Back to Journals » Clinical Ophthalmology » Volume 15
Assessing the Clinical Utility of Point of Care HbA1c in the Ophthalmology Outpatient Setting
Authors Mamtora S , Maghsoudlou P , Hasan H , Zhang W, El-Ashry M
Received 22 October 2020
Accepted for publication 30 November 2020
Published 7 January 2021 Volume 2021:15 Pages 41—47
DOI https://doi.org/10.2147/OPTH.S287531
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Scott Fraser
Video abstract presented by Sunil Mamtora.
Views: 233
Sunil Mamtora, 1 Panayiotis Maghsoudlou, 1, 2 Hani Hasan, 1 Wenrui Zhang, 3 Mohamed El-Ashry 1
1Department of Ophthalmology, Great Western Hospital, Swindon SN3 6BB, UK; 2Department of Developmental Biology, University College London, London WC1E 6BT, UK; 3Department of Ophthalmology, Queen Elizabeth University Hospital, Glasgow G51 4TF, UK
Correspondence: Panayiotis Maghsoudlou
University College London, London, UK
Tel +44 020 7242 9789
Fax +44 020 7905 2000
Email [email protected]
Background/Aims: Effective management of diabetic retinopathy requires multidisciplinary input. We aimed to evaluate the impact of point of care (POC) HbA1c testing as a tool to identify patients most in need of specialist diabetologist input and assess the accuracy and determinants of patients’ insight into their glycaemic and blood pressure control.
Methods: Forty-nine patients with diabetic retinopathy were recruited from the eye clinic at Great Western Hospital. Patients completed a questionnaire and POC HbA1c and blood pressure values were measured. Statistical analysis was completed with SPSS v23.
Results: Mean age was 64.4 years, median interval since the last formal HbA1c reading was 10.2 months and the mean POC HbA1c was 64.1 mmol/mol. HbA1c significantly correlated with the degree of retinopathy. Of the patients, 81.6% had POC readings above the levels recommended by the National Institute for Health and Care Excellence, with only 16.3% having insight into this. Insight to HbA1c levels was predicted by age but not by duration of disease. Fourteen patients (33.3%) identified with high HbA1c readings were referred to secondary diabetic services and 88.8% of patients felt that the test was useful and likely to improve their diabetic control.
Conclusion: The majority of patients had poor insight into their diabetes control, with sub-optimal treatment and follow-up. Poor insight is high in younger patients, suggesting that POC HbA1c testing is particularly important in educating younger patients who may be Type 1 diabetics with more severe disease. POC HbA1c represents a cost-effective, reproducible and clinically significant tool for the management of diabetes in an outpatient ophthalmology setting, allowing the rapid recognition of high-risk patients and appropriate referral to secondary diabetic services.
Keywords: diabetic retinopathy, glycemic control, point of care testing, HbA1c
Introduction
Diabetic eye disease remains one of the most common causes of visual impairment among the working adult population in the UK, with subsequent financial, economic, and health burden.1 Despite increasingly effective treatments including retinal laser, vitreoretinal surgery, and intravitreal treatments2 the prevalence and incidence of the disease continues to rise.3 Diabetes is a complex chronic disease to successfully manage; with reliance placed on the patients’ ability to perform regular glucose self-monitoring, administration of poly-pharmaceutical regimes, and making healthy lifestyle choices and regular attendance for clinical follow-up. Research shows chronic disease treatment non-adherence is as high as 50%.4 Diabetic patients are particularly predisposed to poor treatment adherence, with reported adherence rates of 53–67% for medications, 65% for diet, and 19% for exercise.4,5
Regular glycemic self-monitoring is the mainstay of good diabetic management, providing valuable information to guide medical treatment and prevent acute and chronic complications. Nonetheless this remains one aspect that patients are notably neglectful of. A study showed that amongst Type 2 diabetics, 24% of insulin dependent, 65% of oral anti-diabetic medicated, and 80% of lifestyle managed patients administered self-monitoring of glucose less than once a month.6
HbA1c measurement provides an approximate average of glycemic control in the preceding 3 months. Frequent HbA1c testing, which reflects long-term glycemic control, also has prognostic predictors of diabetic outcomes. A UK multicenter meta-analysis study showed a direct correlation between deteriorating diabetic control and reduced frequency of HbA1c testing.7 In the same study, frequent HbA1c testing led to reductions in HbA1c levels, particularly in those with poor initial HbA1c recordings. Conversely, there was an increase in HbA1c levels with less frequent monitoring. They concluded that the optimal frequency of HbA1c monitoring was every 3 months, which is in keeping with current National Institute for Health and Care Excellence (NICE) guidelines.8
Ophthalmologists are faced with significant challenges when treating patients with diabetic eye disease. Poor medical history combined with inevitable delays in obtaining HbA1c lab results ultimately limits specialist input.
Point of care (POC) HbA1c testing using finger prick blood results could be a valuable screening tool in optimizing diabetic management and improving visual outcomes. POC HbA1c provides instant test feedback with the potential to streamline patient education and intervention. It also represents a cost-effective method of measuring HbA1c in the eye clinic, where it can be used as a triaging parameter to determine which patients would benefit most from referral onto diabetic specialists for intensification of management.
In the UK, the majority of diabetic patients have their diabetes managed by their primary care physician. The ability to offer outpatient appointments with diabetes specialists is limited due to clinic capacity. In this study we therefore aimed to evaluate the viability and clinical impact of POC HbA1c testing as a tool to improve management of diabetes in the NHS within an integrated healthcare setting. We also wanted to assess the accuracy and determinants of patients’ insight into their glycemic and blood pressure control.
Subjects and Methods
This study was completed in accordance with the ethical standards of the Helsinki Declaration of 1975 (as revised in 1983) and was approved by a local research and ethics committee at Great Western Hospital (GWH).
Recruitment
Consecutive patients were prospectively recruited from outpatient diabetic retinopathy clinics at GWH in the period from November 2018 to December 2018. Inclusion criteria consisted of all patients over the age of 18 years, with either Type 1 or Type 2 diabetes, presenting with at least one eye actively affected by diabetic retinopathy with reduced visual acuity using the NHS Diabetic Eye Screening Program grading criteria during the sampling period.10 There were no applicable exclusion criteria; patients were asked if they wished to participate in the study, confirmed with written consent, and then consecutively recruited in the above period. None of the eligible patients asked to take part in the study declined.
Data Collection
Patients were asked prior to their appointment to complete an internally validated questionnaire formulated with multidisciplinary team input from the eye department following a pilot study. Questions detailing personal perception of their glycemic and blood pressure control, type of diabetes, duration of disease, type of clinical management (ie, primary, secondary care), current medications for diabetes and hypertension were recorded. The following NICE objective HbA1c values were suggested as indicative ranges: Good control: <48 mmol/mol, average control: ≥48–>58 mmol/mol, poor control: ≥58->75 mmol/mol, very poor control: ≥75 mmol/mol.8 Furthermore, patients were asked their opinion toward the usefulness of POC HbA1c testing and the likelihood that the results would improve their diabetes management and control.
All patients had their POC HbA1c sample tested using the Quo-Test A1c system (EKF Diagnostics, Cardiff, UK), which operates with a finger prick blood test. Blood pressure was measured using the Dinamap V100 monitor (GE Healthcare, IL, USA). Two separate blood pressure measurements were taken 5 minutes apart on the same arm, with the second reading recorded and used in the analysis as per British Hypertensive Society guidelines.11
Following collection of questionnaire data, patient case notes and previous blood results were reviewed. Information regarding their previous retinopathy treatment, grade of retinopathy using the NHS DES classification of the worse eye,10 and the date and value of the last serum HbA1c taken either in primary or secondary care were recorded for all patients.
Data Analysis
All analyses were carried out using GraphPad Prism® 6 (GraphPad Software, CA, USA) and SPSS ® Statistics 23 (IBM, NY, USA). Shapiro–Wilk test was performed to assess normality of data. Continuous variables are expressed as mean±SD for normally distributed data and median (range) for those without a normal distribution, and compared using the independent samples t-test and Mann–Whitney U-test, respectively. Correlation was determined using Spearman analysis. Multiple linear regression analysis for the accurate prediction of HbA1c levels was completed, including age, sex, type of diabetes, length of diabetes, and degree of retinopathy. All statistical tests were two-sided and P<0.05 was considered as statistically significant.
Results
Forty-nine patients fulfilled the inclusion criteria and were recruited in the study. Table 1 outlines the demographic data and measurements taken at the point of care in the outpatient clinic during the recruitment period. Mean age was 64.4±14.0 years and was significantly lower (P<0.01) in Type 1 diabetics (48.7±10.8) compared to Type 2 diabetics (67.0±12.8, t-test). The patient cohort comprised of 15 female (30.6%) and 34 male (69.4%) patients, with no significant difference between age, onset of disease, and HbA1c according to gender (Mann–Whitney U-test). Seven patients (14.3%) were Type 1 diabetics and 42 (85.7%) were Type 2 diabetics. The duration of diabetes was significantly higher (P<0.01, Mann–Whitney U-test) in the Type 1 group (36 years [15–42]) compared to the Type 2 group (15 years [1–40]) (Table 2).
 |
Table 1 Baseline Demographics |
 |
Table 2 Ophthalmic Findings and Treatment |
The median interval since the last HbA1c reading was 209 days (25–299) and 129 days (25–516) in the Type 1 and Type 2 cohorts, respectively, with no significant difference (Table 2). The mean POC HbA1c was not significantly different between the two groups (63.5 and 64.2 mmol/mol, respectively, Mann–Whitney U-test). Fourteen patients (33.3%) who had POC HbA1c readings >64 mmol/mol were referred onto secondary diabetic services as per national guidelines. HbA1c significantly correlated with the degree of retinopathy (r=0.3). All Type 1 diabetics had significant diabetic retinopathy (R3M0 71.4%, R3M1 28.6%) and were treated with insulin therapy and routinely followed up in secondary care. Most Type 1 diabetics had grade 1 diabetic retinopathy (R1; 66.6%), with (R1M1; 33.3%) or without (R1M0; 33.3%) maculopathy. Type 2 diabetics were mostly on tablet therapy (81%) or combined tablet and insulin therapy (19%). Thirty-five (83.3%) were followed up in primary care by their general practitioner, and seven (16.7%) were reviewed in secondary care.
Self-Perception of Glycemic Control Analysis
Prior to POC HbA1c measurements, patients were asked to self-rate their perception of their glycemic control on a rating scale of: good, average, poor, and very poor. Table 3 illustrates the differences between patients’ perception of their glycemic control when compared to actual POC readings taken for both Type 1 and Type 2 diabetics, while also highlighting the percentage of patients who had good insight into their diabetic control. While most Type 1 diabetics rated their glycemic control as good (71.4%), only one patient had an HbA1c reading below the recommended 48 mmol/mol and most (42.9%) had very poor control. The majority of Type 2 diabetics rated their glycemic control as average (66.6%), while approximately a third (35.7%) had poor control. No patients rated their glycemic control as very poor, while in fact this represented 26.5% of the cohort. Spearman correlation showed a non-significant correlation of r=−0.23 between HbA1c level and perspective of glycemic control (Figure 1).
 |
Table 3 Perception of Glycemic Control |
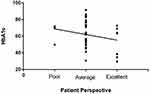 |
Figure 1 HbA1c levels according to patient perspective. |
Overall, 42.3% (3/7) and 26.2% (11/42) of Type 1 and Type 2 diabetics were able to correctly self-rate their glycemic control (Table 3). Multiple linear regression was carried out to investigate the relationship between accuracy of predicted HbA1c and variables including age, type of DM, gender, years of DM diagnosis, and HbA1c. There was a significant relationship between accuracy of predicted HbA1c and higher levels of HbA1c (P<0.001). The R2 value was 0.792, indicating that 79.2% of the variation in HbA1c prediction accuracy can be explained by the model containing HbA1c levels and age. This suggests that, while older patients with a high HbA1c have the most insight into their HbA1c levels, younger patients do not.
In terms of usefulness of POC HbA1c testing, 100% of the Type 1 diabetics felt that performing the test was useful or very useful, with 100% feeling that having knowledge from instant point of care HbA1c results were likely or very likely to improve their diabetic control. Of the Type 2 diabetics surveyed, 85.7% (36/42) felt that performing POC HbA1c testing was useful or very useful and felt that it would likely or most likely improve their glycemic control.
Blood Pressure Analysis
The blood pressure of Type 1 and Type 2 diabetics was 152.4±19.3/75.1±7.1 mmHg and 150.7±16.9/76.6±11.3 mmHg, respectively, with no significant difference (t-test). All Type 1 diabetics were already on antihypertensive medications; monotherapy (n=3) and dual therapy (n=4). Within the Type 2 DM cohort five patients were on no anti-hypertensive medications, 17 received monotherapy, 18 dual therapy, and two were on triple therapy. While the majority of Type 1 (4/7, 57.1%) and Type 2 (30/42, 71.4%) diabetics had poor BP control, only three (6.1%) rated their BP control as poor and overall only 18.4% (9/49) were able to correctly self-rate their blood pressure control (Table 4).
 |
Table 4 Perception of Blood Pressure Control |
Discussion
The main objective of the study was to establish the clinical value of POC HbA1c blood tests as a screening tool to identify diabetic patients with sight threatening diabetic retinopathy (SDTR) who would benefit from secondary intervention to optimize their diabetic control. Effective ophthalmological intervention is ultimately limited without medical and holistic optimization of the underlying diabetes.2 Poor glycemic control combined with cardiovascular risk factors such as blood pressure, abnormal lipid profile, high BMI, and prolonged duration of underlying disease represent risk factors for progression of diabetic retinopathy.15–20
The average duration of diabetic diagnosis for the total sample population was 18 years, the mean point of care HbA1c reading was 64.1 mmol/mol and average time interval since the last formal HbA1c result was 10.2 months. Just over half of the patients (57.1%, 28/49) had a previous HbA1c result recorded within the last 6 months as recommended by the current NICE guidelines.8 Fourteen patients were managed in hospitals with 64.3% (9/14) of patients having had a recent HbA1c test within 6 months compared to 54.3% (19/35) of patients managed in primary care.
Our study found that, collectively, the majority of both Type 1 and Type 2 diabetic patients presenting to the clinic with diabetic retinopathy had poor insight into their glycemic and blood pressure control. High HbA1c levels were associated with a greater degree of retinopathy. Studies investigating patient vs clinical perceptions of diabetes often show a disparity in patient–clinician mismatch related to glycemic control, medical terms, and treatment compliance,12 and, as a consequence, have led to poorer outcomes for patients.13 Of the patients in our study, 81.6% had POC readings above NICE recommended good HbA1c levels of 48 mmol/mol,with only 16.3% able to have good insight into this. Accuracy of HbA1c insight is predicted by age and not by type of diabetes or duration of disease, suggesting that POC HbA1c testing is particularly important in educating younger patients who may be Type 1 diabetics with more severe disease.
Patients felt POC HbA1c testing was useful with regards to diabetes care and would likely improve their glycemic control. Clinically, based on the results from the POC test, 14 patients required referral onto secondary diabetic services. The cut-off parameters for referral were all patients with POC HbA1c readings >64 mmol/mol, which is strongly associated with diabetic retinopathy and reflected in the Trust guidelines for referral. This cut-off was made following local agreement between Ophthalmologists and Diabetologists in order to balance specialist diabetes clinic appointment availability and clinical necessity.
Ideally, effective ophthalmological management of diabetic retinopathy requires multidisciplinary input from diabetic specialists to minimize visual and systemic morbidity and mortality. Subsequently, our study aimed to assess the merits and clinical usefulness of POC HbA1c finger prick blood test as a screening tool to quickly identify the patients who would mostly benefit from intensified secondary intervention as well as an efficient screening tool that does not impact on current resources such as physicians time, laboratory and appointment resources.
POC HbA1c testing is a relatively new but promising technology. A previous US-based randomized controlled trial concluded that measurement of POC HbA1c in an office-based ophthalmic setting did not lead to improved diabetic control.9 Although there are limited assessments of its use in a clinical setting, small trials show that results from POC HbA1c are comparable in accuracy to laboratory HbA1c results with correlation of r=0.758 with POC results within 6–8% of lab recorded values.14 A larger 4-arm clinical trial studying active vs usual algorithmic titration of basal insulin and POC vs laboratory measurements of HbA1c on glycemic control of Type 2 diabetic patients showed that POC HbA1c testing was associated with an increased proportion of patients able to achieve HbA1c readings <53 mmol/mol than those who had been lab monitored (41% for POC vs 36% for laboratory).15
The study was limited due to a relatively small sample size. Furthermore, our study lacks longitudinal data for the 14 patients who were referred from the hospital eye service for specialist diabetes intervention. This data was not included as an extended follow-up interval would be required to appreciate the impact of intensification patients’ diabetic disease including diabetic retinopathy.
POC HbA1c represents a cost-effective, reproducible, and clinically significant tool for the management of diabetes in an outpatient ophthalmology setting, allowing the rapid recognition of high-risk patients and appropriate referral to secondary diabetic services. Our study demonstrated that poor insight of HbA1c levels was high in younger patients, suggesting that POC HbA1c testing is particularly important in educating younger patients who may be Type 1 diabetics with more severe disease. Patient feedback confirms the usefulness in clinical practice and POC HbA1c can improve patient education, shared decision-making, and clinical outcomes and could be incorporated in regular clinical practice. POC HbA1c is particularly important in an integrated healthcare system, such as the National Health Service, to determine the appropriate patients to refer to diabetes specialists and reduce potential systemic complications.
Acknowledgments
The work was completed at Great Western Hospital. We would like to thank Miss. Chanelle Smith, Medical Student, Bristol University, UK, for her assistance with data collection during the study period and Mr. Nimish Shah, Consultant Ophthalmologist, Great Western Hospital, Marlborough Road, Swindon, SN3 6BB, UK, for his guidance during the study period, assistance with data collection, and for providing the opportunity for close liaison with our local diabetologists.
Funding
The authors have no funding to declare.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Liew G, Michaelides M, Bunce C. A comparison of the causes of blindness certifications in England and Wales in working age adults (16-64 years), 1999-2000 with 2009-2010. BMJ Open. 2014;4:e004015. doi:10.1136/bmjopen-2013-004015
2. Frank RN. Systemic therapies for diabetic retinopathy: the accord eye study. Ophthalmology. 2014;121(12):2295–2296. doi:10.1016/j.ophtha.2014.08.019
3. Yau JWY, Rogers SL, Kawasaki R, et al. Global prevalence and major risk factors of diabetic retinopathy. Diabetes Care. 2012;35:556–564. doi:10.2337/dc11-1909
4. Delamater AM. Improving patient adherence. Clin Diabetes. 2006;24:71–77. doi:10.2337/diaclin.24.2.71
5. Anderson RM, Fitzgerald JT, Oh MS. The relationship between diabetes-related attitudes and patients’ self- reported adherence. Diabetes Educ. 1993;19:287–292. doi:10.1177/014572179301900407
6. Harris MI. Frequency of blood glucose monitoring in relation to glycemic control in patients with type 2 diabetes. Diabetes Care. 2001;24:979–982. doi:10.2337/diacare.24.6.979
7. Driskell OJ, Holland D, Waldron JL, et al. Reduced testing frequency for glycated hemoglobin, HbA1c, is associated with deteriorating diabetes control. Diabetes Care. 2014;37:2731–2737. doi:10.2337/dc14-0297
8. National Institute for Health and Care Excellence. Overview | type 2 diabetes in adults: management | guidance | NICE. Type 2 diabetes adults Manag. 2019. Available from: https://www.nice.org.uk/guidance/ng28.
9. Aiello LP, Ayala AR, Antoszyk AN, et al. Assessing the effect of personalized diabetes risk assessments during ophthalmologic visits on glycemic control: a randomized clinical trial. JAMA Ophthalmol. 2015;133:888–896. doi:10.1001/jamaophthalmol.2015.1312
10. Public Health England. NHS Diabetic Eye Screening Programme. NHS Diabet. Eye Screen. Program. 2016. Available from: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/505587/DES_07_GP_information_sheet_March_2016.pdf.
11. Ramsay LE, Williams B, Johnston GD, et al. Guidelines for management of hypertension: report of the third working party of the British Hypertension Society. J Hum Hypertens. 1999;13:569–592. doi:10.1038/sj.jhh.1000917
12. Hunt LM, Arar NH, Larme AC. Contrasting patient and practitioner perspectives in Type 2 diabetes management. West J Nurs Res. 1998;20:656–682. doi:10.1177/019394599802000602
13. Loewe R, Freeman J. Interpreting diabetes mellitus: differences between patient and provider models of disease and their implications for clinical practice. Cult Med Psychiatry. 2000;24:379–401. doi:10.1023/A:1005611207687.
14. Sicard DA, Taylor JR. Comparison of point-of-care HbA 1c test versus standardized laboratory testing. Ann Pharmacother. 2005;39:1024–8. doi:10.1345/aph.1E504.
15. Kennedy L, Herman WH, Strange P, et al. Impact of active versus usual algorithmic titration of basal insulin and point-of-care versus laboratory measurement of HbA1c on glycemic control in patients with type 2 diabetes: the Glycemic Optimization with Algorithms and Labs at Point of Care (GOAL A1C) trial. Diabetes Care. 2006;29:1–8. doi:10.2337/diacare.29.01.06.dc05-1058
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
