Back to Journals » ClinicoEconomics and Outcomes Research » Volume 12
Antipsychotic Medication Adherence and Healthcare Services Utilization in Two Cohorts of Patients with Serious Mental Illness
Authors Forma F , Green T, Kim S, Teigland C
Received 14 September 2019
Accepted for publication 29 January 2020
Published 14 February 2020 Volume 2020:12 Pages 123—132
DOI https://doi.org/10.2147/CEOR.S231000
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Samer Hamidi
Felicia Forma,1 Teresa Green,2 Seung Kim,2 Christie Teigland2
1Otsuka Pharmaceutical Development & Commercialization, Inc., Princeton, NJ, USA; 2Avalere Health — an Inovalon Company, Washington, DC, USA
Correspondence: Christie Teigland Email [email protected]
Objective: To evaluate differences in patient characteristics and real-world outcomes in two distinct high-risk cohorts of patients with serious mental illness (SMI).
Methods: Retrospective cross-sectional analysis using a national multi-payer claims database. Two SMI cohorts identified by a technical expert panel—patients recently discharged (RD) from an SMI-related hospitalization and early episode (EE) patients—were evaluated for antipsychotic medication adherence, healthcare utilization, and spending patterns.
Results: The analysis included 51,705 patients with bipolar disorder, major depressive disorder, and schizophrenia. More than half were over age 46 and > 60% were female. Adherence to psychiatric medications was low (52.5% RD and 16.1% EE). More than half of RD and 100% of EE patients switched medications at least once annually, but 19% of RD patients switched ≥ 2 times compared to 14% of EE. The RD cohort (generally older and sicker) had higher psychiatric related utilization and higher annual costs (US$21,171 versus US$15,398). In both cohorts, women were more likely to have an emergency department (ED) and primary care provider (PCP) visit, but less likely to be hospitalized. Patients age < 46 were less likely to have a PCP visit and more likely to have an ED visit, but younger patients age 18– 24 were less likely to be hospitalized.
Conclusion: Efforts to manage SMI are confounded by heterogeneity and low adherence to treatment. By better understanding which patients are at higher risk for specific adverse outcomes, clinicians can target interventions more appropriately to reduce the significant burden of SMI.
Keywords: adherence, schizophrenia, major depressive disorder, bipolar disorder, healthcare utilization
Introduction
Approximately 10.4 million (4.2%) American adults have a diagnosis of serious mental illness (SMI), which is defined by the National Institutes of Health as a mental, behavioral, or emotional disorder resulting in serious functional impairment, which substantially interferes with or limits one or more major life activities including the three most common diagnoses of bipolar disorder, major depressive disorder (MDD), and schizophrenia.1,2 These mental diseases are often first diagnosed in early adulthood and are among the leading causes of disability in many parts of the world.3,4 The economic impact of SMI cannot be overstated: estimates report the economic costs of SMI are nearly US$200 billion in lost earnings each year in the United States5 and up to US$2.5 trillion worldwide.6 Despite the high prevalence and significant burden of SMI, only two-thirds of individuals suffering from SMI receive treatment for their condition.2 Although there are numerous evidence-based interventions, including pharmacotherapy,7–10 adherence to recommended treatment medications is a significant problem. Several studies have estimated that as many as 50% of patients with SMI are nonadherent to their prescribed treatment regimen.11–14
Nonadherence to SMI treatment is associated with poor outcomes, including psychiatric hospitalization, relapse, negative social outcomes (e.g., arrest, job loss), and increased risk of attempted suicide.15–18 It is estimated that nonadherence to therapy for mental illness costs up to US$20,000 per patient annually due to the aforementioned negative outcomes.19 Broadly, because SMI encompasses diverse conditions, a better understanding of the patterns of care and adherence to antipsychotic treatment among patients in different stages of the disease cycle can help clinicians identify individual patients for additional support and interventions.13,20–25 Our study used comprehensive medical and pharmacy claims data for a national sample of patients diagnosed with SMI to determine if there were differences in treatment adherence, healthcare utilization, and costs among two distinct cohorts of patients at different stages of the disease.
Methods
We conducted a retrospective cross-sectional analysis using data from Inovalon’s Medical Outcomes Research for Effectiveness and Economics (MORE2) Registry® to compare patient characteristics, outcomes, healthcare utilization, and costs in patients with SMI. MORE2 is a large, nationally representative data warehouse of healthcare administrative claims data that includes 100% of Medicare Fee-for-Service (FFS) claims as well as data sourced from more than 150 health plans across the nation through HIPAA compliant Data Use Agreements. MORE2 is statistically de-identified by expert determination following the strictest privacy rules and has exempt IRB status.26 The inputs from this study are from real-world usage of medication and are not part of any human research trials and as such are not covered under the Declaration of Helsinki. The data include longitudinal information about patient demographics, enrollment, diagnoses, medical encounters, pharmacy records, and laboratory results for more than 250 million unique individuals across all geographic regions in the US in various healthcare settings and provider specialties. These data span multiple payer types in the US, including 100% of traditional Fee-for-Service (FFS) Medicare Parts A, B and D provided by the Centers for Medicare and Medicaid Services (CMS) under a research DUA and Inovalon’s status as a Qualified Entity, patients covered by private health insurance (ie, commercial insurers), Medicare beneficiaries covered by private Medicare Advantage plans which consist primarily of health maintenance organizations (HMOs) and preferred provider organizations (PPOs), and Medicaid Managed Care which includes patients enrolled in private insurance plans that a state has contracted with to provide Medicaid benefits on behalf of the state.
The focus of the analysis was patients with SMI which was defined as having a diagnosis for one or more of three of the most common conditions of bipolar disorder, major depressive disorder (MDD), or schizophrenia during the identification period January 1, 2011 and June 30, 2016 and treated with oral antipsychotics (aripiprazole, chlorpromazine, clozapine, fluphenazine, haloperidol, loxapine, lurasidone, olanzapine, paliperidone, perphenazine, quetiapine, risperidone, and ziprasidone).
Cohort Selection
We included health plan members between the ages of 18 and 65 who had at least one inpatient claim or two outpatient claims with a relevant diagnosis code for SMI anywhere on the claim and had at least one prescription claim for an oral antipsychotic between January 1, 2011 and June 30, 2016. Patients were stratified into two high risk cohorts based on input from a technical expert panel: those who were recently discharged from a psychiatric-related hospitalization and those with a new diagnosis of SMI who were considered as early episode. These cohorts were identified by the expert panel to be among those with the greatest unmet needs in the SMI population, including higher risk of being nonadherent to prescribed antipsychotic medications and/or to suffer relapse. SMI patients not meeting the cohort criteria (not newly diagnosed and not hospitalized during the study period) were excluded from the analysis. Patients also must have been enrolled in their health plan with both medical and pharmacy benefits for at least 180 days prior to and 360 days following index event. The inclusion criteria for the two cohorts were:
- Recently Discharged Patients: Patients with at least one hospitalization with an SMI diagnosis anywhere on the claim during the reporting period. For patients with more than one SMI-related hospitalization, the first admission event was regarded as the index admission.
- Early Episode Patients: Patients with at least 6 months of pre-index enrollment and no evidence of prescription antipsychotic use or SMI diagnosis prior to the index event, which was defined as the first prescription fill for an antipsychotic medication or first observed claim with a qualifying SME diagnosis code.
Study Outcomes
Study outcomes included: 1) Healthcare Utilization: All-cause and psychiatric-related (defined as claims with diagnosis for SMI in primary or secondary diagnosis field) for: hospital admissions (for early episode patients) and readmissions (for recently discharged patients); emergency department (ED) visits (defined as a visit to hospital emergency room coded with an ED revenue code or procedure code that did not result in admission), and primary care provider (PCP) visits (defined as an office visit coded with an outpatient revenue code or procedure code to physician designated as a PCP); 2) Antipsychotic Medication Adherence: after isolating all the individual antipsychotic drug claims and calculating proportion of days covered for each antipsychotic therapy, patients with at least one episode where proportion of days covered (PDC) ≥ 0.80 were considered adherent; 3) Antipsychotic Medication Switching: a change in medication from one antipsychotic drug to another treatment within a given year; and 4) Total Healthcare Costs: Expenditures were calculated for each patient on a per member per month basis and annualized. Healthcare costs were calculated by applying standardized Medicare allowed payment amounts to each type of service based on published Medicare rates. Standardized pricing was also applied at the NDC level for each pharmacy claim using a standard discount from the Average Wholesale Price (i.e., 15% for brand name drugs and 65% for generic drugs) for each year in the study. This approach accounts for differences in health plan pricing across payer types, geographic areas, health plan negotiated agreements and provider contracts, and thus allows apples-to-apples comparisons of spending across different insurance types and regions.
We used the Charlson Comorbidity Index (CCI) score to evaluate the severity of illness in SMI patients.27 The CCI classifies 17 comorbid conditions using ICD-9-CM/ICD-10-CM codes to provide a weighted score of disease severity that accounts for both the number and severity level of comorbid conditions as they relate to risk of mortality, with a higher score indicating higher burden of illness.
Descriptive analyses were performed to evaluate and compare the characteristics and outcomes of SMI patients in the two study cohorts. We developed a series of regression models to analyze the relationship between patient characteristics and healthcare utilization. After adjusting for patient characteristics such as demographic factors (age and gender), geographic residence areas (Census region), and payer types (commercial plan, Medicare Advantage, or managed Medicaid), generalized linear models with various functional forms and family distributions were performed. For binary outcomes (whether patients had ED visits, PCP visits, observation stays, readmissions or hospitalizations), logistic regressions were used while negative binomial regressions were used for count outcomes (number of ED visits, PCP visits, observation stays, readmissions or inpatient admissions). For cost outcomes, generalized linear models with log link function and gamma distribution were used to account for right-skewed data with a mass of zero.
Results
A total of 51,705 patients met the study eligibility criteria and were included in the analysis (Table 1). The early episode group included 40,655 patients (78.6%) and the recently discharged group 11,050 patients (21.4%). Approximately half of the patients were over age 46 and more than 60% were women. Early episode patients were on average younger.28–30 Recently discharged patients were more likely to be enrolled in a Managed Medicaid plan while early episode patients were more likely to be enrolled in a commercial insurance plan. Recently discharged patients had significantly higher CCI scores compared to early episode patients, especially Medicare patients (2.31 versus 1.33 respectively). Commercially insured SMI patients had the lowest CCI scores.
 |
Table 1 Baseline Patient Characteristics of SMI Patients by Cohort |
The most common SMI diagnosis was bipolar disorder in both cohorts, but early episode patients were frequently diagnosed with multiple psychiatric conditions. Among patients in the recently discharged cohort, 51.9% were diagnosed with bipolar disorder, 27.8% with MDD, and 25.6% with schizophrenia. The early episode cohort had a much higher proportion of patients with MDD (47.0%), more with bipolar disorder (63.4%), and slightly fewer with schizophrenia (22.2%).
Antipsychotic Medication Adherence and Switching
While overall adherence was low, patients in the recently discharged cohort were significantly more likely to be adherent to their medications compared with early episode patients with slightly more than half of recently discharged patients and less than one-fifth of early episode patients exhibiting adherence (16.1%) meeting the criteria of 80% or more proportion days covered within the first 180 days after index prescription. (Figure 1). Adherence was higher within the first 180 days than at 365 days after prescribing antipsychotic treatment and varied by individual antipsychotic drug (Table 2). Quetiapine was most often used in both cohorts, with annual adherence rate of 42% in the recently discharged cohort but less than 1% in the early episode group. Annual adherence rates ranged from 20% to 68% in the recently discharged cohort but 0% to 21.6% in the early episode group.
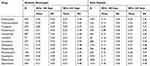 |
Table 2 Adherence to Individual Antipsychotic Medications (PDC≥0.80) |
 |
Figure 1 Adherence to antipsychotic medications. |
In addition to adherence, we examined the rate of medication switching. We found that 100% of early episode patients switched medications during the year (Figure 2), but the majority switched only 1 time (86%). In contrast, just over half of recently discharged patients switched medications during the year, but a larger percentage switched 2 or more times during the year (19% versus 14% of early episode patients).
 |
Figure 2 Number of medication switches per year. |
Utilization of Services
Table 3 presents mean all-cause and mean psychiatric-related utilization of healthcare services, including PCP visits, ED visits, and inpatient admissions/readmissions for the 12-month period following the index date. Events with a psychiatric diagnosis anywhere on the claim were considered psychiatric-related. Recently discharged patients used more healthcare resources across the board, and they also had a larger proportion of psychiatric-related utilization events compared to early episode patients. Psychiatric-related events comprised nearly 40% of PCP visits, 25% of ED visits, and 60% of inpatient readmissions in the recently discharged cohort compared to 28% of PCP visits, 18% of ED visits, and 50% of hospital admissions in the early episode group.
 |
Table 3 Mean All-Cause and Psychiatric Healthcare Resource Utilization |
Healthcare Costs
Both cohorts incurred high levels of annual healthcare costs (Figure 3), with US$21,171 total mean annual cost per patient in the recently discharged cohort and US$15,398 in the early episode cohort. This reflects the higher rate of healthcare utilization shown in Table 3 and reflects higher spending on physician services and tests, outpatient services, ED visits, and inpatient stays. The exception was lower drug costs in the recently discharged cohort compared with the early episode cohort.
 |
Figure 3 Mean annual healthcare costs (US$). |
Regression Results
While patients with SMI have low rates of adherence to antipsychotic medications and high rates of healthcare utilization, we conducted a series of regression analyses to further characterize which patients are most likely to be at risk for specific events (Table 4) to better identify characteristics of SMI patients with greatest unmet needs.
 |
Table 4 Regression Model Results |
Women were more likely to visit their PCP in both groups (OR 1.56 and 1.64 in recently discharged and early episode cohorts respectively), but younger patients were significantly less likely to make a PCP visit (OR 0.58 and 0.63). Women also had a significantly higher likelihood of an ED visit (OR 1.17 and 1.31) and observation stay (OR 1.12 and 1.24), but less likely to have a readmission (OR 0.87 recently discharged) or inpatient stay (OR 0.94 early episode).
In both groups, the youngest subset of patients age 18–25 were most likely to have an ED visit (OR 1.45 and 1.39 respectively) and least likely to have an observation stay (OR 0.56 and 0.54) compared to patients age 46–65. The youngest cohort in both groups were also less likely to have a readmission (recently discharged) or admission (early episode).
We also observed differences in the likelihood of hospitalization by insurance type. Commercially insured patients in the recently discharged cohort were less likely to be readmitted than those in Medicare Advantage plans. In contrast, early episode patients with commercial or Medicaid insurance were more likely to be admitted to the hospital compared to patients insured by Medicare.
Discussion
Serious mental illness is a significant health issue in the United States. However, the populations affected by SMI are quite heterogeneous, with different characteristics, healthcare needs, and burdens of illness related to severity of the disease and existence of multiple comorbidities. This study aimed to determine the patient characteristics associated with antipsychotic medication adherence, healthcare utilization, and cost in patients with SMI. In this national sample of commercially insured, managed Medicare, and managed Medicaid beneficiaries, adherence to antipsychotic medications was low across the board, mirroring previous findings that patients with SMI face unique challenges related to medication adherence.11–14
The SMI population was more likely to be female in both cohorts examined (recently discharged and early episode). Females were found to be significantly more likely to have an ED visit, PCP visit, and observation stay in both cohorts, but less likely to be hospitalized than males. Further investigation is needed to better understand the differences in utilization of healthcare services between males and females.
We found that SMI patients with a recent hospital discharge, who are generally older and sicker, are most often covered by Medicaid, underscoring the fact that these patients face socioeconomic challenges that put them at greater risk for worse outcomes. In addition, since our sample included only patients under age 65, any individuals covered by Medicare could not have “aged in” to the program and thus qualified for Medicare because they were disabled or had end-stage renal disease. This is confirmed by the higher CCI scores observed in the Medicare population in both cohorts compared with patients insured through other means, reflecting the significant burden that longer-term SMI may have on overall health. This is reflected in the significantly higher utilization of healthcare services and higher annual costs for recently discharged patients compared to early episode.
Medicare patients in the recently discharged cohort were more likely to experience a readmission, reflecting their higher burden of disease shown by the high CCI scores and disabled status. There may be an opportunity for Medicare Advantage plans to more aggressively monitor and manage SMI patients following a hospitalization and provide additional non-medical benefits now allowed under the program to reduce the likelihood of readmission.
In contrast, Medicare patients in the early episode cohort were less likely to be admitted to the hospital compared to those in Commercial or Medicaid plans. This may support the notion that although Medicare beneficiaries are older and sicker in general, the capitated payment structure of Medicare Advantage incentivizes plans to avoid unnecessary utilization of high-cost healthcare services through preventive measures and better care coordination. Coordinated management of SMI patients may result in fewer hospitalizations in newly diagnosed patients, but further investigation is needed to evaluate the factors related to fewer hospital admissions in Medicare.
Early episode patients were slightly younger and across the board we observed that younger patients were less likely to have a PCP visit or inpatient stay, they were much more likely to have an ED visit. All early episode patients switched medications during the year, reflecting the fact that these patients may be working with their clinician to find a therapeutic regimen that is most effective for their unique needs and circumstances.
In contrast, about half of the recently discharged cohort switched medications during the year and had lower drug costs. This is somewhat surprising considering the recently discharged have a higher rate of antipsychotic medication adherence. This could be attributed to several things. Compared with early episode patients, recently discharged patients were more likely to switch 2 or more times, which may result in higher drug costs. In addition, a higher portion of recently discharged patients were covered by Medicaid and may receive subsidized drug coverage not reflected in these claims.
These findings accentuate the impact of low adherence to psychiatric treatments on healthcare utilization among different cohorts of SMI patients. By understanding care patterns and health behaviors of heterogeneous cohorts of SMI patients, providers can customize treatment protocols to address adherence to prescribed antipsychotic medications and health outcomes, promote PCP visits and care management, and potentially impact costs.
Limitations
While our study was unique in that it used a large and comprehensive sample of patients, there were several limitations. While MORE2 is a national registry a large proportion of patients in the study population were covered by managed care plans. Results may vary if a larger population of commercial patients or traditional Fee-For-Service Medicare patients were included. Additionally, prior research indicates that patients with SMI are uninsured at higher rates than patients without SMI, and our study does not provide visibility into healthcare utilization patterns of the uninsured SMI population.31 Retrospective claims analysis are also, by nature, limited; for example, PDC is an imperfect measure of adherence since it tracks prescriptions filled and not actual consumption of the medication. The study cohorts were identified using diagnoses recorded on medical claims where coding errors and/or insufficient documentation may occur and could lead to misclassification of patients. Additionally, while we had a 180-day look-back period to identify early episode patients, it is possible these patients had a previous hospitalization or claim for psychiatric treatment prior to our look-back window.
Despite these limitations, the findings underscore the significant heterogeneity in patients with SMI and varying utilization of healthcare services within the population. This analysis provides new insights into which patients are at greater risk for ED visits and hospitalizations, which can help clinicians better manage individual patients with SMI.
Conclusion
Efforts to manage SMI are confounded by the wide heterogeneity and low adherence to treatment observed within the patient population. By better understanding which patients are at higher risk for nonadherence, ED visits, and inpatient hospitalizations, and which patients are less likely to visit their PCP, clinicians can begin to individualize and target care, benefits, and interventions more appropriately to help reduce the significant burden of mental illness.
Highlights
What Is Already Known About This Subject
Although there are numerous evidence-based interventions for serious mental illness (SMI), adherence to recommended antipsychotic medications is a significant problem.
Nonadherence is associated with poor outcomes, including psychiatric hospitalizations and emergency room visits, relapse, and negative social outcomes resulting in additional related costs of up to US$20,000 per patient annually.
What This Study Adds
Our study used comprehensive medical and pharmacy claims data for a national sample of patients diagnosed with SMI to evaluate differences in treatment adherence, healthcare utilization, and costs within two high risk cohorts of patients at different stages of the disease.
Efforts to manage SMI are confounded by heterogeneity and low adherence to treatment. By better understanding which patients are at higher risk for specific adverse outcomes, clinicians can target individual patient interventions more appropriately to reduce the significant burden of SMI.
Acknowledgments
The authors acknowledge that this research study was conducted together with Avalere Health. Avalere maintained full control of manuscript content.
Disclosure
Felicia Forma is an employee of Otsuka Pharmaceutical Development & Commerialization, Inc. The authors report no other conflicts of interest in this work.
References
1. National Institute of Mental Health. NIMH » Mental Illness. Mental illness statistics. Available from: https://www.nimh.nih.gov/health/statistics/mental-illness.shtml.
2. Ahrnsbrak R, Bose J, Hedden SL, Lipari RN, Park-Lee E. Key Substance Use and Mental Health Indicators in the United States: Results from the 2016 National Survey on Drug Use and Health. Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration; 2017.
3. Gogtay N, Vyas NS, Testa R, Wood SJ, Pantelis C. Age of onset of schizophrenia: perspectives from structural neuroimaging studies. Schizophr Bull. 2011;37:504–513. doi:10.1093/schbul/sbr030
4. Häfner H, Maurer K, Löffler W, et al. The epidemiology of early schizophrenia: influence of age and gender on onset and early course. Br J Psychiatry Suppl. 1994;23:29–38. doi:10.1192/S0007125000292714
5. Insel TR. Assessing the economic costs of serious mental illness. Am J Psychiatry. 2008;165:663–665. doi:10.1176/appi.ajp.2008.08030366
6. Trautmann S, Rehm J, Wittchen H. The economic costs of mental disorders. EMBO Rep. 2016;17:1245–1249. doi:10.15252/embr.201642951
7. O’Connor E, Rossom RC, Henninger M, Groom HC, Burda BU. Primary care screening for and treatment of depression in pregnant and postpartum women: evidence report and systematic review for the U.S. Preventive Services Task Force. JAMA. 2016;315:388–406. doi:10.1001/jama.2015.18948
8. Agency for Healthcare Research and Quality. Interventions for Adult Offenders with Serious Mental Illness; 2013.
9. World Health Organization. Pharmacological Treatment of Mental Disorders in Primary Health Care; 2009.
10. Baldwin DS, Anderson IM, Nutt DJ, et al. Evidence-based pharmacological treatment of anxiety disorders, post-traumatic stress disorder, and obsessive-compulsive disorder: A revision of the 2005 guidelines from the British Association for Psychopharmacology. J Psychopharmacol. 2014;28:403–439.
11. Sajatovic M, Valenstein M, Blow FC, Ganoczy D, Ignacio RV. Treatment adherence with antipsychotic medications in bipolar disorder. Bipolar Disord. 2006;8:232–241. doi:10.1111/bdi.2006.8.issue-3
12. Velligan DI, Sajatovic M, Hatch A, Kramata P, Docherty JP. Why do psychiatric patients stop antipsychotic medication? A systematic review of reasons for nonadherence to medication in patients with serious mental illness. Patient Prefer Adherence. 2017;11:449–468. doi:10.2147/PPA.S124658
13. Lacro JP, Dunn LB, Dolder CR, Leckband SG, Jeste DV. Prevalence of and risk factors for medication nonadherence in patients with schizophrenia: A comprehensive review of recent literature. J Clin Psychiatry. 2002;63:892–909. doi:10.4088/JCP.v63n1007
14. Shafrin J, Forma F, Scherer E, Hatch A, Vytlacil E, Lakdawalla D. The cost of adherence mismeasurement in serious mental illness: a claims-based analysis. Am J Manag Care. 2017;23(5):e156–e163.
15. Luciano A, Meara E. The employment status of people with mental illness: national survey data from 2009 and 2010. Psychiatr Serv Wash DC. 2014;65:1201–1209. doi:10.1176/appi.ps.201300335
16. Rosenheck R, Leslie D, Keefe R, et al. Barriers to employment for people with schizophrenia. Am J Psychiatry. 2006;163:411–417. doi:10.1176/appi.ajp.163.3.411
17. Hor K, Taylor M. Suicide and schizophrenia: a systematic review of rates and risk factors. J Psychopharmacol Oxf Engl. 2010;24:81–90. doi:10.1177/1359786810385490
18. Jamison KR. Suicide and bipolar disorder. J Clin Psychiatry Suppl. 2000;61(9):47–51.
19. Cutler RL, Fernandez-Llimos F, Frommer M, Benrimoj C, Garcia-Cardenas V. Economic impact of medication non-adherence by disease groups: a systematic review. BMJ Open. 2018;8:e016982. doi:10.1136/bmjopen-2017-016982
20. Vergouwen ACM, Bakker A, Katon WJ, Verheij TJ, Koerselman F. Improving adherence to antidepressants: a systematic review of interventions. J Clin Psychiatry. 2003;64:1415–1420. doi:10.4088/JCP.v64n1203
21. Scott J, Pope M. Nonadherence with mood stabilizers: prevalence and predictors. J Clin Psychiatry. 2002;63:384–390. doi:10.4088/JCP.v63n0502
22. Chakrabarti S. Treatment-adherence in bipolar disorder: a patient-centred approach. World J Psychiatry. 2016;6:399–409. doi:10.5498/wjp.v6.i4.399
23. Ascher-Svanum H, Zhu B, Faries D, Lacro JP, Dolder CR. A prospective study of risk factors for nonadherence with antipsychotic medication in the treatment of schizophrenia. J Clin Psychiatry. 2006;67:1114–1123. doi:10.4088/JCP.v67n0715
24. Chapman SCE, Horne R. Medication nonadherence and psychiatry.Curr Opin Psychiatry. 2013;26:446–452. doi:10.1097/YCO.0b013e3283642da4
25. MacEwan J, Forma F, Shafrin J, Hatch A, Lakdawalla D, Lindenmayer JP. Patterns of adherence to oral atypical antipsychotics among patients diagnosed with schizophrenia. J Manag Care Spec Pharm. 2016;22(11):1349–1361. doi:10.18553/jmcp.2016.22.11.1349
26. Periodic Review Status for Inovalon’s Medical Outcomes Research for Effectiveness and Economics Registry (MORE2 Registry®), Letter of Determination, Daniel C. Barth-Jones, M.P.H., Ph.D., President, dEpid/dt Consulting, Inc. and Assistant Professor of Clinical Epidemiology, Mailman School of Public Health, Columbia University, October 27, 2017.
27. Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45(6):613–619. doi:10.1016/0895-4356(92)90133-8
28. Kessler RC, Amminger GP, Aguilar-Gaxiola S, et al. Age of onset of mental disorders: a review of recent literature. Curr Opin Psychiatry. 2007;20:359–364. doi:10.1097/YCO.0b013e32816ebc8c
29. National Alliance on Mental Illness. Bipolar disorder. Available from: https://www.nami.org/Learn-More/Mental-Health-Conditions/Bipolar-Disorder.
30. American Psychiatric Association. Warning signs of mental illness. Available from: https://www.psychiatry.org/patients-families/warning-signs-of-mental-illness. Accessed July 5, 2018.
31. Walker ER, Cummings JR, Hockenberry JM, Druss BG. Insurance status, use of mental health services, and unmet need for mental health care in the United States. Psychiatr Serv Wash DC. 2015;66:578–584. doi:10.1176/appi.ps.201400248
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
