Back to Journals » Patient Preference and Adherence » Volume 17
Assessing the Validity of Health Messages Used by the Saudi Public in WhatsApp
Authors Alfaris E , Alhazzani Y, Alkhenizan A, Irfan F, Almoneef N, Alyousefi N , Alfaris H, Alodhaibi K , Ahmed MA
Received 15 November 2022
Accepted for publication 24 December 2022
Published 6 January 2023 Volume 2023:17 Pages 67—73
DOI https://doi.org/10.2147/PPA.S397661
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Eiad Alfaris,1 Yasser Alhazzani,1 Abdullah Alkhenizan,2 Farhana Irfan,1 Naif Almoneef,2 Nada Alyousefi,3 Huda Alfaris,4 Khitam Alodhaibi,2 Abdullah MA Ahmed1
1Department of Family and Community Medicine, College of Medicine, King Saud University Chair for Medical Education Research and Development, King Saud University, Riyadh, Saudi Arabia; 2King Faisal Specialist Hospital and Research Center, Family Medicine and Polyclinics, Riyadh, Saudi Arabia; 3Department of Family and Community Medicine, College of Medicine, King Saud University, Riyadh, Saudi Arabia; 4Prince Sultan Military Medical City, Department of Internal Medicine, Riyadh, Saudi Arabia
Correspondence: Eiad Alfaris, King Saud University Chair for Medical Education Research and Development, Department of Family and Community Medicine (34), College of Medicine, King Saud University, PO Box 2925, Riyadh, 11461, Saudi Arabia, Email [email protected]; [email protected]
Objective: WhatsApp is the most frequently used social media platform in Saudi Arabia. Inaccurate information could negatively impact public health. The number of studies worldwide investigating health-related misinformation in social media increased steadily, with limited data from Arabic-speaking communities. This study aimed to estimate the validity and safety of Arabic-language health information messages circulated on WhatsApp and identify the different categories of these messages based on their credibility.
Participants and Methods: A descriptive, analytical cross-sectional study was conducted from February to April 2021. A total of 374 students were randomly selected from the common first preparatory year college at King Saud University in Riyadh, Saudi Arabia, and participated by sharing up to three health-related WhatsApp messages per student that they or their relatives had recently read. Four board-certified physicians reviewed and classified the messages based on their credibility and sources.
Results: 282 students provided 326 messages (1.2 messages per student). Most messages (86%) had either invalid or inaccurate content, and 83.7% came from unknown sources. Only 26 messages (8%) of the total were written by trusted scientific sources. Most of the messages from unknown sources or unqualified persons were either invalid or invalid, with potential health risks for the public, and the difference from trusted sources was statistically significant.
Conclusion: This study showed a high percentage of inaccurate and invalid health-related messages on WhatsApp. Invalid messages with potential health risks were authored mostly by unknown sources or unqualified persons. Most health messages written by trusted authorities and qualified persons were valid. Trusted scientific authorities should thus be more active in public education on social media platforms. They should advise their communities on how to discern the validity of such messages. More efforts are needed to guide patients from where to obtain accurate and valid health information.
Keywords: health information, WhatsApp, Saudi Arabia, social media
Introduction
Social media’s use for health-related purposes has steadily expanded throughout the world. Literature shows that almost 56–80% of internet users utilize Social media for health information online, with variability in the topics among different population demographics.1,2 Social media channels can easily provide efficient, user-friendly platforms for receiving and providing healthcare information, making the mass dissemination of health information possible.3
According to the latest report from the Saudi communications and information technology commission, internet usage by Saudi citizens continued to rise from 94.3% in 2017 to about 98.1% in 2021 in Saudi Arabia.4 The most common internet devices in Saudi Arabia were mobile phones (98%), followed by computers (42.79%), and then tablets (30.96%).5 The most used social media platform in Saudi Arabia is WhatsApp (89.9%).5 About 34.5% of internet users use it to search for health-related information.5
Alassiri et al found that two-thirds of the Saudi population preferred social media as a source of health information, especially WhatsApp, which represents 90% of usage rate.2,6 Younger generations and women have been shown to be the most frequent seekers of health information on the internet in Saudi Arabia.2 However, patients visiting Saudi primary care clinics were aware of the unreliability of health information on Social media, considering WhatsApp not to be a trusted source for such content.7 About two third of physicians in Saudi Arabia did not interact with their patients through social media.8
Social media platforms contain extensive information, making it challenging to filter out false or inaccurate information that could negatively impact public health making health-related Social media messages a potentially useful infodemiology indicator.9 This allowed radical movements such as anti-vaccination groups to flourish and spread their agendas.10 Health professionals struggle regarding how to intervene when health-related information is misdirected by falsification and is inconsistent with evidence-based medicine.9 They can no longer control or “gate-keep” the information communicated through Social media.11,12
The number of studies worldwide investigating health-related misinformation increased around six times from 7 in 2012 to 41 in 2018.10 Of 414 records included in an Australian bibliometric study aimed to report on concept mapping of infodemic literature, identified Infodemic fabrication context and evaluation as impactful future direction research.13
Measuring the extent of health related infodemic is important in order to implement appropriate interventions to protect the public from the negative psychological and social impacts of social media.10 A study analyzed 232 pieces of misinformation published by the Brazilian fact-checking service related to coronavirus into categories: Misleading; Fabricated; False, or Parody.14 Most of it was found to be fabricated (53%).14 Access to the correct information, at the right time, in the right format is critical.
A study in India assessed participants’ opinions on the accuracy of WhatsApp messages related to coronavirus using a scoring system designed by the authors to calculate the risk of the user getting exposed to, accepting, acting on, or sharing unverified messages.15 It found that users over 65 and unskilled workers were most vulnerable to misinformation spread via WhatsApp.15
Alshareef and Alotiby found that Saudi people accept sharing health information without evidence on social media, believing that sharing is harmless, although they were aware of their unreliability.16 WhatsApp was the most preferred social media platform.16
In Arabic-speaking communities, research on the validity/safety and credibility of WhatsApp health information is scarce. This study hypothesized that either unknown or unqualified persons wrote a large proportion of health-related messages and that most messages were invalid. It aimed to estimate the validity and safety of Arabic-language health information messages circulated on WhatsApp and identify the different categories of these messages based on their credibility.
Materials and Methods
A descriptive, analytical cross-sectional study was conducted through analyzing the content of messages on the WhatsApp social media platform. Students from the Common First preparatory year at King Saud University (KSU) participated by filling out an electronic questionnaire and providing samples of health-related messages. The preparatory year consists of three tracks: health, engineering, science, and humanities.
The inclusion criteria were as follows: currently a student in the Common First preparatory year at KSU (both genders) and in any of the three specialties mentioned earlier. Students from outside KSU were excluded. To be included in the study, the messages were required to be written in Arabic as it is the official and mother tongue of Saudi citizens. Exact duplicate (similar) messages submitted by more than one student and non–health-related messages were excluded.
The sample size was calculated using the Raosoft website, assuming a margin of error of 5% and a confidence level of 90%. It was found to be 267 participants. With an expected non-response rate of 30%, 374 students were invited to participate in the study. Participants were requested to share up to three health-related WhatsApp messages that they had recently read. Examples of such messages are the benefit of stem cells or different herbs for certain diseases and risk factors or causes for diseases and ailments. For instance, one message indicated that Bell’s palsy is caused by or related to direct exposure to air conditioners.
After obtaining the students’ email addresses from the deanship of the Common First preparatory year, the Google form was sent electronically to a randomly selected sample of students. At the beginning of the form, there was an introductory note including the title, aims, and importance of the study; it appealed for participants’ professionalism to fill out the instrument diligently. They were requested to indicate their gender and to provide three health-related WhatsApp messages that they (or one of their relatives) had recently read. Students’ identities were concealed, assuring participants’ anonymity. Informed consent to participate was also obtained.
The four consultants (reviewers) selected to review the messages were board-certified family medicine or internal medicine. The WhatsApp pieces of health information were collected between February and April 2021. Each message was independently reviewed for accuracy by two reviewers based on available scientific evidence. Any disagreement between the two independent reviewers was resolved by the other two reviewers (through consensus), who were blinded to the decision of the first reviewers. Inter-rater reliability with Kappa was not calculated. The information in each message was judged and classified as follows:
Credibility has four categories: Unknown source, known source —unqualified person, known source —a qualified person (healthcare worker), or known source —a trusted scientific body (authority). Validity (Accuracy and safety) has four categories: Valid—contains correct information supported by evidence; inaccurate—contains mixed information (correct and incorrect); invalid with no potential health risk; or Invalid with potential health risk. The categorization of the messages and content analysis was inspired by Park et al analysis of colorectal cancer information on Twitter and its credibility,17 and Biancovilli et al analysis of misinformation published in social media about coronavirus in Brazil.14
The data was entered in an excel sheet. Then were analyzed using IBM SPSS Statistics for Windows version 22.0 (IBM Corp, Armonk, New York, USA). Descriptive statistics such as frequency, percentages, means, and standard deviations were used to describe the composition of the sample. Different categorical variables were compared using chi-square and Fisher’s exact tests as appropriate. A p-value of less than 0.05 was considered significant.
The required ethical approval was obtained from the institutional review board of KSU (IRB Research Project No.- E-20-5011).
Results
Among the 374 students who were invited, 282 (75.4%) agreed to participate. Sixty-three percent (63%) of the students who participated in this study were female. The number of reviewed messages was 326. The average number of messages collected per student was 1.2, as some students submitted one or two messages only.
Around 280 (86%) of the studied messages were either invalid with or without potential risk (63.2%) or inaccurate (22.4%), and only 14.4% were valid (Figure 1). Most of the messages (83.7%) were from unknown sources. Messages authored by qualified persons (5.8%) or trusted scientific sources (2.1%) represented only 8% of the total messages (Figure 2 and Table 1).
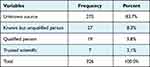 |
Table 1 Distribution of Messages Based on Their Sources’ Credibility |
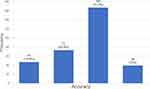 |
Figure 1 Distribution of messages according to their validity. |
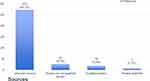 |
Figure 2 Distribution of messages credibility according to their sources. |
Two-thirds, 186 (68%) of the 237 messages authored by an unknown source, were either invalid or invalid with potential risk. A similar pattern was found for the 17 messages (63%) written by unqualified persons. All scientific authorities’ messages were valid and safe (100%). A statistically significant association was found between the messages’ sources’ credibility and their validity (p-value < 0.05) (Table 2).
 |
Table 2 Association Between Messages Sources Credibility and Validity (Accuracy and Safety) |
Discussion
This study sheds light on the validity (accuracy and safety) of health information circulated on WhatsApp in Arabic among Saudi people. Most of the health-related messages in the current study (84%) were authored by unknown sources and were either inaccurate or invalid. Furthermore, 12% of them posed a potential health risk. A systematic review of published data found that misinformation was more popular than accurate information. The finding that most health-related messages were invalid and that most inaccurate information came from unqualified individuals10 was in line with the literature18–20 and is consistent with a recent US study that found seven out of ten articles shared on social media platforms pertaining to prostate cancer to be inaccurate or misleading.21 Similarly, a study from Poland showed that 40% of health messages were inaccurate or untrue.18
The risks of invalid information are significant, as they may cause serious harm to patients22—for example, an Australian study found that 42% of patients discontinued their treatment based on advice from Social media messages.23 Such health information sought from various sources tremendously influences not only individuals’ trust of their physicians’ judgment but also the medical system.
The low involvement of credible sources in patients’ education in social media in the current study is in line with another Saudi study.8 Although studies have identified an improvement in health promotion and adherence to medical advice after social media education,24–26 only half of persons discussed social media health information topics with their physicians in a US study.2
The current study found an alarming rate of invalid and inaccurate messages indicating an infodemic (epidemic of misinformation). It was found that false information is diffused faster and more broadly than valid information.9,27 It is likely that reading “exciting” or fear arousing information is more appealing to the public as reported in a Saudi study among physicians, the public, and the journalists.28 A study investigating the sharing of misinformation by subscribers to a fact-checking newsletter found that around one-quarter of the participants had shared possible fake news or misinformation regarding COVID-19; the poor belief in science could predict this attitude.29
Finding solutions to this problem is an urgent matter. The question is, what should the healthcare authorities do to control the situation? Identifying and tracking inaccurate/invalid messages with potential risk is difficult.7,10 A perfect solution to this challenge may not exist, but achieving something better than the present is a worthy goal.30 Establishing regulations within the system to reduce media misinformation is a challenge for policymakers and regulators. There is a need for academic, scientific, and healthcare professionals to collaborate with the social media industry and consumer representatives to counter the negative impact of media misinformation.10 Furthermore, health practitioners have a crucial role in proactively exploring infodemics,31 disseminating evidence-based information29,31,32 to equip individuals with the ability to critically assess social media information’s credibility to enhance patients’ well-being and satisfaction and improve health outcomes.33
The Ministry of Health in Saudi Arabia exerts a commendable effort to educate and empower the public to provide high-quality information. More expenditure on health literacy rather than efforts to debunk pieces of misinformation on social media may create improvement. Scientific and medical alliances with social media companies can offer a chance to have advisory/think tanks (experts) who can monitor, give opinions on a given subject, and share credible health information.30 The content of social media educational messages should be tailored to suit the target audience, considering people’s values and the relevant cognitive, emotional, sociocultural, and contextual factors.28,34
Health organizations can use social media to dialogue with patient communities following the code of ethics, rather than using these platforms only to broadcast information.29,32 Physicians and organizations should be vigilant in monitoring and evaluating public health advocacy and communication on various popular social media websites.9,35 Efforts can be directed towards the use of all applications to ensure people are directed to a reliable source, such as the ministry of health, WHO website, etc., when they search.36
Some developed countries have utilized various approaches to solve these issues. At a government level, a hotline can operate where the public and healthcare professionals report any misinformation circulating in the media. Another area that can be used is crowdsourcing trusted ratings for consumer evaluation.37 The direction given is limited as it offers a starting point; for what should be an ongoing process. It needs to be regularly revisited and updated with time in accordance with the changes in the information ecosystem.
Limitations
Some participants sent only one or two messages; some were repeated or not health-related. The study examined the shared messages only on the WhatsApp platform. Additionally, the study involved health messages read by the relatives of students of one academic year in one institute without collecting their demographic characteristics. Future work should address user demographic features. The study results cannot be unduly generalized due to its’ limitations. Despite these limitations, the present study highlighted an important area of public healthcare and patient safety in the Saudi community.
Conclusion
The results of this study showed a high rate of inaccurate and invalid health-related messages on WhatsApp. Very few messages were authored by trusted scientific authorities or qualified health professionals. Therefore, we recommend that trusted scientific authorities and qualified persons post health messages on social media platforms to clarify to the public where to obtain accurate and valid health information. We believe this research could play an important role in promoting public awareness of WhatsApp health messages and providing better patient education by analyzing the source and credibility of real-time public information. The present study should be followed by future more representative studies that enable comparisons between different sociodemographic groups.
Abbreviations
SM, social media; KSU, King Saud University.
Acknowledgment
The authors extend their appreciation to the Deanship of Scientific Research, King Saud University, for funding through the Vice Deanship of Scientific Research Chairs, The King Saud University research chair of medical education. The funding organization has no interest in any direction of the study and as expected, did not have any role in the survey’s design, implementation, and analysis.
Disclosure
The authors report no conflict of interest in this study. The manuscript or its contents is not previously published in partial or full in any website or any printed journal in English or any other language.
References
1. Marar SD, Al-Madaney MM, Almousawi FH. Health information on social media.: perceptions, attitudes, and practices of patients and their companions. Saudi Med J. 2019;40(12):1294. doi:10.15537/smj.2019.12.24682
2. El Kheir DYM, Boumarah DN, Bukhamseen FM, Masoudi JH, Boubshait LA. The Saudi experience of health-related social media use: a scoping review. Saudi J Heal Syst Res. 2021;11–12.
3. Gabarron E, Bradway M, Fernandez-Luque L, et al. Social media for health promotion in diabetes: study protocol for a participatory public health intervention design. BMC Health Serv Res. 2018;18(1):1–5. doi:10.1186/s12913-018-3178-7
4. Saudi Communications and Information Technology Commission. Annual report; 2021. Available from: https://www.cst.gov.sa/ar/indicators/PublishingImages/Pages/saudi_internet/internt-saudi-2021.pdf.
5. Saudi Communications and Information Technology Commission. Saudi internet; 2021. Available from: https://www.cst.gov.sa/ar/indicators/PublishingImages/Pages/saudi_internet/internt-saudi-2021.pdf.
6. Alassiri SA, Alowfi AS. Public’s attitudes toward health information on Twitter: a cross-sectional survey based on the Saudi population. Cureus. 2019;11:10.
7. Alduraywish SA, Altamimi LA, Aldhuwayhi RA, et al. Sources of health information and their impacts on medical knowledge perception among the Saudi Arabian population: cross-sectional study. J Med Internet Res. 2020;22(3):e14414. doi:10.2196/14414
8. Alanzi T, Al-Yami S. Physicians’ attitude towards the use of social media for professional purposes in Saudi Arabia. Int J Telemed Appl. 2019;2019. doi:10.1155/2019/6323962
9. Chou W-YS, Oh A, Klein WMP. Addressing health-related misinformation on social media. JAMA. 2018;320(23):2417–2418. doi:10.1001/jama.2018.16865
10. Wang Y, McKee M, Torbica A, Stuckler D. Systematic literature review on the spread of health-related misinformation on social media. Soc Sci Med. 2019;240:112552. doi:10.1016/j.socscimed.2019.112552
11. Nursan C, Dilek K, Sevin A. A autoeficácia das mães quanto à lactância e os fatores que a afetam. Aquichan. 2014;14(3):327–335. doi:10.5294/aqui.2014.14.3.5
12. Pottie K, Ratnayake A, Ahmed R, Veronis L, Alghazali I. How refugee youth use social media: what does this mean for improving their health and welfare? J Public Health Policy. 2020;41(3):268–278. doi:10.1057/s41271-020-00231-4
13. Pool J, Fatehi F, Akhlaghpour S. Infodemic, misinformation and disinformation in pandemics: scientific landscape and the road ahead for public health informatics research. In: Public Health and Informatics. IOS Press; 2021:764–768.
14. Biancovilli P, Makszin L, Jurberg C. Misinformation on social networks during the novel coronavirus pandemic: a quali-quantitative case study of Brazil. BMC Public Health. 2021;21(1):1–10. doi:10.1186/s12889-021-11165-1
15. Bapaye JA, Bapaye HA. Demographic factors influencing the impact of coronavirus-related misinformation on WhatsApp: cross-sectional questionnaire study. JMIR Public Heal Surveill. 2021;7(1):e19858. doi:10.2196/19858
16. Alshareef M, Alotiby A. Prevalence and perception among Saudi Arabian population about resharing of information on social media regarding natural remedies as protective measures against COVID-19. Int J Gen Med. 2021;14:5127. doi:10.2147/IJGM.S326767
17. Park S, Oh H-K, Park G, et al. The source and credibility of colorectal cancer information on twitter. Medicine. 2016;95(7):1.
18. Waszak PM, Kasprzycka-Waszak W, Kubanek A. The spread of medical fake news in social media–the pilot quantitative study. Heal Policy Technol. 2018;7(2):115–118. doi:10.1016/j.hlpt.2018.03.002
19. Bin NS, Bhatti R, Khan A. An exploration of how fake news is taking over social media and putting public health at risk. Heal Inf Libr J. 2021;38(2):143–149. doi:10.1111/hir.12320
20. Islam MS, Sarkar T, Khan SH, et al. COVID-19–related infodemic and its impact on public health: a global social media analysis. Am J Trop Med Hyg. 2020;103(4):1621. doi:10.4269/ajtmh.20-0812
21. Alsyouf M, Stokes P, Hur D, Amasyali A, Ruckle H, Hu B. ‘Fake news’ in urology: evaluating the accuracy of articles shared on social media in genitourinary malignancies. BJU Int. 2019;124(4):701–706. doi:10.1111/bju.14787
22. Hill JA, Agewall S, Baranchuk A, et al. Medical misinformation: vet the message! J Am Heart Assoc. 2019;8(3):e011838. doi:10.1161/JAHA.118.011838
23. Iftikhar R, Abaalkhail B. Health-seeking influence reflected by online health-related messages received on social media: cross-sectional survey. J Med Internet Res. 2017;19(11):e5989. doi:10.2196/jmir.5989
24. Lima ICV, Galvão MTG, Pedrosa SC, Cunha GH, Costa AKB. Use of the Whatsapp application in health follow-up of people with HIV: a thematic analysis. Esc Anna Nery. 2018;22. doi:10.1590/2177-9465-ean-2017-0429
25. O’Reilly M, Dogra N, Hughes J, Reilly P, George R, Whiteman N. Potential of social media in promoting mental health in adolescents. Health Promot Int. 2019;34(5):981–991. doi:10.1093/heapro/day056
26. Latha K, Meena KS, Pravitha MR, Dasgupta M, Chaturvedi SK. Effective use of social media platforms for promotion of mental health awareness. J Educ Health Promot. 2020;9:9. doi:10.4103/jehp.jehp_529_19
27. Vosoughi S, Roy D, Aral S. The spread of true and false news online. Science. 2018;359(6380):1146–1151. doi:10.1126/science.aap9559
28. Al-Faris EA. The selection of appropriate health education topics for publication in the press. Scand J Prim Health Care. 1993;11(3):163–168. doi:10.3109/02813439308994824
29. Saling LL, Mallal D, Scholer F, Skelton R, Spina D. No one is immune to misinformation: an investigation of misinformation sharing by subscribers to a fact-checking newsletter. PLoS One. 2021;16(8):e0255702. doi:10.1371/journal.pone.0255702
30. Kington RS, Arnesen S, Chou W-YS, Curry SJ, Lazer D, Villarruel AM. Identifying credible sources of health information in social media: principles and attributes. NAM Perspect. 2021;2021. doi:10.31478/202107a
31. Gary JL. Social media: how to use it effectively. J Orthop Trauma. 2015;29:S5–S8. doi:10.1097/BOT.0000000000000430
32. Alleje ML, Austria BC, Shrestha PA. Social media etiquette in medicine. Br J Hosp Med. 2019;80(9):130–132. doi:10.12968/hmed.2019.80.9.C130
33. Kornafeld A, Gonzalez-Estrada A, Dimov V. ‘Googling’anaphylaxis. Curr Opin Allergy Clin Immunol. 2019;19(5):432–438. doi:10.1097/ACI.0000000000000575
34. Sylvia Chou W-Y, Gaysynsky A. A prologue to the special issue: health misinformation on social media. Am J Public Health. 2020;110(S3):S270–S272. doi:10.2105/AJPH.2020.305943
35. Stellefson M, Paige SR, Chaney BH, Chaney JD. Evolving role of social media in health promotion: updated responsibilities for health education specialists. Int J Environ Res Public Health. 2020;17(4):1153. doi:10.3390/ijerph17041153
36. John Z. How to fight an infodemic. Lancet. 2020;395(10225):676. doi:10.1016/S0140-6736(20)30461-X
37. Pennycook G, Rand DG. Fighting misinformation on social media using crowdsourced judgments of news source quality. Proc Natl Acad Sci. 2019;116(7):2521–2526. doi:10.1073/pnas.1806781116
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
