Back to Journals » Integrated Pharmacy Research and Practice » Volume 11
Assessment of Pharmaceutical Service Quality Provided in Community Drug Retail Outlets in Selected Towns, South West Ethiopia
Authors Demissie F, Buno H, Paulos G
Received 6 June 2022
Accepted for publication 12 August 2022
Published 22 August 2022 Volume 2022:11 Pages 117—126
DOI https://doi.org/10.2147/IPRP.S375155
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Jonathan Ling
Fitsum Demissie,1 Henok Buno,1 Getahun Paulos2
1Department of Pharmacy, Institute of Health, Bule-Hora University, Bule-Hora, Oromia, Ethiopia; 2Department of Pharmaceutics, School of Pharmacy, Institute of Health Sciences, Jimma University, Jimma, Oromia, Ethiopia
Correspondence: Getahun Paulos, Tel +251 911-72-44-71, Email [email protected]
Background: Inappropriate pharmaceutical services may result in unsafe, ineffective, and poor-quality treatment. This practice ultimately will lead to prolonged illness, suffering and damage to the patient and an increase in the cost of treatment. This study aims to assess the activities of pharmacy professionals and the pharmaceutical service quality given in community drug retail outlets of selected towns, Southern Ethiopia.
Methods: A cross-sectional study was conducted on all drug retail outlets working in Adola, Bule Hora, Dilla, and Yabelo towns, southern Ethiopia from October 1 to November 30, 2021, by interview through self- structured questionnaires and participant observations of the dispensing process.
Results: A total of 46 (100%) dispensers participated. Out of which 18 (39.13%) respondents were from Dilla town, 11 (23.91%) were from Adola, 8 (17.39%) were from Bule Hora and 9 (19.57%) were from Yabelo town. Standard Reference Books 21 (45.7%) and Internet 20 (43.5%) were used as drug information sources by pharmacy professionals to get the latest facts about medicines. The leading causes of a dispensing error were incomplete prescription (54.34%) and illegible prescription (30.43%) from the prescriber. The errors were managed by communicating with patients (23, 50%), and prescribers (18, 39.13%). There was a high frequency of dispensing prescription drugs without prescription paper.
Conclusion: The study revealed that less than half of the respondents use standard reference books and the internet as their drug information sources. Incomplete prescriptions from the prescribers were found to be the leading cause of dispensing errors. Dispensing of prescription drugs without receiving an order from a prescriber remains a common problem. Therefore, extensive work from regulatory authorities and pharmacy professionals is required to improve the quality of pharmaceutical services provided in drug retail outlets.
Keywords: Adola, Bule-Hora, community, Dilla, retail outlets, quality service, Yabelo
Background
Quality service is one of the requirements of the healthcare system. Globally the need for quality healthcare service was given due attention during the World Health Assembly in 2002. Since then, considerable international attention directed toward minimizing healthcare-associated harm and improving the safety of all stakeholders through quality services.1 The healthcare system is expected to provide services such as health promotion, disease prevention, diagnosis and treatment, and rehabilitation.2 One of the components of the healthcare system that offer such services is the community drug retail outlets.
Community drug retail outlets most often are private sector healthcare facilities with minimal government involvement, and offer various primary healthcare services in addition to the traditional dispensing of prescribed medications.3 Pharmacy professionals working in community drug retail outlets are the most reachable and accessible healthcare professionals in a community due to their location. They are in the vicinity of communities close to where people work, live, perform day-to-day activities, and socially interact.4
As a front-line healthcare system, there is always growing pressure on community drug retail outlets to demonstrate and improve the quality of healthcare.5,6 This demand is particularly initiated by the need to determine and evidence how the extended role of community pharmacy teams contributes toward health service delivery and the reduction of pressure on other health sectors.7,8
The community drug retail outlets are involved in the following activities: trading in medications and medicinal products, preparing compounded medications, and providing information on medications and medicinal products.9,10 In addition, the retail outlets provide pharmaceutical care within which pharmacy professionals cooperate with patients and representatives of medical professionals to prevent, identify, and solve medication-related problems. The pharmaceutical care services provided to patients should be up to their standard. A pharmacy professional must ensure the utmost safety and effectiveness of medicines dispensed and the quality of life of a patient getting the services.11,12
In Ethiopia, community drug retail outlets include pharmacies which are medicine shops having the mandate to hold a range of medicines and run by a pharmacist; drug stores are medicine shops with a more limited range of medications and run by a druggist; and rural drug vendors, usually found in rural areas with an even more limited range of medications and run by other healthcare professional. The dispensing practice of these outlets in Ethiopia is regulated by the Ethiopian Food and Drug Authority (EFDA).36
In 1999, a joint document published by FIP and WHO published on good pharmacy practice in hospital and community retail outlets requested national pharmaceutical organizations to direct pharmaceutical care providers to ensure quality service to every patient.13 The document encouraged national pharmaceutical organizations to direct pharmacists to ensure service provision of appropriate quality to every patient. Many countries, including Ethiopia, have developed national standards as per the recommendations of FIP/WHO.14 However, studies indicate that still there has been a limited systemic implementation of quality pharmaceutical services, and a lack of strict control from regulatory bodies. Even in some situations, efforts made by the regulatory body have been unsustained and uncoordinated.15–17
Inappropriate pharmaceutical care services may result in unsafe, ineffective, and poor-quality treatment. This practice ultimately will lead to prolonged illness, suffering and damage to the patient, and an increase in the cost of treatment. Overall, it adversely affects the healthcare of an individual in particular and the community in general.18 The pharmaceutical services provided in Ethiopia are not different from the rest of the World. Although there are appreciable efforts by Ethiopian food and drug administration and professional associations, there remains poor pharmaceutical care and practices.
In Ethiopia, prescribing and dispensing practices are not generally practiced rationally, and as a result, patients are forced to use medicine irrationally.19–21 Moreover, dispensed items are labeled poorly, patient counseling practices are insufficient, incomplete compiling, and unreasonable patient charging with high prices for the dispensed items. The situations are more severe due to the availability of products that are smuggled and counterfeit and things are complicated.22 The inappropriate prescribing practices also contribute to dispensing errors. The most common reasons for dispensing errors include failure to communicate medication orders, illegible handwriting, incomplete prescription, confusion over similarly named drugs, or errors involving dosing units. The objectives of this study were to assess the availability of facilities such as equipment and materials in the dispensary room, and sources of the latest drug information for pharmacists and druggists. The study also identified the main problems and challenges encountered during dispensing practices. Furthermore, the present study evaluated the quality of pharmaceutical services provided in community drug retail outlets at Dilla, Adola, Bule Hora, and Yabelo Towns, Southern Ethiopia.
Methods and Materials
Study Area and Study Period
The study was conducted in Dilla, Bule Hora, Adola, and Yabelo towns, Southern Ethiopia from October –November 2021. Dilla town is the administrative center of the Gedeo zone in the Southern region of Ethiopia. The town is located 365 km to the South of Addis Ababa. The town has a longitude and latitude of 6°24′30″N 38°18′30″E, with an elevation of 1570 meters above sea level. The town has 9 kebeles (small administrative units), which are organized under three sub-cities. The total population of Dilla town projected to date is 94, 400 and the town has one hospital and three health centers. The town has 22 drug stores and Pharmacies.
Bule-Hora town is the capital of the West Guji Zone; the town is located 381 km to the South of Addis Ababa. The town is with an elevation of 1716 meters above sea level having a latitude and longitude of 5035ʹN 38015ʹE/5.5830N 38.2500E. The town has three kebeles. According to the city population Centre, it has a total population of 27,820 in the last census year, 2007 E.C. The governmental health institutions in Bule-Hora town are one General hospital, one health center, three health posts, 17 private clinics within different organizations, and 10 drug stores.
Adola is a town located in the Guji Zone of the Oromia Region and located 470 km from Addis Ababa. The town has a longitude and latitude of 11°48ʹ0”N, 41°42ʹ0”E, with an elevation of 1758 meters above sea level. The 2007 E.C national census reported a total population for this town of 22,938, of whom 11,706 were men and 11,232 was women. The town has three kebeles, one hospital, 1 HC, 4 private clinics and 13 drug stores and pharmacies.
Yabelo is the capital city of the Borena zone of the Oromia region and is located 575 km from Addis Ababa, the capital city of Ethiopia. The town has a latitude and longitude of 4°53′N 38°5′E and an elevation of 1857 meters above sea level. Yabelo has an estimated total population of 18,478 of whom 9551 are men and 8927 are women. The town has four kebeles and 1 hospital, 2 Health centers, 6 private clinics, nine drug stores, and pharmacies.
Study Design
A cross-sectional study design was employed in 46 (Forty-Six) community drug retail outlets in four towns.
Study Population
All dispensers working at Community pharmacies during the data collection period were included in the study and dispensers not available and closed pharmacies or drug stores were excluded from the study. The following variables are used as independent variables: age, sex, religion, and ethnicity, whereas access to facilities, type, and nature of dispensing error, access to drug information, and causes of dispensing error were considered dependent variables.
Operational Definitions
Percentage of Drugs Adequately Labelled: is defined as a percentage of labels that contains the name, strength, dosage regimen, duration, and quantity of the drug dispensed.
Dispensing Error: Errors occurred during dispensing in a pharmacy setting, such as not checking patient age, not dispensing the correct drug, correct frequency, and correct total quantity.
Data Collection Instrument and Procedures
The questionnaire format was adapted after reviews of different kinds of literature and pretested in the study of health care institutions.30,31 The format was further modified after a pretest was conducted. The survey was conducted by interviewing the pharmacist and druggist through self-structured questionnaires.
The questionnaire consisted of forty-four questions divided into three parts. Part one gathered information regarding the socio-demographic characteristics of pharmacy professionals. Part two assessed the availability of necessary facilities and infrastructure of drug retail outlets. Part three assessed the knowledge and experience of pharmacy professionals’ regarding dispensing practice. The complete form of the questionnaire used for data collection is provided as Supplementary Material.
In addition, participation observations of the dispensing process were conducted. To collect data on dispensing errors, we observed the practice of the dispensers while they are in their normal activity. To assess the labeling practice, we conducted exit interviews using structured questionnaires and observed each label for its adequacy. Finally, conditions of dispensing environment and dispensing aids were evaluated against a checklist developed for this study. Data collection was made by investigators.
Data Processing, Analysis, and Presentation
The collected data were entered, cleaned, and analyzed using SPSS version 20.0 software. The software was to determine the following descriptive statistics like mean, frequency, and percentages. Then the findings were presented using tables and figures.
Ethical Consideration
Ethical clearance was obtained from Bule Hora University, Institute of Health ethical review committee. Letter of permission was submitted to Community pharmacies in study towns.
Data was gathered after getting permission. Additionally, each respondent was informed about the objective of the survey. The data collectors discussed the issue of confidentiality and asked for consent before starting data collection and respondents were enlightened that they have full right to decline or discontinue participating in the research. Then verbal informed consent was obtained from study participants. In this study, verbal informed consent was used after being approved by the ethics review committee and the study was conducted following the Declaration of Helsinki.
Results
A total of 46 pharmacy professionals (pharmacists and druggists) participated in the study, giving a response rate of 100%. Out of which, 34 (73.9%) respondents were druggists and 12 (26.1%) were pharmacists. The dispensers’ socio-demographic characteristics were found in Table 1.
 |
Table 1 Socio-Demographic Characteristics of Pharmacists and Druggists in the Community Drug Retail Outlets in Study Towns |
As the current study depicts (Table 2) all community drug retail outlets had a refrigerator and 44 of them had thermometers (95.7%) in dispensing room. More than half of community drug retail outlets had a phone (65.2%) and 82.6% of them had portable water in dispensing rooms.
 |
Table 2 Availability of Equipment/Materials in Community Drug Retail Outlets of Study Towns |
According to this study, three-drug information updating sources were assessed in community drug retail outlets. The study revealed that Standard Reference Books 21 (45.7%) and Internet 20 (43.5%) were the main sources used by pharmacists for updating drug information in CP. However, leaflets were the least sources used by pharmacists serving in Community drug retail outlets (Table 3).
 |
Table 3 Availability of Guidelines and Sources of Drug Information for Updating the Pharmacists and Druggists in Community Drug Retail Outlets in Study Towns |
According to this study, 25 (54.34%) of prescriptions were incomplete and 14 (30.43%) of prescriptions were illegible and these two causes were a major source of prescription errors (Figure 1). At this time, various approaches have been used to manage the errors observed on prescriptions; the majority of dispensers communicate with patients 23 (50%), 18 (39.13%) communicate with Prescribers, and 1 (2.17%) dispense by guess in Community drug retail outlets (Figure 2).
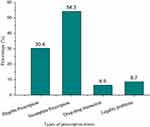 |
Figure 1 Types of prescription errors encountered during the dispensing process. |
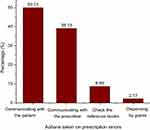 |
Figure 2 Prescription errors managed by the intervention of pharmacy professionals in study towns. |
In the study towns, 41 (89.13%) of community drug retail outlets are privately owned whereas only 5 (10.87%) are government owned. Most of the community drug retail outlets depend on private pharmaceutical suppliers for their drugs 34 (73.91%) and medical supplies needs and only 12 (26.09%) of them get drugs from governmental suppliers.
This study revealed there was a high frequency of dispensing prescription drugs without prescription paper and only 30.43% never dispensed prescription drugs without prescriptions (Figure 3).
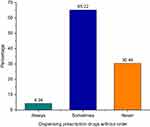 |
Figure 3 Frequency of dispensing prescription drugs without prescriptions. |
Concerning the measurement taken by 46 pharmacy professionals on prescription orders containing brand-named drugs, 19 (41.3%) of them did not take any measures and were filling a prescription order for the same brand-named orders. However, about 26 (57%) of professionals practiced generic substitution and dispensed another generic drug product with the same active ingredient (Table 4).
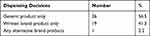 |
Table 4 Dispensing Decisions Taken by Pharmacy Professionals on Brand Product Prescription Orders |
According to this study, all dispensers have a practice of writing a name of a drug and its frequency of administration on the labels of dispensed medicines and a high percentage (91.3%) of them write the dose of the medicine prescribed during the dispensing process. On the other hand, few of them write the name of a patient (6.52%), and the date of dispensing (8.92%); and none of the dispensers had a practice of writing the storage conditions and precautions (Table 5). Based on this study incomplete prescription (54.3%) was the main cause of dispensing errors for pharmacy professionals.
 |
Table 5 Labeling Information Written During Dispensing Practice |
Discussion
The community drug retail outlets are critically placed as frontline primary health care settings among the community and are involved particularly in pharmaceutical care services. The role of pharmacy professionals in community drug retail outlets includes dispensing medications, provision of pharmaceutical care services, and other health promotion services to improve a patient’s health outcomes and quality of life.32–34
For proper pharmaceutical dispensing practices, community drug retail outlets should have all appropriate materials, equipment, and other resources to facilitate quick and proper dispensing of medicines and proper storage to keep medicines in optimum condition. The dispensers and owners of the establishment must always guarantee proper dispensing of all medications to their clients and ensure that there will not be any health risks associated with equipment’s/materials and sources of information. In this study, the most available facilities in the drug retail outlets were a thermometer and refrigerator (100%) and were quite good when compared to studies in Ambo and Bishoftu,22,23 respectively. However, 35% of facilities are not adequately equipped with a phone which is important for communication with physicians, other healthcare providers, and patients.
Regarding the availability of sources of drug information, the community drug retail outlets had Standard Treatment Guideline (STG), internet access, and periodic bulletins about 45.7%, 43.5%, and 10.9%, respectively. The limited availability of such resources in the study facilities indicates that the dispensers might lack the required up-to-date therapeutic information needed in their daily routine dispensing practices. This study is in line with a study done in Addis Ababa on two selected hospitals.24 These hospitals were using leaflets as information sources that may lead to bias.25
According to the current study, 56.6% of respondents took measures on prescription orders containing brand-named drugs and practiced generic substitution. However, about 41% of respondents still dispense drugs directly prescribed in their brand names. Brand name dispensing practice might be due to the promotion of brand products from pharmaceutical companies, customer preference, and wrong beliefs on generic products.26–28 However, this practice is not in line with the WHO recommendation. One of the directions of WHO guidelines on good prescription and dispensing are prescribers should write orders in their generic name and dispensers should also provide drugs in their generic name unless there is a particular reason.29 This practice will reduce health expenditures on pharmaceuticals. Hence, 41% of dispensers practicing dispensing medicines in their brand name should be discouraged through training and regulatory control.
The present study revealed that almost all dispensers have a practice of writing a name of a drug, its dose, and frequency of administration on the packages of dispensed medicines during the dispensing process. This result is by far better than the study performed in Ambo, Ethiopia22 where the labels of dispensed medicines contained names, strength, and quantity of drugs 11.1%, 11.1%, and 11.6%, respectively. Most studies, including the present study, however, indicated that dispensers are not writing the name of a patient, date of dispensing, the storage conditions, and precautions that should appear on the labels of dispensed medicine. These results are not in line with the WHO standard. The WHO drug use indicators stated that the percentage of adequate labeling on dispensed medicines should be 100%.
Regarding the practice of taking action on incomplete prescriptions, half of the dispensers working in the community drug retail outlets responded that they simply dispense medicines without communicating with the prescribers and only 8.96% of them search for information on reference books to correct the prescription errors. This might be due to poor dispenser-prescriber interaction, lack of confidence, and lack of phones in the dispensing room. The study conducted in Bishoftu,23 Ethiopia also revealed similar problems. Literature suggested that the development of communication skills should start at the undergraduate level and continue through the whole career of the dispensers.35 The pharmacy schools and other training institutions in the country should allocate enough training time on dispensing practices and communication skills. In addition, dispensers should get on-the-job training through continuous professional development.
Conclusion
The present study revealed that only 47% of community drug retail outlets use standard reference books and the internet as their drug information sources. More than half of the dispensers encountered incomplete prescriptions and a significant number of dispensers also faced illegible prescriptions. Incomplete prescriptions were not properly managed through timely communication with prescribers. Dispensed medicines from these facilities are not being adequately labeled as per the standard. Two out of five dispensers practiced dispensing medicines in their brand names directly as prescribed. In addition, dispensing prescription drugs without receiving an order from a prescriber remains a common problem. From the foregoing, it is evident that the integrated effort of pharmacy professionals, the communities, and the regulatory bodies is crucial in improving the quality of pharmaceutical services in community drug retail outlets.
Data Sharing Statement
The data collection tool is attached as an additional supplementary materials file. The data sets are available from the corresponding author on reasonable request.
Acknowledgments
The authors appreciate the data collectors and pharmacists and druggists who participated in the study. Finally, the authors extend their deepest gratitude to Bule Hora University for its supporting facilities.
Funding
Self-funding.
Disclosure
The authors declared no conflicts of interest in relation to this work.
References
1. World Health Organization. Delivering quality health services: a global imperative; 2019. Available from: https://www.who.int/publications/i/item/9789241513906.
2. Chen Z, Yu J, Song Y, Chui D. Aging Beijing: challenges and strategies of health care for the elderly. Ageing Res Rev. 2010;9:S2–S5. doi:10.1016/j.arr.2010.07.001
3. Melton BL, Lai Z. Review of community pharmacy services: what is being performed, and where are the opportunities for improvement? Integr Pharm Res Pract. 2017;6:79–89. doi:10.2147/IPRP.S107612
4. Goode J-V, Owen J, Page A, Gatewood S. Community-based pharmacy practice innovation and the role of the community-based pharmacist practitioner in the United States. Pharm. 2019;7(3):106.
5. Palaian S, Alomar M, Hassan N, Boura F. Opportunities for extended community pharmacy services in the United Arab Emirates: perception, practice, perceived barriers and willingness among community pharmacists. J Pharm Policy Pract. 2022;15(1):1–10. doi:10.1186/s40545-022-00418-y
6. World Health Organization. Improving the quality of health services: tools and resources; 2018. Available from: https://www.who.int/publications/i/item/9789241515085.
7. Anderson C, Blenkinsopp A, Armstrong M. Feedback from community pharmacy users on the contribution of community pharmacy to improving the public’s health: a systematic review of the peer-reviewed and non‐peer-reviewed literature 1990–2002. Health Expect. 2004;7(3):191–202. doi:10.1111/j.1369-7625.2004.00274.x
8. Rasheed MK, Alqasoumi A, Hasan SS, Babar Z. The community pharmacy practice change towards patient-centered care in Saudi Arabia: a qualitative perspective. J Pharm Policy Pract. 2020;13:59–68. doi:10.1186/s40545-020-00267-7
9. Bishop C, Yacoob Z, Knobloch MJ, Safdar N. Community pharmacy interventions to improve antibiotic stewardship and implications for pharmacy education: a narrative overview. Res Social Adm Pharm. 2019;15(6):627–631. doi:10.1016/j.sapharm.2018.09.017
10. Gubbins PO, Klepser ME, Dering-Anderson AM, Bauer KA, Darin KM, Klepser S. Point-of-care testing for infectious diseases: opportunities, barriers, and considerations in community pharmacy. J Am Pharma Assoc. 2014;54(2):163–171. doi:10.1331/JAPhA.2014.13167
11. Bratkowska K, Religioni U, Krysiński J, Merks P. Quality of pharmaceutical services in independent pharmacies and pharmacy chains in poland from the patient perspective. Patient Prefer Adherence. 2020;14:2459. doi:10.2147/PPA.S284014
12. Al‐Shaqha WM, Zairi M. Pharmaceutical care management: a modern approach to providing seamless and integrated health care. Int J Health Care Qual Assur Inc Leadersh Health Serv. 2001;14(6):282–301. doi:10.1108/09526860110409045
13. Unhurian L. Implementation of standards of good pharmacy practice in the world: a review. Asian J Pharm. 2018;12(01):42–46.
14. Al Husein N, Watson MC. Quality indicators and community pharmacy services: a scoping review. Int J Pharm Pract. 2019;27(6):490–500. doi:10.1111/ijpp.12561
15. Atif M, Razzaq W, Mushtaq I, Malik I, Razzaq M, Scahill S. Pharmacy services beyond the basics: a qualitative study to explore perspectives of pharmacists towards basic and enhanced pharmacy services in Pakistan. Int J Environ Res Public Health. 2020;17(7):2379. doi:10.3390/ijerph17072379
16. Mossialos E, Courtin E, Naci H, et al. From “retailers” to health care providers: transforming the role of community pharmacists in chronic disease management. Health Policy. 2015;119(5):628–639. doi:10.1016/j.healthpol.2015.02.007
17. Mucalo I, Hadžiabdić MO, Govorčinović T, Šarić M, Bruno A, Bates I. The development of the Croatian competency framework for pharmacists. Am J Pharm Educ. 2016;80(8):134. doi:10.5688/ajpe808134
18. Smith F. Community pharmacy in Ghana: enhancing the contribution to primary health care. Health Policy Plan. 2004;19(4):234–241. doi:10.1093/heapol/czh028
19. Suleman S, Woliyi A, Woldemichael K, Tushune K, Duchateau L, Degroote A. Pharmaceutical regulatory framework in Ethiopia: a critical evaluation of its legal basis and implementation. Ethiop J Health Sci. 2016;26(3):259–276. doi:10.4314/ejhs.v26i3.9
20. Beyene W, Jira C, Sudhakar M. Assessment of quality of health care in Jimma zone, southwest Ethiopia. Ethiop J Health Sci. 2011;21:49–58.
21. Teshale C, Hussein J, Mussa S. Assessment of the quality of pharmaceutical service in Jimma Zone, Oromia regional state, South West Ethiopia. Int J Pharm Teach Pract. 2014;5(2):1–6.
22. Lenjisa JL, Mosisa B, Woldu MA, Negassa DE, Tegegne GT, Gelaw BK. Analysis of dispensing practices at community pharmacy settings in Ambo Town, West Shewa, Ethiopia. J Community Med Health Educ. 2015;5(01):16. doi:10.4172/2161-0711.1000329
23. Kebede KS, Vijaya M, Dhanaraju MD, Gunasekaran T. Research article assessment of pharmaceutical service quality provided in bishoftu general hospital and community pharmacies at Bishoftu, Eastern Shoa, Ethiopia. J Pharm Allied Health Sci. 2016;6:8–13.
24. Ejigu E, Gedif T, Gebre-Mariam T. Assessment of drug labeling in two selected hospitals of Addis Ababa Ethiopia. J Ethiopian Pharma Assoc. 1998;14:123–125.
25. World Health Organization. Promoting rational use of medicines: core components; 2002. Available from https://apps.who.int/iris/bitstream/handle/10665/67438/WHO_EDM_2002.3.pdf.
26. Auta A, Bala ET, Shakur D. Generic medicine substitution: a cross-sectional survey of the perception of pharmacists in north-central, Nigeria. Med Princ Pract. 2014;23(4):53–58. doi:10.1159/000355473
27. Belay YB, Kassa TT, Teni FS, Dinkashe FT, Kassa AG, Welie AG. Assessment of knowledge, attitude, and practice of pharmacy professionals toward generic medicines, Northern Ethiopia, Mekelle: a cross-sectional study. J Basic Clin Pharm. 2017;8(4):1
28. Nasir BB, Muhammed OS, Busier MS. Assessment of knowledge, attitude and practice among pharmacy professionals towards generic medicines in Addis Ababa, Ethiopia. J Generic Med. 2019;15(4):185–192. doi:10.1177/1741134319875764
29. De Vries T, Henning R, Hogerzeil HV, Fresle D, Policy M. Guide to Good Prescribing: A Practical Manual. Geneva:World Health Organization; 1994:51–55
30. Mishore KM, Mekuria AN, Tola A, Ayele Y. Assessment of knowledge and attitude among pharmacists toward pharmaceutical care in eastern Ethiopia. BioMed Res Int. 2020;2020:1–7. doi:10.1155/2020/7657625
31. Ayalew MB, Solomon L, Abay S. Pharmaceutical care practice in community and institutional drug retail outlets of Gondar Town, North West Ethiopia. Glob Adv Health Med. 2019;8:2164956119868777. doi:10.1177/2164956119868777
32. Spanakis M, Sfakianakis S, Kallergis G, Spanakis EG, Sakkalis V. PharmActa: personalized pharmaceutical care eHealth platform for patients and pharmacists. J Biomed Inform. 2019;100:103336. doi:10.1016/j.jbi.2019.103336
33. Apikoglu S, Selcuk A, Ozcan V, et al. The first nationwide implementation of pharmaceutical care practices through a continuous professional development approach for community pharmacists. Int J Clin Pharm. 2022;14:1–9.
34. Abubakar U, Subramaniam L, Ayinla A. Knowledge, attitude and perception of community pharmacists towards pharmacogenomics services in northern Nigeria: a cross-sectional study. J Pharm Policy Pract. 2022;15(1):39. doi:10.1186/s40545-022-00435-x
35. Al Zaidan M, Mohammed AM, Mohamed Ibrahim MI, Al Mahmoud M, Al Abdulla S, Al-Kuwari MG. Pharmaceutical care service at primary health care centers: an insight on patient satisfaction. Int J Clin Pract. 2022;2022:1–7. doi:10.1155/2022/6170062
36. Belachew SA, Hall L, Selvey LA. Community drug retail outlet staff’s knowledge, attitudes, and practices towards non-prescription antibiotics use and antibiotic resistance in the Amhara region, Ethiopia with a focus on non-urban towns. Antimicrob Resist Infect Control. 2022;11:64. doi:10.1186/s13756-022-01102-1
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
