Back to Journals » Drug, Healthcare and Patient Safety » Volume 12
Assessment of Drug Use Pattern Using WHO Core Prescribing Indicators at Outpatient Settings of Governmental Hospitals in Dessie Town
Authors Mengistu G , Misganaw D , Tsehay T, Alemu BK , Bogale K
Received 29 July 2020
Accepted for publication 11 November 2020
Published 27 November 2020 Volume 2020:12 Pages 237—244
DOI https://doi.org/10.2147/DHPS.S266749
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Siew Siang Chua
Getnet Mengistu,1 Desye Misganaw,1 Tessema Tsehay,2 Belete Kassa Alemu,1 Kassahun Bogale2
1Pharmacology and Toxicology Unit, Department of Pharmacy, College of Medicine and Health Sciences, Wollo University, Dessie, Ethiopia; 2Clinical Pharmacy Unit, Department of Pharmacy, College of Medicine and Health Sciences, Wollo University, Dessie, Ethiopia
Correspondence: Getnet Mengistu
Pharmacology and Toxicology Unit, Department of Pharmacy, College of Medicine and Health Sciences, Wollo University, P.o. Box 1145, Dessie, Ethiopia
Tel +251 912 49 26 92
Fax +251 333115052
Email [email protected]
Background: Enhancing the standards of medical treatment at all levels of the healthcare delivery system can improve the quality of life in developing countries. One method to promote rational drug use is an assessment of drug use pattern based on drug use indicators.
Objective: To evaluate prescription patterns at the outpatient pharmacy of Dessie Referral Hospital and Boru Meda Hospital at Dessie town.
Methods: An institution-based retrospective cross-sectional study was conducted to assess the prescribing patterns in governmental hospitals of Dessie town from April 1 to May 30, 2019. Six hundred eligible prescriptions were selected from each hospital through a systematic random sampling technique.
Results: The result of this study showed that both hospitals used standard prescriptions (100%). Age (99.0%) and name (94.7%) of patients were the most commonly recorded patient information while weight, address of patients and diagnosis were recorded only in 1.1%, 39.2% and 61.3% of the studied prescription papers, respectively. A total 2409 drugs were prescribed in the 1200 prescription papers and the percentage of encounters with injection(s) and antibacterial(s) was 9.0% and 42.6%, respectively. At each hospital, all drugs were prescribed from the Ethiopian essential drug list.
Conclusion: The present study revealed the use of standard presecription papers at both hospitals. None of the patient-related information was completely written in all prescrptions. For drug-related information, only the name of the drug was written in all prescription papers. There is also a significant deviation from the acceptable WHO standard for prescribing antibiotics.
Keywords: prescription pattern, completeness, WHO core prescribing indicators, Dessie, Ethiopia
Introduction
Patients should receive the right medications appropriate to their clinical needs, at the right dose, for the right period, at the lowest possible cost to them and their community.1 Enhancing the standards of medical treatment at any healthcare system can improve the quality of life in developing countries. One method to promote rational drug use is the assessment of drug prescribing patterns based on drug use indicators. Rational drug prescribing is the use of the minimum number of drugs to obtain the best possible effect in the shortest period at a reasonable cost.2 Essential medicines are those that satisfy the priority healthcare needs of the population, selected based on evidence on efficacy and safety, comparative cost-effectiveness and public health relevance.3
Global morbidity and mortality can be reduced by appropriate use of medicines. However, around half of all medicines are prescribed or dispensed inappropriately and more than half of all patients fail to take their medicines as prescribed or dispensed. Such inappropriate use of medicines causes serious adverse events, lack of satisfactory outcome and increased antimicrobial resistance (AMR).4,5 To decrease these problems, the World Health Organization (WHO) developed and validated core drug use indicators for prescribing, patient care and facility-specific studies. The prescribing indicators evaluate the practice of prescribers in five key areas (% of drugs prescribed by generic name, average number of drugs per prescription, % of prescriptions containing antibiotics, % of prescriptions containing injectable drugs, and % of drugs prescribed from the latest edition of national Essential Drug Lists (EDL) or formulary.6
Inappropriate drug use has occurred for as long as medicines have been available. Several choices of therapy are available in treating patients with modern medicines which might be one reason to increase the number of irrational medicine treatment encounters and, ultimately, poor patient outcomes. Common drug use problems include: choosing incorrect medicines, polypharmacy, prescribing the incorrect dose, prescribing medicines that cause adverse drug reactions (ADRs) or drug interactions, and prescribing drugs by brand names which increases the cost for the patient instead of using less-costly generic drugs.7
Prescribing indicators are useful for assessing the prescribing practice of the healthcare delivery system. But, those core indicators fail to assess the completeness of prescriptions (including standards, presence of patient, drug and prescriber and dispenser related information).6 The prescribing pattern of healthcare institutions should be done regularly for forecasting drug use and also to monitor and evaluate drug use.8 So, this study was conducted to assess the prescribing practices in the outpatient settings of Dessie Referral Hospital (DRH) and Boru Meda Hospital (BMH), Dessie town, North-East Ethiopia.
Methods
Study Setting and Period
The study was conducted in two government hospitals of Dessie town, namely: - DRH and BMH from April 1 – May 30, 2019. In the town, there are two public hospitals, seven public health centres, three private hospitals, more than ten speciality clinics and forty-three private drug vendors. DRH is a referral hospital with 560 beds and gives service to more than 70,000 outpatients per year, BMH is a general hospital with more than 200 beds and gives service to more than 40, 000 outpatients per year.
Study Design
A facility-based retrospective cross sectional study was conducted to assess the prescribing practices of DRH and BMH.
Population
All prescriptions dispensed from the out-patient pharmacy of each hospital were taken as source population, and those prescriptions dispensed for a period of one year: 01 January − 31 December, 2018, were taken as study populations.
Selection Criteria
Prescriptions that contained at least one drug for all age groups were included in the study whereas prescriptions that contained only medical supplies, and those with illegible handwriting were excluded from the study.
Sample Size Determination and Sampling Techniques
In the year 2018, 63,211and 38,245 prescription papers were dispensed from OPD pharmacy of DRH and BMH, respectively. These prescription papers were arranged in chronological order and 600 prescription papers that fulfilled inclusion criteria were selected from each hospital based on WHO criteria6 through systematic random sampling technique. The sampling fractions were 105 and 64 for DRH and BMH, respectively.
Data Collection Tool
A customized observational checklist was used to collect the required data for the present study which was prepared using prescribing manuals of the Ethiopian Food and Drug authority (EFDA) and WHO.9,10
Data Quality Control
Data collectors and supervisors were trained by the principal investigators and the data collection checklist was pretested at DRH before commencement of the actual data collection (data not considered for the analysis) and necessary modifications were undertaken. Data was cleaned to remove inconsistencies and missing values on a daily basis.
Data Analysis
Data were entered into EPI-Data Version 3.1 and exported to and analyzed with SPSS version 20.0. Prescribing indicators were computed using the formula adopted by the WHO for prescribing indicators assessment.6 Finally, the data was evaluated against WHO standards and presented in a table.
Results
Patient-Related Information
One thousand two hundred prescription papers (600 from each hospital) were included in the study. Both hospitals used standard prescriptions and 99% of the prescriptions had identification card number. From patient-related information, name (94.7%) and age (93.5%) of the patient were most commonly recorded information, while the weight of the patient was the least recorded patient-related information (Table 1).
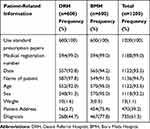 |
Table 1 Presence of Patient-Related Information in Prescriptions Dispensed from Jan to Dec 2018 at Governmental Hospitals of Dessie Town |
Drug-Related Information
Totally 2409 drugs were prescribed from the two hospitals with an average of 2.0 (± 0.25) drugs per prescription. A large proportion of the prescription papers contained one drug (39.2%) followed by two drugs (35.9%). Frequency of administration (93.3%), dose (82.9%) and route of drug administration (82.2%) were the most commonly recorded drug-related information (Table 2).
 |
Table 2 Drug-Related Information on Prescriptions Dispensed from Jan to Dec 2018 at Governmental Hospitals of Dessie Town |
WHO Core Drug Use Indicators
The assessment of prescribing practice using WHO core prescribing indicators revealed that the percentage of encounters with antibacterials and injectables was 42.6% and 9.0%, respectively. From injectables, diclofenac and tramadol were most common from analgesics and ceftriaxone was the most common from antibacterials. The percentage of drugs prescribed with a generic name and from Essential Drug List of Ethiopia was 88.3% and 100%, respectively (Table 3).
 |
Table 3 Prescribing Practice Using WHO Core Prescribing Indicators in Governmental Hospitals of Dessie Town for Drugs Dispensed from Jan to Dec 2018 at the Outpatient Pharmacy Units |
Healthcare Professional Related Information
From 1200 prescription papers, 1036 (86.3%) and 1107 (92.2%) contained the prescribers’ name and signature, respectively. The dispensers’ name and signature were available in 637 (53.1%) and 807 (67.2%) prescription papers, respectively (Table 4).
 |
Table 4 Prescriber and Dispenser’s Information in Prescription Papers Processed from Jan 1 to Dec 31, 2018, at DRH and BMH |
Frequently Prescribed Drugs
Antimicrobials were the most commonly prescribed class of drugs (29.68%) followed by cardiovascular (20.96%) and analgesics and anti-inflammatory agents (19.26%). From a group of antimicrobials, antibacterial agents were the most commonly prescribed drugs (641, 89.65%). Looking at the individual drugs, amoxicillin (22.9%), enalapril (15.84%) and paracetamol (23.06%) were the most prescribed drugs from antibacterial, cardiovascular and analgesics and anti-inflammatory class of drugs, respectively (Table 5).
 |
Table 5 Distribution of Prescribed Drugs Based on Pharmacological Classes from Prescriptions Dispensed During Jan 1 to Dec 31, 2018 at the Outpatient Pharmacy Units of DRH and BMH |
Discussions
Indicators of prescribing practices can be used to measure the performance of healthcare providers in fostering the appropriate use of drugs. The drug use indicators can serve to focus attention on one or two aspects of performance, narrowing down the area of subsequent inquiry.6 Assessing the prescribing practice of health institutions can be used as baseline data for further interventional studies.11
In the present study medical registration number, date, name, age and sex of patient was mentioned in more than 92% of prescription papers included the study. It is expected that all prescription papers should bear all these components for rational dispensing, but none of these variables were mentioned in 100% of the prescription papers. For example, percentage of prescription papers on which date was written were 93.5%; which was relatively higher than findings from previous similar studies conducted in Ethiopia and different parts of the world which reported a percentage of 16.1 to 89.4%.12–17 Date should be written on all prescription papers for retrieval and legal purposes. In this study, on the other hand, name of patient was mentioned in 94.7% of the prescription papers which is comparable with findings from similar studies conducted in Jimma and Harar, Ethiopia which reported 93.3% and 93.9%, respectively.13,18 However, it is higher than a study conducted at Gondar, Ethiopia14 and lower as compared to other study findings.12,15–17 Prescribers should be aware of the importance of writing name of patient in every single prescription paper as it is important in patient identification during the dispensing process. In our study, the percentage of prescription papers with age written was 93.5% which is in line with a study conducted at Bahir Dar, Ethiopia where a percentage of 92.6% is reported.15 The result is, however higher than similar study findings conducted in Ethiopia and India,14,19,20 and lower compared to other similar studies conducted elsewhere.12,16,17 Age is an important variable implicated in dose calculations and selection of appropriate dosage forms, particularly for the pediatric population. Regarding sex of patients, 93.2% of prescription papers in the present study revealed sex, a finding higher than findings from similar studies13–15,20 and lower than some other studies conducted in Ethiopia and beyond.12,16,17 In the present study, weight of patients was recorded in only 1.1% of the prescription papers, which is a very poor practice revealed by the investigators. This finding is comparable with findings reported from previous Ethiopian studies which reported a percentage from 0 to 1%.12,13,15,17 One Ethiopian study, however reported a higher result, 7.3%.16 Failure to write weight of patients may be due to inadequate availability of weighing balance to the prescribers in the study settings. Weight of patients is also important for pharmacists to evaluate doses. Only 39.2% prescription papers recruited in our study revealed address of patients. Though this itself is poor practice, this finding is a much better practice compared to seven similar study findings from different parts of Ethiopia which reported a practice of <21%.12–18
In this study, diagnosis was recorded in 61.3% of the prescription papers recruited from DRH and BMH. This may be due to lack of confidence and skill of prescribers in confirming the exact diagnosis of a disease. It could also be as a result of inadequate/non-availability of laboratory and other investigation facilities in the study settings. This finding is higher compared to findings from similar studies conducted in Ethiopia and Sudan.12–19,21 Pharmacy professionals will be unable to evaluate prescription orders if prescribers fail to write diagnosis on prescription papers, hence they should write diagnosis on every single prescription paper to promote optimal therapeutic patient outcomes.
Regarding pharmacotherapy regimens, the present study identified that all the included prescription papers contained name of drugs which is an excellent practice. But, dose of drugs were written in only 82.9% of prescription papers; which is lower than findings from Dilla, Ethiopia (94.9%) and Jimma, Ethiopia (89.8%) but higher than many findings from similar studies conducted in Sudan and Ethiopia which reported a range between 27.4% and 81.2%.13–17,19 Four hundred twenty four (17.6%) prescription papers revealed type of dosage forms which is in line with a finding from Mizan, Ethiopia (17.9%).16 However, the finding is lower as compared to the study done in Harar (32.7%) and higher than a finding from Bahir Dar, Ethiopia (8.3%) and Jimma Ethiopia (11.45%).13,17,18 In the present study, route of drug administration was written in 82.2% of prescription papers which is relatively comparable with previous findings from Harar, Ethiopia (81.8%) but lower compared to other similar studies which reported between 87.6–93.1%.12,16,18 About 93.3% prescription papers revealed frequency of drug administration, which is higher than previous similar studies conducted at different corners of Ethiopia with a percentage report of 6.4–92.2%.12–18 Percentage of prescription papers with duration of treatment mentioned was 80.1%, a finding comparable with the study conducted in Gondar, Ethiopia (82%).14 However, this finding is higher than findings from other studies (20–74.6%).12,13,15–17,20 Prescribers should be curious enough to write complete pharmacotherapy regimen so as to enable pharmacy professionals to evaluate the appropriateness of therapeutic orders. This in turn has significant effect on optimal therapeutics patient outcomes.
In the present study, possible causes for prescribers’ failure to write every component of a standard prescription order might include: patient load, failure to appreciate the importance of writing every component, negligence, and/or unavailability of measuring device nearby to them. Even though every component of a prescription paper may not serve equally, writing every single bit information is a professional requirement. Hence, besides prescribers own responsibility, all other stakeholders, including pharmacy professionals should be involved in assuring the completeness of every single prescription paper.
In the present study, a total of 2409 drugs were prescribed for 1200 patients who visited the outpatient pharmacy of DRH and BMH which give rise to an average of 2.01 drugs prescribed per encounter which is higher than the WHO standard (1.6–1.8)6 and also findings from similar studies conducted in many parts of Ethiopia which reported average number of drugs per encounter between 1.64 and 1.9.12,14,15,17,22–25 On the other hand, this finding is lower than many other study findings which identified an average value of 2.17–4.18 drugs per encounter.1,13,19–21,26–38 Polypharmacy may expose patients to ADRs and will incur additional costs on patients and hence prescribers should be limited prescribing drugs when only necessary. In this study, percentage of encounters prescribed at least with one antibiotics was 43%, which is much higher than the standard set by the WHO (20–26.8%),6 revealing overuse of antibiotics. Similar studies conducted in various countries found percentage of encounters with antibiotics to be between 9.1–42.04% which is lower than the finding reported by the present study.1,14,15,17,26,27,29,32,33,36 On the contrary, the finding was lower than other similar study findings (48.9–75.1%).12,13,19–25,28,30,31,34,35,37,38 Antimicrobial resistance is at the edge of indiscriminate antibiotics prescribing practice which is a pressing global problem nowadays impacting infection control efforts and costs of antimicrobial treatment, among others. Prescribers should limit themselves from over prescribing these type of drugs. Percentage of drugs prescribed by generic name in the present study was 88.3% which is less than the WHO standard, requiring all drug prescriptions to be written in generic names.6 This finding is higher than many findings reported from studies conducted in different countries1,12,17,20,29–31,33–36,38 and lower than some other study findings.13–15,22–28,32 Brand name prescription may be costly for patients, hence prescribers are encouraged to prescribe drug names in generics. In the present study, percentage of encounters with injectables was 9%, which falls below the standard set by WHO (13.4–24.1%).6 Many similar studies reported a higher percentage of injectables prescribed per encounter beyond this standard.12–14,17,19,22,23,30 On the other hand WHO requires that every drug should be prescribed from the Essential Drug List (EDL); in the present study all drugs were prescribed from the EDL of the country in line with findings from similar studies conducted in UAE and Ethiopia.15,27
Even though this study tried to address several aspects of prescription practice beyond the usual indicator studies, it has several limitations. First, since it is a retrospective study, there were several incomplete documentations, for example, the authors were not able to find out how prescriptions without name of patients were dispensed. Second, it is a descriptive study which showed only the magnitude of the problem without identifying the underlying causes of problems identified.
Conclusions
The present study revealed the use of standard presecription papers at both hospitals. No patient-related information was completely written in all prescrptions. From drug-related information, only the name of the drug was written in all prescription papers. There is also a significant deviation from the acceptable WHO standard in prescribing antibiotics.
Abbreviations
ADR, adverse drug reaction; AMR, antimicrobial resistance; BMH, Borumeda Hospital; DRH, Dessie Referral Hospital; EDL, Essential Drug List; WHO, World Health Organization.
Data Sharing Statement
All the data used for the study is contained within the manuscript.
Ethics Approval and Consent to Participate
The ethical clearance and study approval was obtained from Wollo University, College of Medicine and Health Sciences, Research and Ethics Committee. Since the study was a retrospective study, patient consent to review their medical records was not required by the Research and Ethics Committee of the college. Names of study participants were omitted from the data collection format to keep the privacy of study participants and the confidentiality of their personal information was kept according to the Declaration of Helsinki.
Acknowledgments
We would like to acknowledge Wollo University for providing a fund. We also would like to extend our gratitude for administrators and pharmacists of DRH and BMH who helped us a lot in facilitating data collection. Our deep appreciation also goes to data collectors.
Author Contributions
All authors contributed in conceiving the original idea, drafting the proposal and were also involved in data acquisition, data analysis, drafting and revising the manuscript, have agreed on the journal to which the article will be submitted, gave final approval of the version to be published and agreed to be accountable for all aspects of the work.
Funding
This study was funded from a research grant of Wollo University for the year 2018/19.
Disclosure
The authors declare that they have no conflicts of interest.
References
1. Angamo MT, Wabe NT, Raju N. Assessment of patterns of drug use by using World Health Organization’s prescribing, patient care and health facility indicators in selected health facilities in Southwest Ethiopia. J Appl Pharm Sci. 2011;1(7):62.
2. Shankar RP, Partha P, Shenoy NK, Easow JM, Brahmadathan KN. Prescribing patterns of antibiotics and sensitivity patterns of common microorganisms in the Internal Medicine ward of a teaching hospital in Western Nepal: a prospective study. Ann Clin Microbiol Antimicrob. 2003;2(1):7. doi:10.1186/1476-0711-2-7
3. Tripathy K. Essentials of Medical Pharmacology.
4. Holloway KA. Combating inappropriate use of medicines. Expert Rev Clin Pharmacol. 2011;4(3):335–348. doi:10.1586/ecp.11.14
5. Lu Y, Hernandez P, Abegunde D, Edejer T. The World Medicines Situation 2011. Medicine Expenditures. Geneva: World Health Organization; 2011.
6. WHO. How to investigate drug use in health facilities: selected drug use indicators. 1993. Available from: http://apps.who.int/medicinedocs/en/d/Js2289e.
7. WHO. The world medicines situations: chapter 8, rational use of medicines. 2010. Available from: http://apps.who.int/medicinedocs/en/d/JS/6160e/10.html.
8. Roughead EE, Lhazeen K, Socialine E, Bahri S, Park BJ, Holloway K. Monitoring medicines use to support national medicines policy development and implementation in the Asia Pacific region. WHO South-East Asia j Public Health. 2013;2(2):113. doi:10.4103/2224-3151.122946
9. FMHACA. Manual for Medicines Good Prescribing Practice. Addis Ababa: Food, Medicine and Healthcare Administration and Control Authority of Ethiopia; 2012. Available from: http://apps.who.int/medicinedocs/documents/s22353en/s22353en.pdf.
10. WHO. Guide to Good Prescribing - a Practical manual:World Health Organization Action Programme on Essential Drugs. Geneva: WHO/DAP/94.11; 1994.
11. West SL, Strom BL, Freundlich B, Normand E, Koch G, Savitz DA. Completeness of prescription recording in outpatient medical records from a health maintenance organization. J Clin Epidemiol. 1994;47(2):165–171. doi:10.1016/0895-4356(94)90021-3
12. Bekele NA, Tadesse J. Prescription auditing based on world health organization (WHO) prescribing indicators: a case of Dilla university referral hospital. J Drug Del Ther. 2018;8(6–s):21–25. doi:10.22270/jddt.v8i6-s.2165
13. Gashaw T, Sisay M, Mengistu G, Amare F. Investigation of prescribing behavior at outpatient settings of governmental hospitals in eastern Ethiopia: an overall evaluation beyond World Health Organization core prescribing indicators. J Pharm Pol Pract. 2018;11(1):26. doi:10.1186/s40545-018-0152-z
14. Admassie E, Begashaw B, Hailu W. Assessment of drug use practices and completeness of prescriptions in Gondar University Teaching Referral Hospital. Int J Pharm Sci Res. 2013;4(1):265.
15. Asrade B. Assessment of completeness of prescription and rational drug use practice at Felege Hiwot Referral Hospital, North West Ethiopia. Assessment. 2019;60.
16. Ayele T, Tsehay T, Bedada H. Prescribers’ adherence to the basic principles of prescription order writing in a teaching hospital, Ethiopia. Indo Am J Pharm Res. 2017;7(8):499–503.
17. Yilma Z, Mekonnen T, Siraj EA, et al. Assessment of prescription completeness and drug use pattern in Tibebe-Ghion comprehensive specialized Hospital, Bahir Dar, Ethiopia. Biomed Res Int. 2020;2020.
18. Melaku T, Molla G. Assessment of prescribers’ adherence to the basic standards of prescription order writing in jimma university specialized Hospital, Southwest Ethiopia. Southwest Ethiopia: The Experiment. 2014;19(1):1316–1329.
19. Rabie D, Kheder SI. Assessment of prescribing and dispensing practices based on WHO core prescribing indicators in hospital and community pharmacies in Khartoum State-Sudan. J Med Inf Decision Making. 2020;1(3):1. doi:10.14302/issn.2641-5526.jmid-20-3493
20. Shelat PR, Kumbar SK. Analysis of out door patients’ prescriptions according to World Health Organization (WHO) prescribing indicators among private hospitals in Western India. J Clin Diagn Res. 2015;9(3):FC01.
21. Lenjisa JL, Fereja TH. A retrospective analysis of prescribing practices through WHO prescribing indicators at four selected hospitals of West Ethiopia. J Bioanal Biomed. 2014;6(2):29.
22. Desalegn AA. Assessment of drug use pattern using WHO prescribing indicators at Hawassa University teaching and referral hospital, south Ethiopia: a cross-sectional study. BMC Health Serv Res. 2013;13(1):1–6. doi:10.1186/1472-6963-13-170
23. Getachew T, Tadiwos Y, Sisay M. Evaluation of the prescribing practice using WHO core prescribing indicators in Hiwot Fana Specialized University Hospital, Harar, eastern Ethiopia. J Drug Del Ther. 2016;6(6):25–30. doi:10.22270/jddt.v6i6.1344
24. Dessie B, Atalaye G, Diress E, Getahun A. Practice towards rational drug use at Finotselam and Asirade Zewudie Hospitals based on WHO core drug use indicators, Northwest Ethiopia. Sci World J. 2020;2020.
25. Kasahun G, Demoz G, Asayehegn A, Gebrehiwot L, Tesfay G, Desta D. Evaluation of pattern of drug use in tertiary health care setting in central Tigray Using WHO prescribing indicators. Adv Pharmacoepidemiol Drug Saf. 2020;9(228):1052–2167.
26. Akl OA, El Mahalli AA, Elkahky AA, Salem AM. WHO/INRUD drug use indicators at primary healthcare centers in Alexandria, Egypt. J Taibah Univ Med Sci. 2014;9(1):54–64. doi:10.1016/j.jtumed.2013.06.002
27. Mahmood A, Elnour AA, Ali AAA, Hassan NA, Shehab A, Bhagavathula AS. Evaluation of rational use of medicines (RUM) in four government hospitals in UAE. Saudi Pharm J. 2016;24(2):189–196. doi:10.1016/j.jsps.2015.03.003
28. Mariam AH, Raghavendra Y, Bobasa EM. Evaluating rational drug use with the help of World Health Organization’s core indicators in Bule Hora Hospital, Southern Ethiopia. encounters. 2015;7(8):11.
29. Al-Azayzih A, Al-Azzam SI, Alzoubi KH, Shawaqfeh M, Masadeh MM. Evaluation of drug-prescribing patterns based on the WHO prescribing indicators at outpatient clinics of five hospitals in Jordan: a cross-sectional study. Int J Clin Pharmacol Ther. 2017;55(5):425–432. doi:10.5414/CP202733
30. Atif M, Sarwar MR, Azeem M, Naz M, Amir S, Nazir K. Assessment of core drug use indicators using WHO/INRUD methodology at primary healthcare centers in Bahawalpur, Pakistan. BMC Health Serv Res. 2016;16(1):684. doi:10.1186/s12913-016-1932-2
31. Atif M, Sarwar MR, Azeem M, et al. Assessment of WHO/INRUD core drug use indicators in two tertiary care hospitals of Bahawalpur, Punjab, Pakistan. J Pharm Pol Pract. 2016;9(1):27. doi:10.1186/s40545-016-0076-4
32. Chijioke-Nwauche I, Akodo J. Evaluation of drug use pattern in Lulu Brigg’s Health Centre, University of Port Harcourt, Nigeria using WHO, prescribing indicators. The Pharmainnovation J. 2017;6:506–510.
33. El Mahalli A. WHO/INRUD drug prescribing indicators at primary health care centres in Eastern province, Saudi Arabia. Eastern Mediterranean Health J. 2012;18(11):1091–1096.
34. Enato EF, Chima IE. Evaluation of drug utilization patterns and patient care practices. West Afr J Pharm. 2011;22:1.
35. Otoom S, Batieha A, Hadidi H, Hasan M, Al Saudi K. Evaluation of drug use in Jordan using WHO prescribing indicators. Eastern Mediterranean Health J. 2002;8(4–5):537–543.
36. Prasad PS, Rudra JT, Vasanthi P, Sushitha U, Sadiq MJ, Narayana G. Assessment of drug use pattern using World Health Organization core drug use indicators at Secondary Care Referral Hospital of South India. CHRISMED J Health Res. 2015;2(3):223. doi:10.4103/2348-3334.158683
37. Sisay M, Mengistu G, Molla B, Amare F, Gabriel T. Evaluation of rational drug use based on World Health Organization core drug use indicators in selected public hospitals of eastern Ethiopia: a cross sectional study. BMC Health Serv Res. 2017;17(1):1–9.
38. Yousif BME, Supakankunti S. General practitioners’ prescribing patterns at primary healthcare centers in National Health Insurance, Gezira, Sudan. Drugs-Real World Outcomes. 2016;3(3):327–332. doi:10.1007/s40801-016-0087-0
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
