Back to Journals » Cancer Management and Research » Volume 14
Assessing Diagnostic Value of Combining Ultrasound and MRI in Extrathyroidal Extension of Papillary Thyroid Carcinoma
Authors Hu S , Zhang H, Zhong Y, Agyekum EA , Sun Z , Ge Y, Li J, Dou W, He J, Xiang H, Wang Y, Qian X, Wang X
Received 22 November 2021
Accepted for publication 8 March 2022
Published 29 March 2022 Volume 2022:14 Pages 1285—1292
DOI https://doi.org/10.2147/CMAR.S350032
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Chien-Feng Li
Shudong Hu,1,2,* Heng Zhang,1,2,* Yanqi Zhong,3,* Enock Adjei Agyekum,2,* Zongqiong Sun,1 Yuxi Ge,1 Jie Li,4 Weiqiang Dou,5 Junlin He,6 Hong Xiang,7 Yuandong Wang,8 Xiaoqin Qian,2 Xian Wang2
1Department of Radiology, Affiliated Hospital, Jiangnan University, Wuxi, People’s Republic of China; 2Department of Ultrasound, Affiliated People’s Hospital of Jiangsu University, Zhenjiang, People’s Republic of China; 3School of Medicine, Jiangnan University, Wuxi, People’s Republic of China; 4Department of Interventional Radiology, Affiliated Hospital, Jiangnan University, Wuxi, People’s Republic of China; 5GE Healthcare, MR Research China, Beijing, People’s Republic of China; 6Department of Radiology, Tinglin Hospital of Jinshan District, Shanghai, People’s Republic of China; 7Department of Pediatric, Affiliated Hospital of Jiangsu University, Zhenjiang, People’s Republic of China; 8Department of Radiotherapy, Affiliated People’s Hospital of Jiangsu University, Zhenjiang, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Xian Wang; Xiaoqin Qian, Tel +86 13952808812 ; +86 13813186750, Email [email protected]; [email protected]
Purpose: To explore the separate diagnostic value of preoperative ultrasound (US), magnetic resonance imaging (MRI), and the combination of US and MRI in extrathyroidal extension (ETE) of papillary thyroid carcinoma (PTC).
Materials and Methods: This retrospective study was approved by the Affiliated People’s Hospital of Jiangsu University review board. A total of 158 PTC patients with ETE received preoperative US and MRI examination and underwent surgery between May 2014 and December 2018 in Affiliated People’s Hospital of Jiangsu University. For each case, the US and MRI features of ETE were retrospectively and independently investigated by two radiologists. The clinical assessment for each case was implemented, respectively, using US imaging only, MRI only, and a combination of both modalities at three different time points with one-month intervals.
Results: The diagnostic accuracies of US, MRI, and the combined set for T3 (minimal ETE) were 91.7% (88/96), 74.0% (71/96), and 97.9% (94/96), respectively, indicating a significantly different performance (P < 0.001). The diagnostic accuracies for T4 (extensive ETE) were 62.9% (39/62), 87.1% (54/62), and 93.5% (58/62), respectively. The difference between the three methods for T4 was statistically significant (P = 0.000). The diagnostic accuracies for overall ETE were 80.4% (127/158), 79.1% (125/158), and 96.2% (152/158), respectively. The difference between the three methods for ETE was statistically significant (P = 0.001).
Conclusion: This study suggests that ETE can be predicted most accurately by the combination of preoperative US and MRI.
Keywords: thyroid cancer, ultrasonography, magnetic resonance imaging, neoplasm staging
Introduction
Papillary thyroid cancer (PTC) is the most common type of well-differentiated thyroid cancer.1–5 The malignant degree of PTC is low, which is associated with low mortality and morbidity.1–4,6–13 However, some PTCs (aggressive PTC variants such as tall cell, columnar, hobnail, cribriform, T3 or T4 tumors, tumors with nodal metastases, N1a or N1b tumors with distant metastases, tumors with extensive ETE, and so on) exhibit aggressive behavior and recurrence.6–9,11–13 Extrathyroidal extension (ETE) is recognized as a significant factor influencing PTC prognosis and recurrence.4,6–8,10,11,13 ETE is a tumor that grows outside of the thyroid gland and enters nearby or surrounding tissues. According to the American Joint Committee on Cancer (AJCC) (Edition VIII) TNM staging of thyroid cancer, ETE is classified as (I) T3: minimal ETE (extension to sternothyroid muscle or perithyroid soft tissues); and (II) T4: extensive ETE (extension to subcutaneous soft tissue, larynx, trachea, esophagus, recurrent laryngeal nerve (RLN), or the prevertebral fascia.14 ETE, along with other factors such as age, tumor size, and cervical lymph node metastasis, has been established as an important prognostic factor. Extensive ETE has significant clinical utility as a prognostic marker, potentially outweighing other prognostic factors.6 Patients who had extensive ETE had a 13-fold higher risk of recurrence.6 The American Thyroid Association’s practice guidelines recommend total thyroidectomy for patients with ETE and postoperative radioactive iodine ablation for patients with high-risk PTCs.5,9,11,12,14 As a result, preoperative detection of ETE is critical not only for adequate nodal staging but also for surgical planning.
Currently, ultrasound (US) is a common method for the initial diagnostic evaluation of ETE of PTCs in clinics.15–21 Previous research on the diagnostic performance of preoperative US for the determination of ETE of PTCs reported numerous benefits, such as high-resolution imaging capability and ease of access.15–21 However, the US has several limitations. The most important is operator reliance. Meanwhile, MRI is increasingly being used to image the thyroid gland.19,22–26 Multiplanar section MRI of lesions can be used to visualize the thyroid anatomy in stereoscopic mode. MRI has been proposed as a complementary method for assessing large tumors or extensive ETE, particularly the invasion of adjacent structures (trachea, esophagus, and great vessels).19,22–26 There have been few studies to date on the value of US, MRI, or a combination of the two in assessing ETE of PTC. As a result, the primary goal of this study was to assess the feasibility and clinical utility of high-resolution US, MRI, and a combination of both in predicting ETE in patients with PTCs.
Materials and Methods
Study Population
The study was conducted in accordance with the Declaration of Helsinki and the study was approved by the Ethics Committee of Jiangsu University Affiliated People’s Hospital. Informed consent was obtained from all subjects involved in the study. A search of the hospital’s database yielded 158 patients with surgically and pathologically confirmed PTCs with ETE who underwent preoperative thyroid US and MRI at our institute between May 2014 and December 2018. This study included 158 patients (59 males and 99 females) with a mean age of 48.9 years (range, 24–72 years). The male to female ratio was approximately 1:1.68, with 86 (54.4%) over 45 years old and 72 (45.6%) under 45 years old. Among all patients, 95 (60.1%) were diagnosed with PTC during a routine health examination, 34 (21.5%) had a neck mass discovered by themselves, four (2.5%) had dysphagia, eight (5.1%) had hoarseness, and the remaining 17 (10.8%) had a history of thyroid disease. All patients had a thyroid ultrasound and an MRI within two weeks before having a thyroidectomy.
Instruments and Methods
US Examination
All patients had routine preoperative US performed by well-trained technicians using an iU22 (Philips Healthcare, Eindhoven, the Netherlands) ultrasound system with a 5–12 MHz linear array transducer. The instrument was programmed to run a specific “Thyroid” program. During the examination, each patient was placed in a supine position with a pillow removed and the head lowered and moved slightly backward to expose the neck as much as possible. First, the thyroid was examined using two-dimensional ultrasound. The probe was placed beneath the thyroid cartilage. The location, diameter, and number of nodules, as well as their sonographic manifestations, were determined using both cross-sectional and longitudinal examinations. Color Doppler flow imaging (CDFI) was used to observe blood flow distribution in and around the nodules after observing superficial and deep muscles, trachea, esophagus, and great vessels surrounding the parathyroid gland.
MRI Examination
All examinations were carried out on two 1.5 Tesla MR scanners (GE Signa HD 1.5 TMR scanner; GE Healthcare Systems, Milwaukee, WI, USA, and UIH uMR560 1.5T MR scanner, United Imaging Healthcare, Shanghai, China) equipped with an eight-channel high-resolution receiver synergy-head/neck phased-array coil. T1WI, T2WI, DWI, and contrast-enhanced MRI were all used in all MRI protocols. Conventional MRI: axial T1WI spin-echo (TR/TE=520/14ms), T2WI fast spin-echo (TR/TE=3500/95 ms) with and without fat suppression, and coronal T2WI (TR/TE = 3500/95). DWI was acquired in three orthogonal directions using STIR fat-suppressed single-shot echo-planar imaging spin-echo sequences at two different b values (0 and 500 s/mm2). All patients had contrast-enhanced T1WI (TR/TE=520/14ms) with or without fat suppression immediately following intravenous injection of 0.1mmol/kg Gd-DTPA (Magnevist, Schering AG, Germany). Section thickness 3 mm, with a 1-mm intersection gap, FOV = 40×28 cm, matrix = 256×256, number of excitations (NEX) = 4. The entire exam was completed in 30 minutes.
Image Analysis
Preoperative imaging with US and MRI was performed on all patients. Two experienced radiologists, each with 15 and 20 years of experience in head and neck MRI, reviewed the images and reached an agreement. The review of US and MRI images was done independently over a two-week period. All US and MRI images were reviewed retrospectively and independently by two radiologists for minimal ETE and invasion into the surrounding tissues of the trachea, esophagus, common carotid artery (CCA), internal jugular vein (IJV), and RLN. In patients with multiple thyroid lesions, both reviewers were blinded to the surgical and pathologic findings but were given information about the location and size of the index malignancy. Both reviewers worked independently and were unaware of the patient’s clinical history, previous radiological findings, and final diagnosis. The ETE of the PTCs was classified using AJCC guidelines (Edition VIII). Minimal ETE was defined as more than 25% of the lesion’s perimeter in contact with the thyroid capsule or loss of the echogenic capsule line at the lesion’s contact site. Extensive ETE was defined as a tumor of any size that extended beyond the thyroid capsule and invaded the subcutaneous soft tissues, larynx, trachea, esophagus, RLN, carotid artery, or mediastinal vessels.
Statistical Analysis
All statistical analyses were carried out using the SPSS 20.0 statistical software (SPSS Inc., Chicago, IL, USA). The mean standard deviation was used to express continuous data. The findings of the US and MRI were compared to the pathological results obtained after surgery. There was an agreement between the pathological findings and those of MRI-identified ETE and US. The differences in patient age and thyroid nodule diameters were analyzed using an unpaired Student’s t-test.
Results
Pathology confirmed ETE in all 158 PTC patients. There were 74 patients with right-sided lesions, 61 with left-side lesions, and 23 with isthmus lesions. Lesions ranged in size from 0.8 cm to 4.6 cm, with a mean of 2.54 ±0.88 cm. There were 75 patients who had capsule extension, 24 who had extension into sternothyroid muscle, 27 who had extension into the trachea, 20 who had extension into the esophagus, five who had extension into the great vessels, and ten who had extension invaded the RLN. The pathological findings after surgery revealed that 96 patients had T3 carcinomas and 62 had T4 carcinomas.
Diagnosis of ETE T3 Staging of PTC
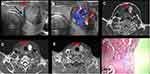
US correctly diagnosed 88 cases as T3 (Figure 1A and B), with an accuracy rate of 91.7% (88/96) and a misdiagnosis rate of 8.3% (8/96); among them, five cases were diagnosed severely (Figure 2) and three cases were diagnosed superficially. MRI correctly classified 71 cases as T3 (Figure 1C–E), with an accuracy rate of 74.0% (71/96) and a misdiagnosis rate of 26.0% (25/96); 17 cases were classified severely and eight cases were classified superficially. The combination of US and MRI correctly diagnosed 94 cases of T3, with an accuracy of 97.9% (94/96) and a 2.1% (2/96) misdiagnosis rate. The differences in diagnostic accuracy between the three methods were statistically significant (P<0.001, Table 1).
 |
Table 1 Diagnostic Accuracy: Comparison of US, MRI and Combined Examination of ETE |
Diagnosis of ETE T4 Staging of PTC
A total of 39 cases were correctly diagnosed using US as T4, with an accuracy of 62.9% (39/62) and a misdiagnosis rate of 37.1% (23/62); 8 cases were diagnosed severely and 15 cases were diagnosed superficially (Figure 3). MRI was used to correctly diagnose 54 cases as T4, with an accuracy of 87.1% (54/62) and a misdiagnosis rate of 12.9% (8/62); four cases were diagnosed severely, while four cases were diagnosed superficially. A total of 58 cases were correctly diagnosed as T4 using a combination of US and MRI, with a 93.5% (58/62) accuracy rate and a 6.5% (4/62) misdiagnosis rate. The differences in diagnostic accuracy between the three groups were statistically significant (P=0.000, Table 1).
Diagnosis of Overall ETE of PTC
In total, 127 cases were correctly diagnosed using US as the overall ETE, with an accuracy rate of 80.4% (127/158) and a misdiagnosis rate of 19.6% (31/158); 125 cases were correctly diagnosed using MRI as the overall ETE, with an accuracy rate of 78.1% (125/158) and a misdiagnosis rate of 20.9% (33/158). The combined use of US and MRI correctly diagnosed 152 cases as overall ETE, with an accuracy of 96.2% (152/158) and a misdiagnosis rate of 3.6% (6/158). The diagnostic accuracy differences between the three groups were statistically significant (P=0.001, Table 1).
Discussion
In this study, we evaluated the diagnostic performance of preoperative high-resolution US, MRI, and a combined set of both for the prediction of ETE in patients with PTCs. According to the results, the combination of preoperative US and MRI performed the best in predicting ETE in PTC patients.
The presence of ETE is regarded as significant and has been included as a staging variable in almost all prognostic scoring systems. The reported incidence of ETE in the literature ranges from 5% to 34%.1,2,7,9,13 Currently, methods of imaging ETE of PTC include US, CT, MRI, radionuclide imaging, and others. US is the preferred method for ETE due to a number of advantages such as the absence of radiation, the absence of pain, real-time dynamic imaging, and so on. US can provide higher spatial resolution, more clearly display the normal thyroid capsule, and achieve higher accuracy in the diagnosis of micro ETE. Several previous studies demonstrated the relatively good predictability of US findings for minimal ETE.16,18–21 The diagnostic accuracies of the US in this study for minimal ETE and extensive ETE were 91.7% and 62.9%, respectively, which was consistent with previous studies’ findings. However, the inherent characteristics of US limit its application in clinics. It is heavily influenced by the operator’s subjectivity during scanning, such as artificial compression or omission of marginal small lesions, resulting in unclear lesions. Furthermore, because the central region of the upper respiratory tract tissues is occluded by gas interference in the trachea, it is impossible to clearly display the fine structure of those tissues and determine whether the PTC has extended into tracheal mucosa.
MRI is a common imaging technique for diagnosing ETE of PTC. Anatomical imaging with MRI is more intuitive than US and is less affected by the examiner’s subjectivity. It is also easier to precisely locate the tumor prior to surgery and to display tissues that are inaccessible to US, such as the mediastinum and parapharynx. Furthermore, it allows for good soft tissue resolution and can precisely stage lesions and define peripheral invasion prior to surgery. As a result, MRI is more effective than US in assessing extensive ETE. In this study, US only indicated an invasion of the thyroid capsule in four cases of PTC invasion of tracheal mucosa. MRI, on the other hand, has a higher resolution and is unaffected by the presence of skeleton or gas, allowing it to clearly show the boundary of tumors and their relationship with the trachea. It indicated that the PTC had invaded the tracheal mucosa in these cases. With the advancement of new technology, MRI can now assess the extent of PTC invasion of the RLN, as well as display its continuity and abnormal signal intensity around the lesion. MRI is an important imaging technique for predicting PTC invasion of the RLN. However, it has limitations. For example, MRI cannot be used on patients who have metal in their bodies. It is calcification insensitive and prone to artifacts. It has a poor spatial resolution as well. Furthermore, patients with a history of contrast agent allergy cannot have an enhanced MRI examination.
The principles of US and MRI are not the same. They can observe lesions from multiple angles and layers, make a thorough and accurate diagnosis of ETE, and provide a solid foundation for clinical treatment. In this study, the diagnostic accuracy of the US for ETE was 80.4%, with a 19.6% misdiagnosis rate. The diagnostic accuracy of MRI was 79.1%, with a 20.9% misdiagnosis rate. When they were combined, they had a diagnostic accuracy of 96.2% and a misdiagnosis rate of 3.6% indicating that the combined set is significantly better than either modality alone. Because US has good tissue resolution on the thyroid and MRI has good density resolution, their combination improved the diagnostic accuracy of ETE of PTC and reduced the misdiagnosis rate. As a result, the complementary advantages of the two methods are extremely important for improving the detection of ETE in PTC. A combined diagnosis is more than just a combination of US and MRI diagnosis results. In patients with a small mass and clear microcalcification, US examination should be prioritized, whereas MRI examination should be prioritized in patients with a large mass. Patients can be diagnosed using US first, and those with suspicious or unclear diagnoses can be further diagnosed using MRI, followed by a comprehensive analysis based on the two methods.
Limitations of the Study
Our study had several limitations. First, one major limitation of this study was the low prevalence of invasion of the esophagus, trachea, and RLN in the study group. This low prevalence may have influenced the accuracy of experimental results. Second, this was a retrospective study. As a result, selection bias may have existed. Third, this study did not use a combined set of US and MRI data for tumor staging. In conclusion, both methods have distinct advantages and disadvantages. The US can be used as a primary screening method, while the MRI can be used as an additional supplementary examination. In this context, combining US and MRI improves ETE of PTC diagnostic accuracy and provides a more reliable foundation for clinical treatment.
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was financially supported by Jiangsu University Clinical Medical Science and Technology Development (Project No.JLY2021001), Zhenjiang Commission of Science and Technology (Project No. SH2020046, Project No. SH2018050, Project No. SH2018056).
Disclosure
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
1. Nilubol N, Kebebew E. Should small papillary thyroid cancer be observed? A population-based study. Cancer. 2015;121(7):1017–1024. doi:10.1002/cncr.29123
2. Fagin JA, Wells SA. Biologic and clinical perspectives on thyroid cancer. N Engl J Med. 2016;375(11):1054–1067. doi:10.1056/NEJMra1501993
3. Vaccarella S, Franceschi S, Bray F, et al. Worldwide thyroid-cancer epidemic? The increasing impact of overdiagnosis. N Engl J Med. 2016;375(7):614–617. doi:10.1056/NEJMp1604412
4. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA Cancer J Clin. 2019;69(1):7–34. doi:10.3322/caac.21551
5. Lim H, Devesa SS, Sosa JA, et al. Trends in thyroid cancer incidence and mortality in the United States, 1974–2013. JAMA. 2017;317(13):1338–1348. doi:10.1001/jama.2017.2719
6. Kim JW, Roh JL, Gong G, et al. Extent of extrathyroidal extension as a significant predictor of nodal metastasis and extranodal extension in patients with papillary thyroid carcinoma. Ann Surg Oncol. 2017;24(2):460–468. doi:10.1245/s10434-016-5594-4
7. Youngwirth LM, Adam MA, Scheri RP, et al. Extrathyroidal extension is associated with compromised survival in patients with thyroid cancer. Thyroid. 2017;27(5):626–631. doi:10.1089/thy.2016.0132
8. Amit M, Boonsripitayanon M, Goepfert RP, et al. Extrathyroidal extension: does strap muscle invasion alone influence recurrence and survival in patients with differentiated thyroid cancer? Ann Surg Oncol. 2018;25(11):3380–3388. doi:10.1245/s10434-018-6563-x
9. Chu KP, Baker S, Zenke J, et al. Low-activity radioactive iodine therapy for thyroid carcinomas exhibiting nodal metastases and extrathyroidal extension may lead to early disease recurrence. Thyroid. 2018;28(7):902–912. doi:10.1089/thy.2017.0136
10. Liang J, Huang X, Hu H, et al. Predicting malignancy in thyroid nodules: radiomics score versus 2017 American College of Radiology Thyroid Imaging, Reporting and Data System. Thyroid. 2018;28(8):1024–1033. doi:10.1089/thy.2017.0525
11. Abraham E, Roshan D, Tran B, et al. The extent of extrathyroidal extension is a key determinant of prognosis in T4a papillary thyroid cancer. J Surg Oncol. 2019;120(6):1016–1022. doi:10.1002/jso.25683
12. Lee YK, Kim D, Shin DY, et al. The prognosis of papillary thyroid cancer with initial distant metastasis is strongly associated with extensive extrathyroidal extension: a retrospective cohort study. Ann Surg Oncol. 2019;26(7):2200–2209. doi:10.1245/s10434-019-07314-x
13. Song E, Lee YM, Oh HS, et al. A relook at the T stage of differentiated thyroid carcinoma with a focus on gross extrathyroidal extension. Thyroid. 2019;29(2):202–208. doi:10.1089/thy.2018.0300
14. Edge SB, Compton CC. The American Joint Committee on Cancer: the 7th edition of the AJCC cancer staging manual and the future of TNM. Ann Surg Oncol. 2010;17(6):1471–1474. doi:10.1245/s10434-010-0985-4
15. Kim SY, Kwak JY, Kim EK, et al. Association of preoperative US features and recurrence in patients with classic papillary thyroid carcinoma. Radiology. 2015;277(2):574–583. doi:10.1148/radiol.2015142470
16. Yi YS, Kim SS, Kim WJ, et al. Comparison of two- and three-dimensional sonography for the prediction of the extrathyroidal extension of papillary thyroid carcinomas. Korean J Intern Med. 2016;31(2):313–322. doi:10.3904/kjim.2014.363
17. Kuo EJ, Thi WJ, Zheng F, et al. Individualizing surgery in papillary thyroid carcinoma based on a detailed sonographic assessment of extrathyroidal extension. Thyroid. 2017;27(12):1544–1549. doi:10.1089/thy.2017.0457
18. Gweon HM, Son EJ, Youk JH, et al. Preoperative assessment of extrathyroidal extension of papillary thyroid carcinoma: comparison of 2- and 3-dimensional sonography. J Ultrasound Med. 2014;33(5):819–825. doi:10.7863/ultra.33.5.819
19. Kim H, Kim JA, Son EJ, et al. Preoperative prediction of the extrathyroidal extension of papillary thyroid carcinoma with ultrasonography versus MRI: a retrospective cohort study. Int J Surg. 2014;12(5):544–548. doi:10.1016/j.ijsu.2014.03.003
20. Lee CY, Kim SJ, Ko KR, et al. Predictive factors for extrathyroidal extension of papillary thyroid carcinoma based on preoperative sonography. J Ultrasound Med. 2014;33(2):231–238. doi:10.7863/ultra.33.2.231
21. Lee DY, Kwon TK, Sung MW, et al. Prediction of extrathyroidal extension using ultrasonography and computed tomography. Int J Endocrinol. 2014;2014:351058. doi:10.1155/2014/351058
22. Erdem G, Erdem T, Muammer H, et al. Diffusion-weighted images differentiate benign from malignant thyroid nodules. J Magn Reson Imaging. 2010;31(1):94–100. doi:10.1002/jmri.22000
23. Sasaki M, Sumi M, Kaneko K, et al. Multiparametric MR imaging for differentiating between benign and malignant thyroid nodules: initial experience in 23 patients. J Magn Reson Imaging. 2013;38(1):64–71. doi:10.1002/jmri.23948
24. Lu Y, Moreira AL, Hatzoglou V, et al. Using diffusion-weighted MRI to predict aggressive histological features in papillary thyroid carcinoma: a novel tool for pre-operative risk stratification in thyroid cancer. Thyroid. 2015;25(6):672–680. doi:10.1089/thy.2014.0419
25. Hao Y, Pan C, Chen W, et al. Differentiation between malignant and benign thyroid nodules and stratification of papillary thyroid cancer with aggressive histological features: whole-lesion diffusion-weighted imaging histogram analysis. J Magn Reson Imaging. 2016;44(6):1546–1555. doi:10.1002/jmri.25290
26. Shi R, Yao Q, Wu L, et al. T2* mapping at 3.0T MRI for differentiation of papillary thyroid carcinoma from benign thyroid nodules. J Magn Reson Imaging. 2016;43(4):956–961. doi:10.1002/jmri.25041
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.