Back to Journals » Patient Preference and Adherence » Volume 17
Let Us Talk Treatment: Using a Digital Body Map Tool to Examine Treatment Burden and Coping Strategies Among Young People with a Chronic Condition
Authors van Schelven F , van der Meulen E, Wessels E, Boeije HR
Received 8 December 2022
Accepted for publication 9 February 2023
Published 2 March 2023 Volume 2023:17 Pages 517—529
DOI https://doi.org/10.2147/PPA.S400702
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Femke van Schelven,1 Eline van der Meulen,2 Elise Wessels,2,3 Hennie R Boeije1
1Department Perspective of Patients and Clients in Healthcare, Netherlands Institute for Health Services Research, Utrecht, the Netherlands; 2JongPIT, Amsterdam, the Netherlands; 3Department of Gastroenterology and Hepatology, Amsterdam University Medical Center, Amsterdam, the Netherlands
Correspondence: Femke van Schelven, Netherlands Institute for Health Services Research, Otterstraat 118, Utrecht, 3513, CR, the Netherlands, Email [email protected]
Purpose: Treatment for a chronic condition can pose a heavy burden on young people and affect their quality of life. The present study examined young people’s experiences with treatment burden and their coping strategies.
Patients and Methods: The body mapping method was employed, in which a life-sized outline of someone’s body is traced and populated with visual representations, symbols and words. For the present study, a digital tool for body mapping was developed. This is a chat robot which helps young people make a body map by asking questions about their lives, wellbeing and the influence of their treatment on this. In two series of three workshops, ten young people (16 to 25 years) with a chronic, somatic condition created individual body maps using this tool. The body maps were discussed in the group to obtain insight into experiences with treatment burden. The findings were analysed using thematic analysis. In all stages of the study, two adolescents with a chronic condition were involved as co-researchers.
Results: The results show that young people with a chronic condition experience considerable treatment burden. Although treatment reduces their symptoms, it also leads to physical and emotional side-effects, restrictions of meaningful activities, issues with future planning, reduced independence, and autonomy and loneliness. Young people apply several strategies to cope with this burden, such as seeking support from others, focusing on the positive, ignoring treatment advice, and seeing a psychologist.
Conclusion: Treatment burden is a subjective experience and not merely based on the number or types of treatment. It is therefore vital that young people with a chronic condition discuss their experiences with their care provider. This can help to tailor treatment decisions to their lives and needs.
Keywords: chronic disease, adolescence, self-management, treatment adherence, body mapping, visual methods
Introduction
It is widely known that a chronic, somatic condition can have a major impact on the lives and wellbeing of young people. It influences, for example, school outcomes,1 making friends,1,2 and participation in leisure activities, such as sports.2 These consequences are not solely of the condition, but also of its treatment. Taking medications, navigating health services and medical consultations can result in a heavy burden on young people and affect their quality of life and wellbeing,3 also known as treatment burden.
Treatment burden is an emerging topic and researchers have not yet agreed upon its definition. A recent review found that most definitions focus on the work and tasks that have to be performed for treatment and their impact on wellbeing.4 The definition formulated by Boyd et al was considered most thorough:
a patient’s perception of the aggregate weight of the actions and resources they devote to their health care, including difficulty, time and out-of-pocket costs dedicated to health care tasks, such as adhering to medications, dietary recommendations and self-monitoring.5
This definition predominantly focuses on devoted actions and resources, whereas the burden of treatment is also determined by the presence (or absence) of medication side-effects. Following the suggestions of Alsadah et al,4 we therefore explicitly include this in our definition of treatment burden.
Literature provides examples of ways treatment can disrupt the lives and wellbeing of young people with a chronic condition.6 Well-known examples are the physical side-effects of treatment, such as tiredness and nausea.7–13 Young people can also experience fear and shame as a consequence of their treatment.7,8,10,12,14–16 Another instance is the restrictions treatment poses on engagement in meaningful activities, such as going to school and hanging out with friends.7,10,17–19 Findings about treatment burden among young people with a chronic condition are however often part of broader studies on quality of life, treatment adherence and illness experience. There is a scarcity of studies explicitly focusing on experiences of treatment burden among this young patient group.
When seeking a balance between treatment burden and daily life, young people may apply several coping strategies. According to Lazarus and Folkman, two (non-mutually exclusive) types of coping exist: emotion-focused coping and problem-focused coping.20 The first aims to regulate emotional responses to a problem and the latter to manage or alter the problem. Studies on treatment burden among adult patients report the use of both types, such as distraction (emotion-focused), adapting daily routines (problem-focused) and searching online sources for information (both).6,21
Coping strategies can increase people’s capacity to deal with treatment burden,6,21,22 however some may also have detrimental effects. In the context of treatment burden, an example of such a strategy is “rationalised non-adherence”, ie patients deliberately decide to cease, modify or reduce treatment.6 In the short term, rationalised non-adherence may offer relief from treatment requirements. Though, in the long term it can have consequences on one’s health and quality of life. In addition, rationalised non-adherence can negatively impact the relation between patients and care providers,6 causing feelings of guilt and shame among patients and disappointment and disapproval among care providers. This can lead to mutual incomprehension and ineffective communication. Systematic reviews have suggested that especially young people are at risk of non-adherence.23,24 During the developmental period of adolescence, living a socially active life is likely to outweigh competing care priorities.25 Next to school and side-jobs, young people wish to spend time with friends and doing leisure activities.
Despite the importance of treatment burden and coping strategies, it receives limited attention.26 During consultations, care providers predominantly focus on physical effects of treatment.25,27 Limited attention is paid to the “immense social challenge of full adherence”, as worded by Oddleifson and Sawicki.25 Scientific studies also rarely explicitly focus on treatment burden. The present study therefore examined the following research question: what treatment burden do young people with a chronic condition experience and what coping strategies do they apply to minimise its consequences on their health and quality of life?
Materials and Methods
This study employed the method of body mapping, a visual and arts-based research method. Visual and arts-based methods are increasingly recognized as providing new ways to discuss issues that are difficult to articulate verbally.28 In body mapping, a life-sized outline of someone’s body is traced, which is then populated with visual representations, symbols and words related to the topic under study.29,30 A body map communicates a message such as “This is who I am, this is my story, and this is what is important to me”.29 The method of body mapping was considered an appropriate method to study treatment burden, as it allows young people to visually demonstrate the impact of their treatment inside and outside their bodies. Several studies have pointed out that body mapping provides rich insights in lived experiences and social contexts.29,30
Design
Two series of three body map workshops were organized to study the experiences of young people with a chronic condition with regards to treatment burden. Due to COVID-19 circumstances, it was not possible to apply the body mapping method in its traditional way. A digital tool for body mapping – the Map your Burden of Treatment (MyBoT) tool – was developed in collaboration with young people with a chronic condition. MyBoT is a chat robot which helps young people make a body map by asking questions about their lives, wellbeing, and the influence of their treatment. By answering the questions, young people build a personal body map in stepwise way. The first questions are general and intended to choose the background, figure and facial expression on the body map (Figure 1). Young people are asked, for example, how they are feeling right now. After that, young people fill their body map with self-chosen icons, pictures, photos and/or text, based on questions, such as “How does your treatment affect your body and life?”, “What things do you manage yourself in your treatment?”, “What things do you dislike in your treatment?” and “What would you like to discuss with your care provider?”. After completing the questions, young people can print their body map and discuss it with their care provider.
 |
Figure 1 Basis of a body map. Text on top reads: “Body map of XXX”. |
The development and application of this tool will be described in a separate paper. Body mapping using digital techniques is a relatively unexplored area, nevertheless according to De Jager et al it is promising, especially when used in conjunction with face-to-face workshops.29
Participants
Young people (16 to 25 years) who undergo treatment for a chronic, somatic condition were invited to participate. They were recruited using an recruitment call placed on the website of JongPIT, a Dutch foundation for and led by young people with a chronic condition. In total, ten young people participated in this study (Table 1). They had different chronic conditions, such as diabetes, rheumatism, cerebral palsy and scoliosis.
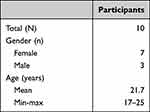 |
Table 1 Participants |
Data Collection
Two groups of four and six young people participated in three workshops, hosted by two members of the research team (FS and EM/EW). The workshops were conducted online, using Zoom. MyBoT was used as a means to discuss experiences with treatment burden. Guided by the hosts, participants went through the tool step-by-step. After each question, participants shared their experiences with treatment burden based on the additions they made to their body maps.
In the first workshop, the participants and hosts started with introducing themselves to each other. After that, MyBoT was introduced. Participants went through the first steps of the tool to create the basis of their personal body map, including a name, figure, face and background. Their wellbeing and the impact of treatment on their body was discussed based on some first icons they placed on their body map. In the second workshop, participants continued to fill their body map with icons, photos and text. Based on this, they discussed the activities they like to do now and in the future, the impact of their treatment on these activities and the positive impact of their treatment. Social support was addressed as well. The final workshop focused on coping strategies. Participants shared their experiences with different coping strategies, based on the icons and text they added to their body maps.
All workshops lasted one and a half hour. They were audio taped and transcribed verbatim.
Data Analysis
Thematic analysis was used to analyse the findings, namely becoming familiar with the data, generating initial codes, searching for themes, reviewing themes, defining and naming themes and reporting.31 Transcripts were analysed by the principal researcher (FS) and analyses were refined in discussions with the research team (HB, EM, EW). Relevant excerpts were marked and coded. The initial codes were based on the domains of treatment burden identified in a literature review on treatment burden of patients in general.6 To identify themes in the transcribed data, the research team discussed the codes and excerpts. Following these discussions, some additional excerpts were marked in the transcripts. In addition, it was chosen to merge and rename some of the initial codes. For example, “Feeling isolated and inadequately supported” and “Experiencing relationship strain” (domains identified in the literature review) were merged into one theme, namely “Loneliness”. “Living with uncertainty” was renamed “Future planning”. The themes and the relations between themes were discussed until consensus was reached. The MAXQDA-11 software package served as an aid in the coding process.
Patient and Public Involvement Statement
Two adolescents with a chronic condition were involved as co-researchers in the research team (EM, EW). They provided feedback on draft versions of the project proposal and co-designed the digital tool for body mapping that guided the workshops. All workshops were hosted by one researcher and one co-researcher. They had similar roles: they alternately took the lead in the discussions and asked follow-up questions. During data analysis, the co-researchers received all coded transcripts. With the principal researcher, they reflected on the fragments and codes until consensus was reached. The co-researchers also provided feedback on the drafts of this paper.
Results
The body mapping workshops provided rich insights, categorized in three groups: (a) the positive effects of treatment, (b) experienced treatment burden and (c) coping strategies. The findings are described below. Figure 2 provides an example of a body map that was created during the workshops.
Positive Effects of Treatment
Participants emphasize they need treatment to reduce the consequences of their condition. An important advantage of treatment is that it reduces symptoms. They experience less pain and are less tired, allowing them to do what matters to them, such as studying, meeting friends, and pursuing hobbies. This contributes to their sense of independence. Treatment can also be an educational experience, as young people learn to reflect, deal with setbacks, and stand up for themselves.
The positive thing about my treatment is that I wouldn’t be able to walk without it. And then I would still be wheelchair bound. – Female, 18 years
Treatment Burden
Physical Side-Effects
Young people report several direct side-effects of their treatment, such as pain, nausea, tiredness, obstipation, discomfort, and an increased heart rate. For some, these side-effects are always present, for others they are predominantly present during the first days after a specific treatment or change of medicines. Solely a few experience no direct side-effects of their treatment.
Nausea plays the biggest role in my life. Since I got sick, I have been stuffed with medication. This made me nauseous once and now I just keep being nauseous all the time. - Female, 23 years
Young people also describe some indirect physical side-effects of their treatment. For example, many agree that the stress and emotions experienced the days before a specific treatment, such as a hospital visit or a surgery, sometimes results in physical discomfort, such as abdominal pain or tiredness.
Emotions
Young people consider the emotional side-effects of their treatment more severe than the physical side-effects. Medication can directly influence their emotional wellbeing by causing mood swings. However, most emotions are indirect consequences of their treatment. Young people experience stress before hospital visits, since they fear that their care provider will not understand them or that treatment will cause discomfort or pain. Young people also experience stress or fear, when it is unclear what type of treatment can reduce their symptoms. Frustration is experienced, when they have to undergo treatments they do not want, when they have to explain their situation repeatedly to different care providers or when they are unable to get in contact with their care provider. Some young people described feeling sad, when treatment does not work or when recovery periods after surgery take longer than expected.
When I was diagnosed with [condition], I was afraid of what was going on. Nothing could be found, but I was sure there was something. When I was finally diagnosed, I was so happy. Then I knew what it was and I could stop being so scared. – Male, 20 years
Restriction of Meaningful Activities
Treatment restricts young people in doing activities that are meaningful to them. An example of such an activity is attending school. Some young people described not being able to attend school for longer periods of time, due to surgeries or medication that makes them feel sick. Others miss school more occasionally, for example, due to appointments with care providers.
Young people also find it difficult to find and keep a side job due to their treatment. One female participant wished to work at the local supermarket, but surgeries and lengthy recovery periods discourage employers to hire her. Another female participant takes medication that makes her too nauseous to work. Some do manage to find a (side) job. They find it bothersome that they sometimes have to cancel their work, for example, when hospital appointments are rescheduled during their working hours.
My brother works in the supermarket and I hear great things about it. But yeah, that won’t work for me. I can’t just say to my employer, ‘Yeah, bye. I’m not there for half a year, because I need an operation. That won’t work. – Female, 18 years
Treatments also restrict participation in activities with friends or family. Sometimes, family and friends plan activities on the day young people have to undergo treatment. For example, one female participant described she could not join an escape room, since she was tired of having her four week drip on that same day. Also, young people find it difficult to participate in activities that are planned spontaneously. Sometimes, they choose to undergo treatment at a time they normally spend time with friends to prevent they will miss another meaningful activity, such as school:
It really impacts friends and stuff. I always tried to plan treatment after school, because I did not want to miss it. However, the time after school is the time I normally spend with friends and then I have to cancel on them. – Female, 25 years
Another meaningful activity to young people is traveling. Several young people dream of going on a long backpacking trip. However, for many this is impossible due to their treatment. For example, a female participant described that she could not go away for more than three weeks, because she gets a drip every four weeks. Shorter vacations are also difficult and require good preparation. A vacation can disrupt eating and sleeping rhythms. Sometimes, young people have to teach the people they travel with to perform certain treatments, such as a massage or drip. A female participant described that she always has to make sure there is a refrigerator at her travel destination, so she can store her medicines.
Most people go on vacation to rest, but I actually find it more strenuous than staying at home. – Female, 25 years
Future Planning
Treatment affects young people’s future plans. Many young people adapt their educational aspirations to their condition and treatment. For example, one female participant chose to follow a lower level of education. This made it easier to keep up, despite her surgeries and long recovery periods. Another female participant quit school, since she was not able to meet the attendance requirements due to her treatment.
A fear of many young people is that their treatment will prevent them from starting their own family. For example, one female participant indicated that she worries that she will never find a partner who is willing to go through all her surgeries and recoveries. Having children was another issue. One female participant explained that she has to stop taking her medication during a possible pregnancy. She described that this worries her as this may worsen her condition. Another female participant also indicated that she worries about having children:
Having children is one of my biggest wishes. But I do not want to have children, if I still have to undergo those surgeries. What if they are one year old or something, and I cannot do anything with them for half a year or longer, because I have to recover from another surgery? – Female, 18 years
Independence and Autonomy
All young people agreed that they depend on their treatment to reduce the symptoms of their condition, but they also mentioned other ways in which treatment affected their independency. Most young people need the help of others to manage their treatment. Family members often help with drips or made appointments with care providers. Several young people feel dependent on others for transport to appointments with care providers because they cannot drive home after treatment themselves.
I would like to be less dependent on my drip, which is done every four weeks by a nurse at my home. That I can do the injections myself. Then I can also say I do it on Friday evening or during the weekend, if that suits me better. – Female, 20 years
Loneliness
Despite being surrounded by loving family and friends, young people reported feeling lonely due to their treatment. One male participant said: “being lonely is not the same as being alone”. Sometimes young people feel lonely, when they are (unintentionally) excluded. For example, sometimes a day out is planned on the same day young people have a hospital appointment, which means that they cannot join. Young people who are often absent from school reported they lost many friends. While they undergo and manage their treatment, their friends go on with their lives. This creates distance and feelings of loneliness.
Incomprehension is another important cause of loneliness. Young people experience that others can never fully understand what treatment burden means and how this affects their lives. It is common for young people to be advised to try yoga or a new diet to “cure” their condition. A female participant explained that her friends keep asking why her surgeries did not cure here yet. For young people, this feels like trivializing their experiences and problems.
My mother is always there for me. But she does not understand my situation. She never had surgery. And neither does my father. So I’m really alone in that. And well, my dog really helps with that, that sound very stupid, but a dog sometimes understands you better than people. – Female, 18 years
Coping with Treatment Burden
Seeking Support from Others
Virtually all young people received support from family and friends. They assist in carrying out treatment and help them to ask questions they are afraid to ask or forget during consultations with care providers. Other forms of support are taking care of young people when they are recovering from treatment and arranging transport to appointments with care providers. Family and friends also provide emotional support. They provide comfort when a treatment is not going well or distract young people when they are stressed for an unpleasant treatment. Talking with family and friends about treatment burden makes them feel less lonely.
Sometimes, things can get really stuck in my head. It makes such a huge difference, when I can just talk to my friend or parents. That is very different from my treatment team, I see them only once in a while. - Female, 24 years
Some young people have a family member or friend with a similar chronic condition. This is valuable as they have a better understanding of treatment burden. However, not everyone has a family or friend with a similar chronic condition. Therefore, some young people seek contact with peers with a chronic condition on social media or online forums to exchange experiences and tips.
Finally, young people mentioned that their pet was an important support for them. Cuddling and talking to a pet helps them to cope with their emotions. A number of young people have an assistance dog. These offer practical support, such as sounding an alarm in the event of an epileptic seizure, opening doors or picking up things.
Focusing on the Positive
Young people try to stay positive. They do this by focusing on the things they can do, enjoying moments of happiness even more and being proud of themselves. Some young people reward themselves with a gift after (unpleasant) treatment. Although focusing on the positive helps them, young people also warn that it should not go too far. Some young people feel they are putting on a mask. They tell everyone they are doing fine, even though they are not. This makes them feel lonely and hinders successful treatment, as they are not honest about its consequences.
I try to think about all the possibilities and not focusing on the limitations. Some people see a solution for every problem and others see a problem for every opportunity. I’d like to be part of the first group. – Female, 23 years
Ignoring Treatment Advice
Sometimes young people do not follow the advice of their care provider to reduce treatment burden. A few stopped a specific treatment or chose not to do a recommended surgery. Young people also postpone treatments. A female participant said that she walked with a broken foot for six months, as she did not want to get a cast again. However, most decisions to ignore treatment advice concern smaller decisions in everyday life. For example, young people sometimes (purposely) forget to perform the advised physical exercises, to take medication or to rest sufficiently. Some young people described they (occasionally) drink alcohol, even though their care providers advised against this due to their prescribed medication.
Officially I have to eat every two hours, otherwise I will get a hypo, because my body is making too much insulin. But that’s not in my system yet and I just find that really difficult, because I’m just not much of an eater. So that’s something I rarely succeed in doing. – Female, 24 years
Seeing a Psychologist
As noted before, young people experience negative emotions from their treatment. Most young people in the workshops therefore choose to see a psychologist. Talking to an objective person helps them to see their own situation differently. Psychologists also help young people to make treatment choices by discussing the benefits and burden of a specific treatment.
I am currently seeing a psychologist. She made me realize that the way I am dealing with my treatment has an impact on how I am doing. Even when you think you are doing very well, you can sometimes do a little better. – Female, 25 years
Other Ways to Cope
The previous ways of coping with treatment burden are most often mentioned by young people. They also mentioned some other ways. Some young people look for information on the internet to reduce their treatment burden. They read about, for example, the latest technological developments and (homeopathic) remedies that could help as a supplement to their medication. Others try to reduce the side effects of their treatment by eating healthy and exercising. Some try to become more independent by learning how to do (parts of) their treatment themselves, such as getting a drip.
Discussion
The present study examined treatment burden and coping strategies among young people with a chronic, somatic condition. It was found that young people experience a considerable treatment burden. Treatment reduces symptoms of their chronic condition, but also leads to physical and emotional side-effects, restrictions of meaningful activities, issues with future planning, reduced independence and autonomy and loneliness.
The findings support existing research on quality of life, treatment adherence and illness experience among young people with a chronic condition.7,8,11,13,32 To our knowledge, the present study is the first to explicitly focus on treatment burden among a young patient group. We found that some issues young people experience are similar to those of adults, such as physical side-effects, negative emotions, and disruptions in daily life.33–35 In addition to this, young people struggle with the impact of treatment on future planning and becoming independent from their family. Adolescence is a period in life in which many developmental milestones are achieved, such as finishing school, finding a partner, and starting a family.36,37 Young people with a chronic condition generally lag behind in this transition to adulthood,36,38 and our results indicate that treatment burden contributes to this. For example, the loss of friends and a limited social life due to treatment can have implications for later social development and relationships.39 Additionally, restriction of meaningful activities such as finding a side job and going on long backpacking trips inhibits trying out new things and developing into an independent adult.39
Although young people were not always able to clearly distinguish between the consequences of treatment and the condition itself, the concept of treatment burden appeared to be helpful to reflect on treatment choices. Their reflections showed that treatment burden is highly subjective. In fact, emotional side-effects of treatment were considered more severe than physical side-effects. This finding implicates that we should not only include physical side-effects in Boyd’s definition of treatment burden, but also emotional side-effects, such as fear, frustration, and sadness.4,5 Another finding is that young people with different treatments had similar experiences and coping strategies, and the other way around. This is in line with studies stating that treatment burden is not merely a simple count of types of treatment.21,40,41 The way young people experience and cope with treatment burden depends on various factors, such as personal characteristics, social context and resources.21 For example, more outspoken young people with an extensive social network may find a specific treatment less burdening than less outspoken young people with a limited social network. This finding underscores that treatment burden is about perspective, as Boyd et al point out in their definition.5
Although treatment burden cannot be completely resolved, young people with a chronic condition apply several coping strategies to reduce it. As they considered treatment mainly emotionally burdening, they applied many emotional-focused coping strategies, such as seeking for emotional support from family, friends and pets, seeing a psychologist and focusing on the positive. Other studies have confirmed that these strategies can be helpful in reducing stress and burden.21,42 In line with a study by Serlachius et al, participants noted that suppressing emotions is an emotion-focused coping strategy with potentially detrimental effects.43 Examples of problem-focused strategies that participants applied were looking for information, adapting life style, and asking practical support from family and friends. These strategies are helpful to incorporate treatment in daily life and routines.21,42
A much discussed and potentially maladaptive coping strategy is rationalized non-adherence.6,44–46 In the present study, young people with a chronic condition recognized that they needed treatment to reduce symptoms of their chronic condition, but sometimes the perceived psychosocial costs outweighed the medical benefits. Consequently, they did not only adapt daily life to their treatment, but also the other way around. In line with Rapoff and Calkins-Smith, we argue that the ultimate goal of medical care is not strict adherence to (medically speaking) the most optimal form of treatment, but improving health and quality of life.45 Therefore, a balance needs to be found between medical benefits of treatment and an acceptable psychosocial treatment burden.45,46 This requires good patient-provider communication and shared decision making to complement medical knowledge with experiential knowledge.46,47 Insight in experienced treatment burden can help care providers and young people to tailor treatment decisions to daily live, increase adherence, and improve health and quality of life.
On a larger scale, the attention for treatment burden during consultations between young people and care providers can be increased by including treatment burden in clinical guidelines.48 In the Netherlands, the quality standard ‘Psychosocial care in case of chronic conditions’ draws attention to the importance of talking about the psychosocial consequences of chronic conditions and treatment.49 On a smaller scale, young people with a chronic condition and care providers may benefit from practical tools that support communication about treatment burden, such as MyBoT. Although we applied MyBoT in a research setting, our experiences show promising results for the clinical setting as well. In line with previous studies, we found that the visual and arts-based method of body mapping provided rich insights in lived experiences.29,30 MyBoT helped young people with a chronic condition to tell their personal stories, as they could visualize and show their experiences before discussing them. This was very helpful in discussing important and sensitive topics such as emotions, losing friends and having children.
Patient and Public Involvement
Two adolescents with a chronic condition (EM, EW) were involved in all stages of the present study. Due to their enthusiasm and dedication to the research topic, they contributed more than expected. Initially, it was agreed upon that they would be involved during the early stages of the study. After data collection, the adolescents expressed the wish to be involved in the processing of the data they helped collect. Therefore, they also contributed to data analysis and writing this manuscript. Both the researchers and adolescents considered their collaboration a valuable experience. The adolescents were considered equal partners in the research process.
The adolescents added value to the study in different ways. First, they helped create an open and safe atmosphere during the workshops. Participants appreciated the presence of a host with lived experience. The adolescents made it easier for participants to share their experiences by sharing some of their own. Second, the adolescents asked additional questions relevant to the lives of young people with a chronic condition. For example, future planning was not a big topic in MyBoT, but follow-up questions of the adolescents showed that it was an important topic. Third, as co-authors they made sure that relevant aspects received sufficient attention in this manuscript. For example, they emphasized the importance of also highlighting the positive effects of treatment.
Strengths and Limitations
The present study examined treatment burden among a young patient group, using an innovative, digital tool for body mapping. This provided valuable insights into their lived experiences. We believe, however, that physical workshops would have facilitated more discussion between participants than online workshops. Despite this, we also discovered some advantages of digital workshops. It enabled participation from home, which is an important advantage for young people who have to cope with a chronic condition and its treatment. Additionally, participants were allowed to participate at their own pace, since they could turn off their cameras and microphones. This created an environment in which they felt safe to share emotional experiences. Another limitation of this study is that we studied treatment burden among a relatively small group of ten young people with different chronic conditions. Although we found similar experiences across different treatments and conditions, it would be interesting to repeat this study among a larger group to improve the generalizability of the findings.
Conclusion
Young people with a chronic condition experience a considerable treatment burden. It is vital that they discuss their experiences with their care provider as this can help to tailor treatment decisions to their lives and needs, as well as to find coping strategies that help them deal with treatment burden. There is also a need for more research on the topic of treatment burden, as it can provide valuable insights into young people’s treatment choices, non-adherence and patient-provider relations. The visual and arts-based method of body mapping can be a useful aid in discussing treatment burden in care and research settings.
Data Sharing Statement
Data are available from the corresponding author upon reasonable request.
Ethics Approval and Informed Consent
The present study complies with the Declaration of Helsinki. All participants provided informed consent at the start of the first workshop. This included the publication of anonymized responses. The Medical Ethics Committee (METc) of the University Medical Centre Utrecht concluded that this study is not a clinical research with human subjects as meant in the Medical Research Involving Human Subjects Act (WMO). Further ethical approval of this study was therefore not required under Dutch legislation. All participants and co-researchers received reimbursement for their contribution to the study.
Acknowledgments
The authors would like to thank Martha Grootenhuis, Tiny van Merode, and Sanne Nijhof for their valuable feedback during all phases of this research project.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
The research was funded by Agis Innovatiefonds, Amersfoort grant number 2019-16.
Disclosure
Dr Femke van Schelven reports grants from Agis Innovatiefonds, during the conduct of the study. Dr Hennie Boeije reports grants from Agis Innovatiefonds, during the conduct of the study. The authors report no conflicts of interest in this work.
References
1. Lum A, Wakefield CE, Donnan B, et al. Understanding the school experiences of children and adolescents with serious chronic illness: a systematic meta-review. Child Care Health Dev. 2017;43(5):645–662. doi:10.1111/cch.12475
2. Tonkin BL, Ogilvie BD, Greenwood SA, Law MC, Anaby DR. The participation of children and youth with disabilities in activities outside of school: a scoping review. Can J Occup Ther. 2014;81(4):226–236. doi:10.1177/0008417414550998
3. Eton D, Ridgeway J, Egginton J, et al. Finalizing a measurement framework for the burden of treatment in complex patients with chronic conditions. Patient Relat Outcome Meas. 2015;6:117. doi:10.2147/prom.s78955
4. Alsadah A, van Merode T, Alshammari R, Kleijnen J. A systematic literature review looking for the definition of treatment burden. Heliyon. 2020;6(4):e03641. doi:10.1016/j.heliyon.2020.e03641
5. Boyd CM, Wolff JL, Giovannetti E, et al. Healthcare task difficulty among older adults with multimorbidity. Med Care. 2014;52(3):118–125. doi:10.1097/MLR.0b013e3182a977da
6. Demain S, Gonçalves AC, Areia C, et al. Living with, managing and minimising treatment burden in long term conditions: a systematic review of qualitative research. PLoS One. 2015;10(5):e0125457. doi:10.1371/journal.pone.0125457
7. Taylor RM, Franck LS, Dhawan A, Gibson F. The stories of young people living with a liver transplant. Qual Health Res. 2010;20(8):1076–1090. doi:10.1177/1049732310368405
8. Stasiulis IE, Gladstone B, Boydell IK, et al. Children with facial morphoea managing everyday life: a qualitative study. J Dermatol. 2018;179:245–246. doi:10.1111/bjd.16449
9. Lam CG, Cohen KJ, Roter DL. Coping needs in adolescents with cancer: a participatory study. J Adolesc Young Adult Oncol. 2013;2(1). doi:10.1089/jayao.2012.0011
10. Nicholas DB, Picone G, Selkirk EK. The lived experiences of children and adolescents with end-stage renal disease. Qual Health Res. 2011;21(2):162–173. doi:10.1177/1049732310382789
11. Cartwright T, Fraser E, Edmunds S, Wilkinson N, Jacobs K, Cartwright T. Journeys of adjustment: the experiences of adolescents living with juvenile idiopathic arthritis. Child Care Health Dev. 2015;41(5):734–743. doi:10.1111/cch.12206
12. De Simoni A, Horne R, Fleming L, Bush A, Griffiths C. What do adolescents with asthma really think about adherence to inhalers? Insights from a qualitative analysis of a UK online forum. BMJ Open. 2017;7:6. doi:10.1136/bmjopen-2016-015245
13. Livermore P, Gray S, Mulligan K, Stinson JN, Wedderburn LR, Gibson F. Being on the juvenile dermatomyositis rollercoaster: a qualitative study. Pediatr Rheumatol. 2019;17:30. doi:10.1186/s12969-019-0332-7
14. Ridosh M, Braun P, Roux G, Bellin M, Sawin K, Ridosh M. Transition in young adults with spina bifida: a qualitative study. Child Care Health Dev. 2011;37(6):866–874. doi:10.1111/j.1365-2214.2011.01329.x
15. Sliwinski SK, Gooding H, de Ferranti S, et al. Transitioning from pediatric to adult health care with familial hypercholesterolemia: listening to young adult and parent voices. J Clin Lipidol. 2017;11:147–159. doi:10.1016/j.jacl.2016.11.001
16. Poti S, Emiliani F, Palareti L. Subjective experience of illness among adolescents and young adults with diabetes: a qualitative research study. J Patient Exp. 2018;5(2):140–146. doi:10.1177/2374373517738234
17. Kirk S. How children and young people construct and negotiate living with medical technology. Soc Sci Med. 2010;71(10):1796–1803. doi:10.1016/j.socscimed.2010.07.044
18. Aoto H, Nakatani H, Kanayama S, Okada SI, Fukada M, Hanaki K. Qualitative analysis of the psychosocial adaptation process in children with chronic kidney disease: toward effective support during transition from childhood to adulthood. Yonago Acta Med. 2018;61(3):166–174. doi:10.33160/yam.2018.09.004
19. Assa A, Ish-Tov A, Rinawi F, Shamir R. School attendance in children with functional abdominal pain and inflammatory bowel diseases. J Pediatr Gastroenterol Nutr. 2015;61(5):553–557. doi:10.1097/MPG.0000000000000850
20. Lazarus RS, Folkman S. Stress, Appraisal and Coping. Springer Publishing Company; 1984.
21. Ridgeway J, Eton DT, Egginton JS, et al. Factors that lessen the burden of treatment in complex patients with chronic conditions: a qualitative study. Patient Prefer Adherence. 2014;8:339–351. doi:10.2147/PPA.S58014
22. Shippee ND, Shah ND, May CR, Mair FS, Montori VM. Cumulative complexity: a functional, patient-centered model of patient complexity can improve research and practice. J Clin Epidemiol. 2012;65(10):1041–1051. doi:10.1016/j.jclinepi.2012.05.005
23. Lemay J, Waheedi M, Al-Sharqawi S, Bayoud T. Medication adherence in chronic illness: do beliefs about medications play a role? Patient Prefer Adherence. 2018;12:1687–1698. doi:10.2147/PPA.S169236
24. Gast A, Mathes T. Medication adherence influencing factors—an (updated) overview of systematic reviews. Syst Rev. 2019;8(1):112. doi:10.1186/s13643-019-1014-8
25. Oddleifson DA, Sawicki GS. Adherence and recursive perception among young adults with cystic fibrosis. Anthropol Med. 2017;24(1):65–80. doi:10.1080/13648470.2017.1278865
26. Powell P, Saggu R, Jones S, et al. Discussing treatment burden. Breathe. 2021;17(1):200284. doi:10.1183/20734735.0284-2020
27. Schofield LM, Horobin HE. Growing up with primary ciliary dyskinesia in Bradford, UK: exploring patients experiences as a physiotherapist. Physiother Theory Pract. 2014;30(3):157–164. doi:10.3109/09593985.2013.845863
28. Harrison B. Seeing health and illness worlds - using visual methodologies in a sociology of health and illness: a methodological review. Sociol Health Illn. 2002;24(6):856–872. doi:10.1111/1467-9566.00322
29. de Jager A, Tewson A, Ludlow B, Boydell KM. Embodied ways of storying the self: a systematic review of body-mapping. Forum Qual Sozialforschung. 2016;17(2). doi:10.17169/fqs-17.2.2526
30. Dew A, Smith L, Collings S, Dillon Savage I. Complexity embodied: using body mapping to understand complex support needs. Forum Qual Sozialforschung. 2018;19(2). doi:10.17169/fqs-19.2.2929
31. Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101. doi:10.1191/1478088706qp063oa
32. Green A, Meaux J, Huett A, Ainley K. It has its ups and downs”: adolescents’ quality of life after heart transplantation. Prog Transplant. 2011;21(2):115–120. doi:10.1177/152692481102100205
33. Eton D, Ramalho de Oliveira D, Egginton J, et al. Building a measurement framework of burden of treatment in complex patients with chronic conditions: a qualitative study. Patient Relat Outcome Meas. 2012;3:39–49. doi:10.2147/PROM.S34681
34. Jordan S, Philpin S, Warring J, Cheung WY, Williams J. Percutaneous endoscopic gastrostomies: the burden of treatment from a patient perspective. J Adv Nurs. 2006;56(3):270–281. doi:10.1111/j.1365-2648.2006.04006.x
35. Sav A, Kendall E, Mcmillan SS, et al. “You say treatment, I say hard work”: treatment burden among people with chronic illness and their carers in Australia. Health Soc Care Community. 2013;21(6):665–674. doi:10.1111/hsc.12052
36. Waldboth V, Patch C, Mahrer-Imhof R, Metcalfe A. Living a normal life in an extraordinary way: a systematic review investigating experiences of families of young people’s transition into adulthood when affected by a genetic and chronic childhood condition. Int J Nurs Stud. 2016;62:44–59. doi:10.1016/j.ijnurstu.2016.07.007
37. Taylor RM, Gibson F, Franck LS. The experience of living with a chronic illness during adolescence: a critical review of the literature. J Clin Nurs. 2008;17(23):3083–3091. doi:10.1111/j.1365-2702.2008.02629.x
38. Maurice-Stam H, Nijhof SL, Monninkhof AS, Heymans HSA, Grootenhuis MA. Review about the impact of growing up with a chronic disease showed delays achieving psychosocial milestones. Acta Paediatr. 2019;108:2157–2169. doi:10.1111/apa.14918
39. Stam H, Hartman EE, Deurloo JA, Groothoff J, Grootenhuis MA. Young adult patients with a history of pediatric disease: impact on course of life and transition into adulthood. J Adolesc Health. 2006;39(1):4–13. doi:10.1016/j.jadohealth.2005.03.011
40. Sav A, King MA, Whitty JA, et al. Burden of treatment for chronic illness: a concept analysis and review of the literature. Health Expect. 2015;18(3):312–324. doi:10.1111/hex.12046
41. Cameron RA, Office D, Matthews J, et al. Treatment preference among people with cystic fibrosis. Chest. 2022;162(6):1241–1254. doi:10.1016/j.chest.2022.07.008
42. Pennant S,C, Lee S, Holm S, et al. The Role of Social Support in Adolescent/Young Adults Coping with Cancer Treatment. Children. 2019;7(1):2. doi:10.3390/children7010002
43. Serlachius A, Frydenberg E, Northam E, Cameron F. Qualitative study exploring coping strategies in youth with type 1 diabetes. Children Australia. 2011;36(3):144–152. doi:10.1375/jcas.36.3.144
44. McGrady ME, Hommel KA. Medication adherence and health care utilization in pediatric chronic illness: a systematic review. Pediatrics. 2013;132(4):730–740. doi:10.1542/peds.2013-1451
45. Rapoff MA, Calkins‐Smith A. Enhancing treatment adherence in young people with chronic diseases. In: The Wiley Handbook of Healthcare Treatment Engagement. Wiley; 2020:354–364. doi:10.1002/9781119129530.ch19
46. Pai A, Ostendorf HM. Treatment adherence in adolescents and young adults affected by chronic illness during the health care transition from pediatric to adult health care: a literature review. Child Health Care. 2011;40(1):16–33. doi:10.1080/02739615.2011.537934
47. Schaefer MR, Kavookjian J. The impact of motivational interviewing on adherence and symptom severity in adolescents and young adults with chronic illness: a systematic review. Patient Educ Couns. 2017;100(12):2190–2199. doi:10.1016/j.pec.2017.05.037
48. Dobler CC, Harb N, Maguire CA, Armour CL, Coleman C, Murad MH. Treatment burden should be included in clinical practice guidelines. BMJ. 2018;363:k4065. doi:10.1136/bmj.k4065
49. Werkgroep psychosociale zorg bij een ingrijpende somatische aandoening. Kwaliteitsstandaard Psychosociale Zorg Bij Somatische Aandoeningen[Working group on psychosocial care in case of a major somatic disorder. Quality Standard Psychosocial Care for Somatic Disorders]; 2019. in Dutch.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

