, Katz PP, Yelin EH, Iribarren C, Eisner MD. The influence of perceived control of asthma on health outcomes. Chest. 2006;130(5):1312–1318. doi:10.1378/chest.130.5.1312
18. Saunders B, Sim J, Kingstone T, et al. Saturation in qualitative research: exploring its conceptualization and operationalization. Qual Quant. 2018;52(4):1893–1907. doi:10.1007/s11135-017-0574-8
19. Niederberger M, Spranger J. Delphi technique in health sciences: a map. Front Public Health. 2020;8:457. doi:10.3389/fpubh.2020.00457
20. Goldberg D. Manual of the General Health Questionnaire. NFER Nelson; 1978.
21. Goldberg DP, Gater R, Sartorius N, et al. The validity of two versions of the GHQ in the WHO study of mental illness in general health care. Psychol Med. 1997;27(1):191–197. doi:10.1017/S0033291796004242
22. Hankins M. The factor structure of the twelve item General Health Questionnaire (GHQ-12): the result of negative phrasing? Clin Pract Epidemiol Ment Health. 2008;4:10. doi:10.1186/1745-0179-4-10
23. Nelder JA, Wedderburn RWM. Generalized linear models. J R Stat Soc Series A. 1972;135(3):370. doi:10.2307/2344614
24. Akaike H. A new look at the statistical model identification. IEEE Trans Automat Contr. 1974;19(6):716–723. doi:10.1109/TAC.1974.1100705
25. Youden WJ. Index for rating diagnostic tests. Cancer. 1950;3(1):32–35. doi:10.1002/1097-0142(1950)3:1<32::aid-cncr2820030106>3.0.co;2-3
26. Cole T. Hosmer DW, Lemeshow S, Applied Logistic Regression. Wiley, New York: Wiley Online Library; 1991.
27. Salmeron S, Liard R, Elkharrat D, Muir JF, Neukirch F, Ellrodt A. Asthma severity and adequacy of management in accident and emergency departments in France: a prospective study. Lancet. 2001;358(9282):629–635. doi:10.1016/S0140-6736(01)05779-8
28. Boulet LP. Influence of comorbid conditions on asthma. Eur Respir J. 2009;33(4):897–906. doi:10.1183/09031936.00121308
29. Katon WJ, Richardson L, Lozano P, McCauley E. The relationship of asthma and anxiety disorders. Psychosom Med. 2004;66(3):349–355. doi:10.1097/01.psy.0000126202.89941.ea
30. Adams RJ, Wilson DH, Taylor AW, et al. Psychological factors and asthma quality of life: a population based study. Thorax. 2004;59(11):930–935. doi:10.1136/thx.2003.010256
31. Weiser EB. The prevalence of anxiety disorders among adults with asthma: a meta-analytic review. J Clin Psychol Med Settings. 2007;14(4):297–307. doi:10.1007/s10880-007-9087-2
32. Heaney LG, Conway E, Kelly C, Gamble J. Prevalence of psychiatric morbidity in a difficult asthma population: relationship to asthma outcome. Respir Med. 2005;99(9):1152–1159. doi:10.1016/j.rmed.2005.02.013
33. Ciprandi G, Schiavetti I, Rindone E, Ricciardolo FLM. The impact of anxiety and depression on outpatients with asthma. Ann Allergy Asthma Immunol. 2015;115(5):408–414. doi:10.1016/j.anai.2015.08.007
34. Lavoie KL, Cartier A, Labrecque M, et al. Are psychiatric disorders associated with worse asthma control and quality of life in asthma patients? Respir Med. 2005;99(10):1249–1257. doi:10.1016/j.rmed.2005.03.003
35. Grzeskowiak LE, Smith B, Roy A, et al. Impact of a history of maternal depression and anxiety on asthma control during pregnancy. J Asthma. 2017;54(7):706–713. doi:10.1080/02770903.2016.1258080
36. Hannane A, Misane L, Devouassoux G, Colin C, Letrilliart L. Asthma patients’ perception on their care pathway: a qualitative study. NPJ Prim Care Respir Med. 2019;29(1):9. doi:10.1038/s41533-019-0121-2
37. Losappio L, Heffler E, Carpentiere R, et al. Characteristics of patients admitted to emergency department for asthma attack: a real-LIFE study. BMC Pulm Med. 2019;19(1):107. doi:10.1186/s12890-019-0869-8
38. Castro M, Zimmermann NA, Crocker S, Bradley J, Leven C, Schechtman KB. Asthma intervention program prevents readmissions in high healthcare users. Am J Respir Crit Care Med. 2003;168(9):1095–1099. doi:10.1164/rccm.200208-877OC
39. Baren JM, Boudreaux ED, Brenner BE, et al. Randomized controlled trial of emergency department interventions to improve primary care follow-up for patients with acute asthma. Chest. 2006;129(2):257–265. doi:10.1378/chest.129.2.257
40. Ducharme FM, Zemek RL, Chalut D, et al. Written action plan in pediatric emergency room improves asthma prescribing, adherence, and control. Am J Respir Crit Care Med. 2011;183(2):195–203. doi:10.1164/rccm.201001-0115OC
41. Villa-Roel C, Nikel T, Ospina M, Voaklander B, Campbell S, Rowe BH. Effectiveness of educational interventions to increase primary care follow-up for adults seen in the Emergency Department for Acute Asthma: a systematic review and meta-analysis. Acad Emerg Med. 2016;23(1):5–13. doi:10.1111/acem.12837
42. Aaron SD, Vandemheen KL, FitzGerald JM, et al. Reevaluation of diagnosis in adults with physician-diagnosed asthma. JAMA. 2017;317(3):269–279. doi:10.1001/jama.2016.19627
43. Coster JE, Turner JK, Bradbury D, Cantrell A. Why do people choose emergency and urgent care services? a rapid review utilizing a systematic literature search and narrative synthesis. Acad Emerg Med. 2017;24(9):1137–1149. doi:10.1111/acem.13220
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.