Back to Journals » Patient Preference and Adherence » Volume 17
Assessing a Pharmacist-Enabled Intervention to Improve Adherence to Medication for Hypertension, Dyslipidemia, and Chronic Venous Circulation Disorders in Greece
Authors Golna C, Poimenidou C, Giannoukari EE , Saridi M, Liberopoulos E , Souliotis K
Received 17 July 2023
Accepted for publication 7 November 2023
Published 13 December 2023 Volume 2023:17 Pages 3341—3352
DOI https://doi.org/10.2147/PPA.S420811
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Christina Golna,1 Christina Poimenidou,1 Evdokia Elisavet (Evelyn) Giannoukari,1 Maria Saridi,2 Evangelos Liberopoulos,3 Kyriakos Souliotis1,4
1Research Department, Health Policy Institute, Maroussi, Greece; 2Faculty of Nursing, University of Thessaly, Larissa, Greece; 3First Department of Propaedeutic Internal Medicine, Medical School, Laiko General Hospital, National and Kapodistrian University of Athens, Athens, Greece; 4Department of Social and Education Policy, University of Peloponnese, Corinth, Greece
Correspondence: Kyriakos Souliotis, Email [email protected]
Background: Adherence to medication in chronic conditions may be influenced by interventions from pharmacists. This study aimed to assess the impact of guidance and reminders from pharmacists on adherence to medication for hypertension, dyslipidemia, and chronic venous circulation disorders (CVCD) in Greece.
Methods: The prospective CONCORD study aimed to record and report on change in self-reported adherence to medication following pharmacist reminders amongst a cohort of adult patients, diagnosed with at least one or a combination of these health conditions. All study participants were regular patients of a network of pharmacies in Attica and southern Greece. Pharmacists were trained to provide adherence reminders over 4 months. Impact on self-reported adherence of the intervention was reported at baseline and again in month 4.
Results: Of the 1146 participants, 48% were men and 60% were aged 55– 74 years. Among them, 23.7% were diagnosed with hypertension, 16.5% with dyslipidemia, 3% with CVCD, 42.5% with hypertension and dyslipidemia, 3.1% with hypertension and CVCD, 2.6% with dyslipidemia and CVCD, and 8.6% with dyslipidemia, hypertension, and CVCD. In month 4 vs month 0, patients were less likely to forget to take their prescribed medications (p< 0.001), to be careless about their medications during the last 30 days (p< 0.001), and to temporarily discontinue their medications without prior doctor’s advice (p< 0.001). Patients with CVCD were more prone to lower self-reported adherence compared to patients who were not diagnosed with CVCD or a combination of conditions that included CVCD.
Discussion: Reminders and advice from pharmacists resulted in higher adherence to medication amongst participants in month 4 versus month 0.
Conclusion: Pharmacist-enabled interventions, including reminders and advice, following targeted training, may positively impact on patient medication adherence in chronic health conditions.
Plain Language Summary: This study aimed to measure the impact of reminders and advice on adherence to medication provided by private pharmacists to patients with hypertension, dyslipidemia, and/or chronic venous circulation disorders (CVCD) in Greece. Patients were asked to self-report adherence to medication at months 0 and 4, following advice and reminders received from trained pharmacists. Self-reported adherence was significantly improved at month 4 vs month 0 across our sample. Our study showed that pharmacist-enabled interventions, following targeted training, can quickly and significantly improve adherence to medication in patients with chronic diseases in Greece.
Keywords: adherence, reminders, chronic non communicable diseases, pharmacist-enabled interventions, health policy
Introduction
Compliance with or adherence to medication and treatment guidelines has long been considered a critical contributor both to improved treatment outcomes and to patient satisfaction with therapy. It has also been shown to lower or avert the increase of disease-related medical costs.1–7 Nonetheless, and particularly as regards cardiovascular disease, adherence to medications remains a major challenge, with nonadherence leading to poor clinical outcomes, rehospitalizations, subsequent myocardial infarction, and increased mortality.8 Contributing factors to sub-optimal adherence include patient-related and treatment-related factors. The former are forgetfulness,9 denial,4 lack of motivation, cultural issues, low educational level or health literacy,10 alternate belief systems, and lack of proper physician–patient communication.11,12 The latter13 refer to limited treatment outcomes, failure to improve or maintain a patient’s health status, patient’s access to medications,9 complexity,14–18 cost and time of treatment, and side effects.6,19
To address this persistent challenge of nonadherence, the literature reports on several pharmacist-led interventions that have shown a positive impact on patients’ adherence to medication and clinical outcomes.4,5,20,21 For instance, enrollment in a medication adherence program in community pharmacies in New Zealand improved adherence, with individuals in the intervention group having 2.99 (95% CI: 2.79–3.20) greater odds of being adherent 12 months after the start of the study.20 Elsewhere, patients were telephoned by pharmacists monthly to assess changes in adherence to medication for diabetes, hypertension, or hyperlipidemia therapies over 6 months. Results confirmed a statistically significant improvement in adherence across all medication classes, with average adherence increasing by 11%.22
Community pharmacists are well-positioned for this purpose as 80% of medical treatments involve drug prescriptions.21 Among health care professionals, the pharmacist may be the most accessible healthcare provider, who maintains regular contact with patients.20 In addition, the community pharmacist’s role has evolved recently, from only dispensing medications to providing direct care to patients. For example, in Belgium, Finland, Italy, Switzerland, and the United Kingdom, pharmacists participate in health promotion and disease prevention, especially in rural areas.23 Pharmacist-led interventions may help reduce unnecessary provider visits, hospitalizations, and readmissions while strengthening integrated primary care delivery across the health system.24,25
In 2019, Greece had the highest number of community pharmacies per 100,000 population amongst all Organisation for Economic Cooperation and Development (OECD) countries (88 per 100,000 inhabitants vs an OECD-27 average of 28 per 100,000 inhabitants).26 These offer an array of services apart from dispensing medications, including regular measurement of blood pressure, vaccinations, health advice, etc., to which access is universal, widely available across the geographies of the country, and free of charge at the point of delivery. Nonetheless, they have not, to the best of our knowledge, been utilized in structured interventions to improve medication adherence in chronic conditions with a high prevalence, such as hypertension and dyslipidemia.
This paper reports on the results of a study to measure difference (Δ) in self-reported adherence to medication in a cohort of patients on chronic treatment for hypertension, dyslipidemia, and venous circulation disorders at month 4 vs month 0 in Attica and southern Greece, following trained pharmacist guidance and reminders. Conditions were selected based on their high prevalence (hypertension and dyslipidemia) and their out-of-pocket medication cost (chronic venous circulation disorders, CVCD). CVCD is a condition for which medications are not reimbursed by the National Organization for Health Services Provision (EOPYY) in Greece, therefore patients have to cover the cost for such medications themselves.
Materials and Methods
The study sample consisted of a cohort of adult patients on pharmaceutical treatment for hypertension, dyslipidemia, and/or CVCD. To be eligible to participate in the study, patients were required to visit the same Piraeus Pharmaceutical Association (PEIFASYN) pharmacy more than once a month. PEIFASYN is the second biggest single collaborative network of individual private pharmacies. Its presence is concentrated in Attica and southern Greece.
PEIFASYN selected 115 pharmacies from its 600 members, as a convenience sample, based on their willingness to participate in the study. Pharmacists in each of the participating pharmacies received virtual training to provide medication adherence reminders and support in dedicated seminars co-organized by PEIFASYN and the Health Policy Institute, with the support of Servier. Training during these seminars focused on communication skills to enhance patient–pharmacist relationship, including providing reminders to patients to adhere to their treatment regiments. Each pharmacy was requested to enroll 10 patients in the study. A folder was prepared for each patient, which included printouts of: (a) the informed consent form for completion by the patient (2 copies, one for the patient and one for the pharmacist’s records); (b) a revocation of informed consent form, to be used in cases when the patients wished to revoke his/her consent; and (c) a drop-out form, that was completed and retained by the pharmacist in cases of patient dropout due to, eg, death, hospitalization, etc. The folder also included a pharmacovigilance and safety reporting form to record any adverse events (AEs). The main survey tool included a cover sheet (Section A) with the anonymized patient characteristics. Section B included two identical questionnaires for the patient to complete (one in month 0 and one in month 4). Each document in the folder had a unique pharmacy ID and patient folder ID combination number. Pharmacists were also provided with a separate numbered sheet on which they would match number of each folder with patient name, contact details, and enrollment date – this sheet was for their records, was maintained solely by the pharmacists, and was destroyed by them upon the completion of the data collection process.
In month 0 (ie, at baseline), the pharmacist asked participants for their written consent to participate in the study and filled in Section A of the questionnaire that captured patient demographics, diagnosis, and current treatment. In cases of treatment switches, pharmacists were instructed to fill in a new form with new treatment details and file this in the patient folder. The patient was then given the Section B questionnaire to complete on his/her own. Section B probed into patient self-reported general health status, years on treatment, and medication adherence. The last-mentioned was assessed using 3 questions (B3–B5) with a 5-point Likert scale (from 1 – never to 5 – all the time) that was based on previous work by the researchers9 and is presented in Figure 1. Once baseline (month 0) measurement was completed, the pharmacist provided information and reminders to participating patients to take medication as prescribed during months 1, 2, and 3. Reminders highlighted the importance of adherence to medication as well as the risk of suboptimal or nonadherence or discontinuation of treatment without prior doctor’s advice. Impact of this intervention was evaluated again, using the same questionnaire at month 4.
 |
Figure 1 Patient self-reported adherence questionnaire. |
Data were extracted and statistical analysis carried out using R Core Team (2022). We conducted a Shapiro–Wilk test27 and a Kolmogorov–Smirnov test28 for each variable, and, depending on the data distribution (if it satisfied normality or not), we used either parametric or non-parametric methods. More specifically, to determine the effect of the intervention on patients’ treatment compliance between month 0 and month 4, we conducted a paired samples Wilcoxon test.29 Additionally, to examine the impact of the patient’s clinical diagnosis on medical adherence between month 0 and month 4, we conducted a Wilcoxon signed rank test.29 Furthermore, we used a paired samples Wilcoxon Test29 to explore the difference in adherence to treatment in month 0 vs month 4, relative to diagnosis and pill burden.
Results
A total of 1146 patients participated in the survey. Patient characteristics, clinical diagnosis, and current management are presented in Table 1.
 |
Table 1 Patient Characteristics, Clinical Diagnosis, and Current Management Status |
Patient Characteristics
Of patients participating in the study, 48% were male and 52% female; 97% were aged 45 or older, of whom 15% were 45–54 years old, 25% 55–64 years old, 35% 65–74 years old, and 22% 75+ years old. Over half (65.4%) of study participants lived in Attica, while the rest lived in southern Greece.
Clinical Diagnosis and Current Management
Of patients, 23.7% were diagnosed with hypertension, 16.5% with dyslipidemia, 3% with CVCD, 42.5% with hypertension and dyslipidemia, 3.1% with hypertension and CVCD, 2.6% with dyslipidemia and CVCD, and 8.6% with dyslipidemia, hypertension, and CVCD. Of participants with hypertension, 70% received their medication once per day, 24% twice per day, and 6% 3 or more times per day. Of patients with dyslipidemia, 92.7% received their medication once per day, while 7.3% received their medication 2 or more times per day. Finally, 56.5% of patients diagnosed with CVCD received their medication once per day, 34.2% twice per day, and over 9.3% 3 or more times per day.
Self-Reported General Health State
Most study participants (72%) rated their general health state as above average (60 or higher on a scale from 0 to 100), while 21% reported their general health state as average (between 40 and 60 on a scale from 0 to 100). The remainder (7%) rated their general health as below average.
Difference in Adherence Pre and Post Intervention
On average, it was less likely for patients to forget to take their prescribed medications, to be careless about their prescribed medications during the last 30 days, and to temporarily discontinue their medications without prior doctor’s advice during month 4 compared to month 0. Results are presented in Table 2. The median (M) represents the central tendency of our data values, and IQR represents a measure of spread.
 |
Table 2 Difference in Adherence Pre-Intervention (Month 1) and Post-Intervention (Month 4) |
Impact of Clinical Diagnosis on Adherence
Patients with dyslipidemia or/and hypertension were significantly less likely to: (a) forget to take their prescribed medications; (b) be careless about their prescribed medications during the last 30 days; and (c) temporarily discontinue their medications without prior doctor’s advice in month 4 compared to month 0. Patients with CVCD reported a non-significant positive impact on adherence across all 3 questions assessed post pharmacists’ reminders and advice (Table 3).
 |
Table 3 Impact of Pharmacist Intervention on Adherence According to Clinical Diagnosis |
Impact of Pill Burden on Adherence
We explored, with a paired samples Wilcoxon test,29 the difference in adherence to treatment in month 0 vs month 4, relative to diagnosis and pill burden, ie, for patients who were on a one-pill-a-day treatment vs more-than-one-pill-per-day. Our analysis revealed that pharmacists’ reminders and advice resulted in a statistically significant improvement in adherence to treatment in patients with dyslipidemia on one-pill-a-day and a non-significant improvement in patients with dyslipidemia on multiple-pills-a-day. Patients with CVCD had a lower chance to temporarily discontinue their medication without prior doctor’s advice when they were on one-pill-a-day medication. Moreover, pharmacists’ reminders had a statistically significant impact on adherence to medication in month 4 vs month 0 in all patients on treatment for hypertension, irrespective of pill burden (Table 4).
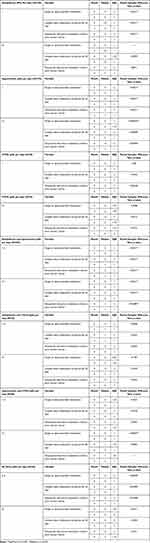 |
Table 4 Differences in Adherence to Treatment, in Month 0 vs Month 4, Relative to Diagnosis and Pill Burden |
Further, pharmacists’ reminders and advice resulted in a significant improvement in adherence in month 4 vs month 0 in patients diagnosed with both dyslipidemia and hypertension, and a non-significant improvement in patients diagnosed with both dyslipidemia and CVCD, irrespective of pill burden. Patients diagnosed with hypertension and CVCD, who were on more-than-2-pills-a-day, had a lower chance to forget to take their medications in month 4 vs month 0.
Lastly, pharmacists’ reminders had a significant impact on adherence to medication in month 4 vs month 0 in patients diagnosed with all 3 conditions, who were on 2-to-3-pills-a-day and a non-significant improvement in patients on more-than-3-pills-a-day.
Discussion
Pharmacies are emerging as a significant outpost for the implementation of impactful primary care interventions, including interventions to strengthen adherence to medication, and thus clinical outcomes, particularly in highly prevalent chronic conditions. In countries such as Greece, where the concentration of community pharmacies per 100,000 inhabitants is considerably higher than the European (and global) average, the exploration of the impact of such interventions in these facilities may inform decision-making on optimal allocation of resources. To the best of our knowledge, this is the first study in Greece to measure the impact on medication adherence of trained pharmacists’ reminders and advice to patients who are on treatment for highly prevalent, chronic conditions, ie, hypertension, dyslipidemia, and CVCD.
Our study revealed that patients in our cohort were significantly less likely to: (a) forget to take their prescribed medications; (b) be careless about their prescribed medications during the last 30 days; and (c) temporarily discontinue their medications without prior doctor’s advice in month 4 compared to month 0 (baseline), following reminders and advice from their pharmacists on the importance of adherence to medication. Our results were consistent across patient categories and diagnoses and were more pronounced for those on single-pill regimens in all 3 conditions. We confirmed that pharmacists’ interventions can have a significant and immediate impact on the level of adherence to medication in chronic conditions, including those that may be considered “silent” (eg, dyslipidemia). They also highlighted the need to consider interventions to strengthen adherence, even in patients on one-pill-a-day, despite preconceptions that these patients are more adherent. Also, they revealed a non-significant improvement in adherence amongst patients with CVCD. This is important as it refers to a condition for which patients must cover treatment cost out of their pocket, which has been shown to be a barrier to adherence.30,31
As the majority of patients in our study were aged 55–75, our findings are in line with previous meta-analyses on the impact of pharmacists’ interventions in older patients’ adherence. Marcum et al concluded that irrespective of type, pharmacist-led interventions resulted in a significant improvement in adherence to medication in older adults.5 In another intervention in the US,4 which targeted patients ≥65 years old, in nonadherent participants who in the process became adherent, the mean proportion of days covered (PDC) increased by 14%. In yet another study, from Canada, the presence of a pharmacist in primary care clinics increased patient self-management behaviors, including increased medication adherence.32
The immediate positive impact on adherence reported in our study confirmed results from a previous study by Spears et al,33 which improved adherence rates in antihypertensives, antihyperlipidemics, and antidiabetics immediately and increased adherence rates over 5 years. Equally, in another prospective quality-improvement study by Stanton-Robinson et al,34 consisting of pharmacist telephone interviews and interventions, 69.0% of patients with hypertension and 64.3% with diabetes reached a proportion of days covered (PDC) greater than 80% within 3 months, compared to baseline.
Limitations
This was a one-arm study without a control population. All participants received pharmacists’ reminders and advice. The study was performed in pharmacies located in Attica and southern Greece. There was no geographic representation of northern Greece in the sample of pharmacies and patients, but as both rural and urban areas of the country were included in the study, the authors are confident that the results are equally applicable to the northern part of the country, which has the same urban and rural characteristics. The patient sample skews towards older age groups, since older patients tend to be loyal to their pharmacist and visit the same pharmacy to fill their prescriptions. Younger patients may be driven by convenience to visit different pharmacies, eg, depending on current or temporary location. Further, the setting of the survey may bias results toward higher self-reported adherence than actual, as this is a survey administered by the pharmacist the patient regularly visits; therefore, it may be hard for the patient to admit to not taking prescribed medication as indicated. This limitation is partially addressed by our study design – this is a cohort study, therefore, any misrepresentations of actual levels of adherence would impact responses at both months 0 and 4 and, to this end, not impact on the difference in adherence between the 2 time points.
Conclusion
Guidance and reminders by community pharmacists improved adherence to medication for hypertension, dyslipidemia, and CVCD in Attica and southern Greece. Participants remembered more consistently to take their medications and were more compliant to doctors’ advice, following reminders from pharmacists, even within a short time frame of 4 months. This study may help to inform future interventions at the pharmacy level to further optimize adherence to medication amongst these critical patient groups and beyond, ie, among patient groups with chronic conditions managed in the community (outpatient) setting.
Data Sharing Statement
The authors are committed to sharing the full survey with qualified external researchers. The requests are to be made to the corresponding author and will be appraised based on scientific merit.
Ethics Approval and Consent to Participate
The study was approved by the Ethics Committee of the Health Policy Institute, Athens, Greece, and was conducted in line with the ethical standards set by the Declaration of Helsinki. Participation was voluntary and anonymized, and informed consent was requested and obtained from all participants.
Acknowledgments
We would like to thank the Board of Directors of PEIFASYN for fully supporting and facilitating this study and all participating PEIFASYN pharmacists for their enthusiasm, collaborative spirit, and diligence in implementing the study protocol. Early descriptive results of this study were presented at the 26th Annual Meeting of ESPACOMP, as a poster presentation. The poster’s abstract was published in “Abstracts of the 26th Annual Meeting of ESPACOMP, the International Society for Medication Adherence, Berlin, Germany, 17-19 November 2022” in the International Journal of Clinical Pharmacy, 2023 Feb 1;45(1):250–280. https://pubmed.ncbi.nlm.nih.gov/36725807/
Funding
This study was funded by Servier (Grant Number 19484/11 02 2021). The funding body had no role in the design of the study, data collection and analysis, interpretation of the data and in writing the manuscript.
Disclosure
K Souliotis has received advisory boards’ fees from Boehringer Ingelheim, Βristol Myers Squibb, and Pfizer; research grants from Sanofi and Roche. E Liberopoulos reports personal fees and non-financial support from Amgen, AstraZeneca; personal fees from Bayer, Viatris, Nova Nordisk, Recordati, Servier, Sanofi, Boehringer-Ingelheim, Lilly, Novartis, Chiesi, outside the submitted work. C Golna, C Poimenidou, E Giannoukari, and M Saridi report no potential conflicts of interest for this work.
References
1. Sabaté E. Adherence to Long-Term Therapies: Evidence for Action. World Health Organization. 2003.
2. Nieuwlaat R, Wilczynski N, Navarro T, et al. Interventions for enhancing medication adherence. Cochrane Database Syst Rev. 2014;11:Cd000011.doi:10.1002/14651858.CD000011.pub4
3. Dao N, Lee S, Hata M, Sarino L. Impact of appointment-based medication synchronization on proportion of days covered for chronic medications. Pharmacy. 2018;6(2). doi:10.3390/pharmacy6020044.
4. Daly CJ, Verrall K, Jacobs DM. Impact of community pharmacist interventions with managed care to improve medication adherence. J Pharm Pract. 2021;34(5):694–702. doi:10.1177/0897190019896505
5. Marcum ZA, Jiang S, Bacci JL, Ruppar TM. Pharmacist-led interventions to improve medication adherence in older adults: a meta-analysis. J Am Geriatr Soc. 2021;69(11):3301–3311. doi:10.1111/jgs.17373
6. Kleinsinger F. The unmet challenge of medication nonadherence. Perm J. 2018;22:18–033. doi:10.7812/tpp/18-033
7. Ruppar T, Ho PM, Garber L, Weidle PJ. Overcoming barriers to medication adherence for chronic diseases. CDC Public Health Grand Rounds. 2017.(pp. 1–2).
8. Baroletti S, Dell’Orfano H. Medication adherence In cardiovascular disease. Circulation. 2010;121(12):1455–1458. doi:10.1161/CIRCULATIONAHA.109.904003
9. Souliotis K, Giannouchos TV, Golna C, Liberopoulos E. Assessing forgetfulness and polypharmacy and their impact on health-related quality of life among patients with hypertension and dyslipidemia in Greece during the COVID-19 pandemic. Qual Life Res. 2022;31(1):193–204. doi:10.1007/s11136-021-02917-y
10. Pacleb A, Randall S, Neubeck L, Lowres N, Gallagher R. Health literacy and medication adherence in cardiac disease. Br J Card Nurs. 2018;13(11):545–554. doi:10.12968/bjca.2018.13.11.545
11. Barbouni A, Nalmpanti M, Gennimata D, Theodoridis D, Merakou K. Beliefs and practices of Greek doctors in relation to patients’ adherence to antihypertensive medication. J Hum Hypertens. 2017;31(5):341–346. doi:10.1038/jhh.2016.84
12. Voutsina P. Adherence to antihypertensive treatment and quality of life of patients who live in the area of responsibility of the Health Centre of Meligalas; 2016. in Greek. Available from: https://apothesis.eap.gr/archive/item/91255.
13. Marzec LN, Maddox TM. Medication adherence in patients with diabetes and dyslipidemia: associated factors and strategies for improvement. Curr Cardiol Rep. 2013;15(11):418. doi:10.1007/s11886-013-0418-7
14. Tsioufis K, Kreutz R, Sykara G, van Vugt J, Hassan T. Impact of single-pill combination therapy on adherence, blood pressure control, and clinical outcomes: a rapid evidence assessment of recent literature. J Hypertens. 2020;38(6):1016–1028. doi:10.1097/hjh.0000000000002381
15. Kalaitzidis RG, Panagiotopoulou T, Stagikas D, et al. Arterial stiffness, cognitive dysfunction and adherence to antihypertensive agents. is there a link to hypertensive patients? Curr Vasc Pharmacol. 2020;18(4):410–417. doi:10.2174/1570161117666190415112953
16. Liakos CI, Papadopoulos DP, Kotsis VT. Adherence to treatment, safety, tolerance, and effectiveness of perindopril/amlodipine fixed-dose combination in Greek patients with hypertension and stable coronary artery disease: a pan-hellenic prospective observational study of daily clinical practice. Am J Cardiol. 2017;17(5):391–398. doi:10.1007/s40256-017-0232-5
17. Sarafidis PA. Patient cases: 1. a patient with apparent Compliance. High Blood Press Cardiovasc Prev. 2015;22(1):15–18. doi:10.1007/s40292-015-0109-0
18. Fuller RH, Perel P, Navarro-Ruan T, et al. Improving medication adherence in patients with cardiovascular disease: a systematic review. Heart. 2018;104(15):1238–1243. doi:10.1136/heartjnl-2017-312571
19. Tedla YG, Bautista LE. Drug side effect symptoms and adherence to antihypertensive medication. Am J Hypertens. 2016;29(6):772–779. doi:10.1093/ajh/hpv185
20. Milosavljevic A, Aspden T, Harrison J. The impact of a community pharmacy service on patients’ medication adherence and ambulatory sensitive hospitalizations. Res Social Adm Pharm. 2020;16(7):904–913. doi:10.1016/j.sapharm.2019.09.059
21. Newman TV, San-Juan-Rodriguez A, Parekh N, et al. Impact of community pharmacist-led interventions in chronic disease management on clinical, utilization, and economic outcomes: an umbrella review. Res Social Adm Pharm. 2020;16(9):1155–1165. doi:10.1016/j.sapharm.2019.12.016
22. Colvin NN, Mospan CM, Buxton JA, Waggett JD, Gillette C. Using Indian health service (IHS) counseling techniques in an independent community pharmacy to improve adherence rates among patients with diabetes, hypertension, or hyperlipidemia. J Am Pharm Assoc. 2018;58(4):S59–S63. doi:10.1016/j.japh.2018.04.024
23. OECD. Realising the Potential of Primary Health Care. OECD Publishing; 2020.
24. Mossialos E, Courtin E, Naci H, et al. From “retailers” to health care providers: transforming the role of community pharmacists in chronic disease management. Health Policy (New York). 2015;119(5):628–639. doi:10.1016/j.healthpol.2015.02.007
25. Dwyer G, Popoola A, Seiler N, et al. Peer reviewed: chronic disease management service opportunities for community pharmacists during the COVID-19 pandemic. Prev Chronic Dis. 2022;2022:19.
26. OECD. Health at a Glance 2021: OECD Indicators. OECD Publishing; 2021.
27. Hanusz Z, Tarasinska J, Zielinski W. Shapiro–wilk test with known mean. Revstat Stat Jl. 2016;14(1):89–100. doi:10.57805/revstat.v14i1.180
28. Massey FJ Jr. The Kolmogorov-Smirnov test for goodness of fit. J Am Stat Assoc. 1951;46(253):68–78. doi:10.1080/01621459.1951.10500769
29. Rey D, Neuhäuser M. Wilcoxon-signed-rank test. Int Ency Stat Sci. 2011;2011:1658–1659.
30. McAdam-Marx C, Ruiz-Negron N, Sullivan JM, Tucker JM. The effects of patient out-of-pocket costs for insulin on medication adherence and health care utilization in patients with commercial insurance; 2007–2018. J Manag Care Spec Pharm. 2022;28(5):494–506. doi:10.18553/jmcp.2022.21481
31. Williams CP, Davidoff A, Halpern MT, et al. Cost-related medication nonadherence and patient cost responsibility for rural and urban cancer survivors. JCO Oncol Pract. 2022;18(8):e1234–e1246. doi:10.1200/op.21.00875
32. Erker R, Alefan Q, Goodridge D, et al. Evaluation of a medication safety and adherence program within a first nations community in Saskatchewan, Canada. J Am Pharm Assoc. 2021;61(1):e39–e45. doi:10.1016/j.japh.2020.08.001
33. Spears J, Erkens J, Misquitta C, Cutler T, Stebbins M. A pharmacist-led, patient-centered program incorporating motivational interviewing for behavior change to improve adherence rates and star ratings in a medicare plan. J Manag Care Spec Pharm. 2020;26(1):35–41. doi:10.18553/jmcp.2020.26.1.35
34. Stanton-Robinson C, Al-Jumaili AA, Jackson A, et al. Evaluation of community pharmacist-provided telephone interventions to improve adherence to hypertension and diabetes medications. J Am Pharm Assoc. 2018;58(4):S120–S124. doi:10.1016/j.japh.2018.04.03
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
