Back to Journals » Patient Preference and Adherence » Volume 11
Text messaging to decrease tuberculosis treatment attrition in TB-HIV coinfection in Uganda
Authors Hermans SM , Elbireer S, Tibakabikoba H, Hoefman BJ, Manabe YC
Received 24 February 2017
Accepted for publication 24 June 2017
Published 31 August 2017 Volume 2017:11 Pages 1479—1487
DOI https://doi.org/10.2147/PPA.S135540
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Sabine M Hermans,1–4 Sawsan Elbireer,5 Harriet Tibakabikoba,1 Bas J Hoefman,6 Yukari C Manabe1,2,7
1Department of Research, Infectious Diseases Institute, Makerere University College of Health Sciences, Kampala, Uganda; 2Department of Internal Medicine, School of Medicine, Makerere University College of Health Sciences, Kampala, Uganda; 3Department of Global Health, Academic Medical Center, University of Amsterdam, Amsterdam Institute for Global Health and Development, the Netherlands; 4Department of Internal Medicine and Infectious Diseases, University Medical Centre Utrecht, Utrecht, the Netherlands; 5Makerere University–Johns Hopkins University Research Collaboration, Kampala, Uganda; 6TTC Mobile, Kampala, Uganda; 7Division of Infectious Diseases, Department of Medicine, Johns Hopkins University School of Medicine, Baltimore, MD, USA
Background: Low tuberculosis (TB) treatment completion rates in sub-Saharan Africa are an important driver of multidrug resistance. Mobile technology-based interventions have been shown to improve adherence to antiretroviral therapy in sub-Saharan Africa. We aimed to test the effect of a short-message service (SMS) intervention on loss to follow-up (LFU).
Materials and methods: In this quasi-experimental study, all adult, literate, HIV-infected patients with mobile phone access diagnosed with TB between November 2010 and October 2011 in an urban clinic in Uganda were eligible to receive adherence and appointment reminders and educational quizzes during the first 8 weeks of TB treatment. Their risk of LFU in the first 8 weeks of treatment was compared with that of patients starting treatment between March 2009 and August 2010 using logistic regression.
Results: One of 183 (0.5%) enrolled patients was lost to FU during the intervention compared to six of 302 (2.0%) in the preintervention control group (RR 0.27, 95% CI 0.03–2.07; P=0.22). The SMS intervention was rated as very helpful by 96%. Barriers identified included interrupted phone access (26%, median 14 days) and difficulties responding by SMS. The response rate to educational quizzes was below 10%. There were no unintentional disclosures of TB or HIV status due to the intervention.
Conclusion: An SMS reminder service did not show a clear effect on short-term risk of LFU in this study, which was underpowered due to a lower baseline risk in the control group than expected. The SMS-reminder service was rated highly, and there were no breaches of confidentiality. Important technological barriers have implications for larger-scale implementation, not only for TB but also other disease modalities.
Keywords: mHealth, mobile technology, short message service, text messaging, e-health, cellular phone, telemedicine, tuberculosis, adherence, Uganda, Africa
Background
Incomplete treatment of tuberculosis (TB) poses a serious risk to the individual, as well as the community. Treatment loss to follow-up (LFU) leads to treatment failure and relapse, prolonged infectiousness, and development of drug resistance that requires prolonged and expensive therapy that is less likely to be successful.1,2 Health service factors, including lack of communication with health care providers, are important risk factors for TB-treatment LFU.3 There is a clear need to develop and test affordable, innovative strategies and tools to provide adherence support.
Mobile technology-based support systems are attractive in sub-Saharan Africa (SSA), because of the high mobile phone penetration and network coverage that has occurred in the last decade. In 2015, 76% of the continent’s population was estimated to have a mobile telephone subscription compared to 12% in 2005.4 There is evidence that mobile technology-based interventions are effective in improving healthy behavior or aiding disease management (such as medication adherence).5 Although data from SSA are limited, there is good evidence to support 20%−60% higher adherence to antiretroviral therapy (ART) with text messaging interventions.6
The potential of mobile-phone technology to aid TB control has been recognized by the Stop TB Partnership.7 A number of pilot projects and studies have been undertaken in this area, but with limited impact evaluations.8 A systematic review on this topic found a paucity of well-designed studies that were published in peer-reviewed literature.9 Recently, two randomized controlled studies in China and Pakistan found no impact of daily reminders on TB adherence.10,11
Uganda is one of the countries with a high burden of TB and HIV coinfection.12 It also has one of the highest proportions of TB patients lost to follow-up in SSA (12% in 2014).12 As multidrug-resistance rates are still relatively low,13 an intervention to decrease TB treatment LFU could help avert a multidrug-resistant TB epidemic. Uganda has a mobile phone network coverage of over 95%, and 50% of inhabitants have a mobile phone subscription.14,15 We implemented a mobile phone text message reminder service in an integrated TB-HIV clinic with a high documented LFU rate in Kampala, Uganda.16 This study aimed to test the effect of this service on 8-week TB treatment LFU in individuals coinfected with HIV.
Materials and methods
Study setting
The Infectious Diseases Institute (IDI) in Kampala, Uganda and its integrated TB-HIV clinic have been described in detail previously.16,17 In brief, the IDI provides adult outpatient care to over 30,000 registered HIV patients. At the time of the study, more than 13,000 patients were in active FU, of which over 8,000 had initiated ART. The clinicians followed the guidelines of the National TB and Leprosy Programme (NTLP) for diagnosis and treatment of TB.18 Available diagnostics included sputum fluorescence microscopy and fine needle aspirates of lymph nodes, chest radiology, and abdominal ultrasonography. No routine mycobacterial culture facilities were available. Diagnosis was made on the basis of these investigations, but very often on clinical judgment alone. Treatment for new TB cases consisted of 2 months of isoniazid, rifampicin, ethambutol, and pyrazinamide, followed by 6 months of isoniazid and ethambutol. Directly observed treatment (DOT) was not practiced, although community-based DOT with treatment buddies was advocated. As part of routine care, all TB patients received a one-on-one counseling session by the dedicated TB-HIV nurse–counselor before treatment initiation. This counselor also performed tracing of LFU patients by phone tracing and home visits on an approximate 2 weekly basis. TB care took place in an outdoor integrated HIV and TB clinic, offering care for both diseases simultaneously and by the same staff.16
At the time of conception of the study (2008), 17% of TB patients became lost to FU within the first 8 weeks of TB treatment.16 Risk factors for LFU were investigated by a case-control study: lack of essential information about TB and its treatment was found to be a strong predictive factor.19
Study design
We designed a quasi-experimental study with a historical control group to investigate the effect of short message service (SMS) text message reminders at the integrated TB-HIV clinic of the IDI for all patients initiating TB treatment. The intervention period was November 1, 2010 to October 31, 2011. The preintervention control period was March 1, 2009 to August 31, 2010; this period was predetermined to allow for an equal number of participants in the intervention group, as estimated by the sample size calculation. The 2 month gap was to allow for completion of 2 months of treatment by the historical control group before implementation of the reminder service, to avoid spillover (changed study outcome among controls by discussions about the intervention, eg, in the waiting area). No additional interventions to improve TB care were instituted during either period. A reminder text service duration of 8 weeks was chosen to coincide with the early treatment period, during which patients were most prone to LFU in our clinic.16 FU duration was 8 months after enrolment.
Sample-size calculation
With an estimated 50% decrease in LFU from 17% to 8.5%, we estimated our sample size with 80% power and 95% level of significance at 291 participants per group. With an approximate equal number of preintervention controls, the total estimated sample size was 582 patients.
Ethical approval
The study was approved by the Scientific Review Committee of the IDI (May 27, 2010) and the institutional review boards of Makerere University College of Medicine (August 24, 2010), Johns Hopkins University School of Medicine (October 21, 2010), and the Uganda National Council for Science and Technology (September 9, 2010). The study was conducted in accordance with the Declaration of Helsinki. All intervention group participants signed a written informed consent form. The control group participants gave written informed consent for use of their routinely collected data for research purposes at enrolment in the clinic, as is standard for all IDI patients. The study was registered at the Pan African Clinical Trials Registry (PACTR201310000671259). This took place retrospectively following eligibility confirmation (nonrandom assignment of the intervention and use of a historical control group). This study is in accordance with the Transparent Reporting of Evaluations with Nonrandomized Designs (TREND) statement.20 The study protocol and the completed TREND checklist is available upon request from the corresponding author.
Study population
For our intervention group, we consecutively recruited all adult (≥18 years) HIV-positive men and women diagnosed with active TB at the IDI TB-HIV clinic or at Mulago Hospital and willing to receive FU care at the IDI who had either not yet started treatment or for whom TB treatment initiation had occurred within the 2 weeks prior to enrolment. Participants had to have daily access to a mobile phone and to have demonstrated ability to operate a mobile and communicate using text messaging. Shared phone access was allowed if access was daily, if participants had disclosed or were willing to disclose their TB status to the phone owner and/or any other users of the phone, and if the phone owner agreed to participate. Literacy was assessed at screening using a tool previously used for a randomized controlled trial in our clinic;21 we estimated that 86% of patients would be literate. Illiterate patients who had disclosed or who were willing to disclose their TB status to a literate and willing treatment buddy were eligible to receive the services.
The preintervention control group consisted of all patients diagnosed with TB and started on TB treatment in the IDI TB-HIV clinic during the specified period. To maximize comparability with participants receiving the SMS services, patients without a mobile phone number recorded at treatment initiation (which is routine practice) were excluded. Literacy data were unavailable for these preintervention control patients.
Intervention
The implemented SMS-reminder service consisted of three different types of text messages: adherence reminders (on days 2, 7, and 11 after the most recent appointment), reminders of upcoming appointments (once every 2 weeks, sent the day before the appointment), and educational quizzes (on days 3, 6, 9, and 12 after the most recent appointment). The latter were interactive: a multiple choice question was sent to the participant, to which they could reply free of charge.22 A computer-generated response was sent in reply, including the correct answer with some additional information. The intervention also included a toll-free callback service for support with any queries participants might have. This phone number was included in all text messages sent. The AIDS Treatment Information Centre, based at the IDI, received these phone calls and connected the study participants with the study nurse based at the TB-HIV clinic. The intervention coincided with the intensive phase of TB treatment, during which all TB patients visited the TB clinic every 14 days. The adherence reminder and educational messages were sent in a cycle of 8 weeks, ensuring no duplication. Samples of the different types of text messages are included in the Supplementary material.
Study outcomes and definitions
The primary outcome measure was the risk of LFU in the first 2 months of TB treatment, defined as a failure to collect TB treatment for 2 or more consecutive weeks. Secondary study outcomes included 1) TB treatment outcomes at the end of TB treatment, defined by the World Health Organization guidelines: cure (smear-positive patients who were smear-negative in the last month of treatment), completion, treatment LFU (interrupted treatment for more than 2 months), failure (smear-positive after 5 months of treatment), and transfer out;23 2) average self-reported TB drug adherence, expressed in percentages of pills taken; 3) average self-reported ART adherence, expressed in percentages of pills taken; and 4) patients’ satisfaction and knowledge on TB-HIV issues, based on pre- and postintervention questionnaire assessment. The evaluation of the toll-free callback service will be reported separately (manuscript in preparation). The latter three outcomes were available only for the intervention group. As a larger proportion than anticipated were excluded from the intervention, we also investigated the difference in baseline characteristics and treatment outcomes (both at 8 weeks and at the end of TB treatment) between the intervention group and the group of patients who were screened but not enrolled. There was no blinding of study outcome ascertainment.
Data collection
Data on intervention group participant characteristics, risk factors for LFU, and knowledge of TB and HIV care were collected at the time of enrolment and at the end of the intervention (at 8 weeks). In addition, feedback on the study interventions and TB and HIV care was collected at 8 weeks. Intervention group participants who became lost to FU from treatment according to the protocol’s definition were contacted by the study nurse to identify the underlying reason. Information on phone calls from participants received by the study nurse was recorded in a separate questionnaire. The study nurse collected the primary study outcome for all study participants. For those in the control group, these were determined by reviewing the TB register, which captures visit dates for all TB patients. For all study participants, routine clinical data at each visit were captured in a Microsoft SQL database (HIV data) and a Microsoft Access database (TB data). Data on study participants and preintervention controls were extracted from these databases through linking of the patient’s clinic identification number. The database of the implementing mobile-phone partner, Text to Change (Kampala, Uganda), captured data on all sent and received text messages as part of the intervention.
Statistical methods
Baseline characteristics were summarized using proportions for categorical variables and means (with standard deviations) or medians (with interquartile ranges) for normally and abnormally distributed numerical variables, respectively. Treatment outcomes across groups were assessed using proportions and compared using χ2 or Fisher’s exact test to account for low expected numbers. RRs of TB treatment LFU during the first 8 weeks of treatment and at the end of treatment in the intervention group compared to the control group were calculated. Multivariable analysis was not performed, because of the risk of overfitting due to the small number of events. Other secondary study outcomes were analyzed using summary statistics alone. All analyses were conducted as “modified intention to treat” (excluding patients who died, were transferred out, or stopped treatment on doctor’s orders during the intervention period of the study) and using Stata version SE 11.2 (StataCorp, College Station, TX, US).
Results
A total of 354 consecutive patients initiating TB treatment were assessed for eligibility to participate in the intervention group. Of these, 183 were enrolled in the study and 171 were excluded on the basis of the predefined eligibility criteria (Figure 1). We did not complete enrolment, due to funding restrictions and the results of an interim analysis performed in September 2011 prompted by lagging patient enrolment (see Supplementary material). Twelve participants did not complete the study exit visit as they became lost to FU (n=1), died (n=9), or had been transferred out (n=2). These patients did not contribute toward the qualitative study outcomes. Baseline characteristics of the participants included are summarized in Table 1. The control group had a higher proportion of extrapulmonary TB and retreatment diagnoses. The characteristics of the excluded participants did not differ from those that were included (see Supplementary material).
TB-treatment outcomes and risk of LFU
Treatment outcomes at the end of the study period and at the end of treatment were similar between the two groups (Table 2). There was no statistical evidence for a difference in the risk of LFU during the first 8 weeks in the intervention group compared to the preintervention control group (one of 183 compared to six of 302, RR 0.27, 95% CI 0.03−2.07; P=0.22). The group of patients who initiated TB treatment during the same period but who were not enrolled in the study had no different risk of LFU at 8 weeks compared to the preintervention control group (RR 0.31, 95% CI 0.04−2.37; P=0.27). The mean self-reported adherence to TB treatment among the intervention group participants who completed the study exit visit was 98% (SD 7.2%), and their self-reported adherence to ART was 99% (SD 7.5%).
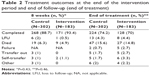  | Table 2 Treatment outcomes at the end of the intervention period and end of follow-up (end of treatment) |
Knowledge on TB-HIV issues
At enrolment, intervention group participants answered an average of six of eight questions on TB-HIV knowledge correctly (n=171, SD 1); 90% (n=155) had been counseled by the dedicated TB-HIV counselor at TB treatment initiation, the majority of which had taken between 30 and 60 minutes. At completion of the study, the average of correct answers increased to seven of the same eight questions (SD 0.7). The median increase in correct answers between study entry and exit was 1 (IQR 0−1).
Participant satisfaction with SMS-reminder service
No participant reported adverse consequences as a result of other phone users reading their messages, although 46 (85%) thought the other users objected to them. None of the study participants (sharing or not sharing their phone) were forced to disclose their TB or HIV diagnosis because of the intervention.
A total of 165 (96%) participants rated the text messages as helpful or very helpful, and none as not helpful. The majority (84%) found the message frequency just right, 7% not frequent enough, and 4% too frequent. Participants rated all the specific types of messages (reminder messages 94%, interactive quizzes 92%, and appointment reminders 94%) as equally helpful. None of the participants found the messages intrusive. A quarter of participants stated they did not always understand the messages, due to the technical language used (28%).
Appointment reminders were generally found to be helpful; one participant noted “Mum would give me [money for] transport without hesitation”, and another “There was no money in the village but when aunt reminded me they gave me [money for] transport”. These messages were found to be useful for logistical issues: “… to remind me [to] pick [up] streptomycin which I forgot in the clinic” and “… helped call the clinic to request for change of appointment while far”; 92% of participants reported that the reminders helped them to remember their appointment and encouraged clinic attendance: “Was encouraged to come to clinic, even during the time of riots”.
Despite rating the messages as helpful, 46% of participants stated they replied to quizzes sometimes (n=79), 29% always (n=49), and 25% (n=43) never. This self-reported participation was higher than the actual participation (estimated at below 10%). Reasons for not replying were varied: the messages and instructions were confusing, the participants were “weak”, had busy schedules, had phone problems (no network or credit, a faulty phone), did not recognize the symptoms in the message, or felt no need to reply. Many commented on the complexity of the messages and their frustration at trying to send a reply that was not recognized by the system. Response rates did not differ by education level. On the whole, participants were keen for more information. Eight of 13 participants who gave additional input suggested the service should be continued up to the end of treatment.
Usage and technological barriers of the SMS reminder service
Of the 171 patients who completed the study exit questionnaire, 155 (91%) reported having received all expected text messages. A total of 45 (26%) reported that they had been unable to use their mobile phone for a median duration of 14 (IQR 5−28) days during the period of the intervention. Reasons included having their phone stolen (18%), no longer having access to the shared phone (24%), not being able to charge the battery (26%), and the phone getting damaged or broken (26%). Of the 46 participants (25%) that shared a phone during the 8 weeks of the SMS reminders, six (13%) did not have daily access to it.
Messages were not delivered to participants when a particular network provider had interrupted service. These interruptions were generally short (a few days), but one particular network provider had an interruption of 6–8 weeks (between September and October 2011, possibly affecting three participants enrolled at that time). To improve stability and performance, the implementing mobile technology partner TTC decided to upgrade their network server in April 2011 (halfway enrolment). As an unforeseen consequence of this, some of the data collected on sent and received text messages before the upgrade became irretrievable. The final database from TTC contained phone numbers of 178 of the 183 participants in the intervention group. However, no data on sent and received messages were recorded for 80 of these 178 (45%) participants. Therefore, we cannot reliably report on exact numbers of texts sent and received. The data that we were able to analyze showed a response rate of 13% (599 responses received to 4,741 quizzes sent). Furthermore, a large proportion of responses were sent in a text format unrecognizable by the server (not in the required format “<question number><space><Answer Nr>”; see Supplementary material).
Discussion
During an SMS reminder service in the first 8 weeks of TB treatment, only one of 183 enrolled participants became lost to FU from TB treatment. The primary outcome did not differ from the control period; however, this was due to unexpectedly low LFU rates in the study population in the control period, likely due to improvement in care resulting from integration of TB and HIV services that occurred after study inception.16 The new “one-stop shop” model of care was implemented in January 2009, and included a dedicated medical officer and counselor responsible for the care of both diseases at the same time. Improved tracing of patients also led to improved outcome ascertainment, and likely accounts for the lower risk of LFU than prior to integration.
Considering the good evidence to suggest increased adherence to HIV treatment in a similar setting,6,24 there has been interest in the potential of mobile-phone services in improving TB treatment adherence and outcomes.8 A cluster-randomized controlled trial in China showed no effectiveness of daily SMS reminders in improving adherence to TB treatment, but LFU was reduced by 58%.10 Another recent randomized trial of daily interactive two-way reminders in Pakistan showed no difference in treatment completion.11 Results of other published studies are encouraging, despite the potential for substantial bias due to suboptimal study designs.8,9 A small randomized controlled trial (n=37) found higher self-reported adherence among Argentinean TB patients receiving biweekly educational text messages and interactive SMS-based reminders compared to those that did not.25 A pilot study in Cape Town found that 221 TB patients who received SMS adherence and appointment reminders had similar outcomes to patients who received standard of care (DOT).26 However, the lack of effect was attributed to poor implementation of the SMS service, due to logistical issues. In northern Thailand, Kunawararak et al compared treatment outcomes of 49 TB patients who received daily reminder phone calls to those who did not.27 Treatment completion was higher in those who received calls than in those who did not (100% versus 59%). An unpublished nonrandomized Kenyan study found increased TB-clinic attendance when sending SMS appointment reminders 1 day in advance,28 and this was confirmed by a systematic review on the effect of reminders on clinic attendance in general.29 Other initiatives have incorporated text messaging with other mobile phone applications, such as interactive voice responses, video-based DOT, and medication dispensers with GSM communication chips.8,30
Despite its lack of power to assess effectiveness, our study gives important insights into the feasibility of implementing mobile-phone services in TB care in SSA. Currently there is a lack of data on this topic, which is essential to inform best implementation practices.8 Participants rated the intervention highly, which confirms data from Peru and China showing positive perceptions of TB patients on the use of SMS to improve adherence.31,32 The acceptance of SMS reminders and quizzes was very high, the messages were highly rated, and there were no breaches of confidentiality. The service increased communication between the clinic and patients, and as such was a good adjunct in a highly functioning TB-HIV clinic where baseline counseling and TB knowledge was good and LFU rates low.
High rates of illiteracy and mobile-phone sharing halved the number of eligible patients. In addition, there were significant technological issues with the automated messaging service (problems with scheduled messages, undelivered messages, participants’ difficulty in responding to quizzes). Almost a quarter of participants reported interruptions in use of their mobile phone for a significant period during the intervention. Despite better treatment outcomes than expected in our study, these difficulties likely limit the potential impact of similar interventions to improve health-care outcomes.
Also, there were very low response rates to the interactive quizzes. Evaluations of SMS quizzes for the purposes of health education among the healthy population in Uganda have also shown low response rates (below 10%), despite additional monetary incentives.22 Among a subgroup of highly active subscribers of one mobile-phone provider in northern Uganda, the response rate to HIV quizzes was 21%.33 The free HIV counseling and testing services offered as a reward were only accessed by one of ten responders. These issues raise questions about using bidirectional text-messaging interventions as the principal communication method between clinics and their patients.
The successful mobile-phone intervention for ART adherence in Kenya used a generic bidirectional weekly text message coupled with FU phone calls if participants did not respond within 48 hours, or if they responded that they were in need of assistance.24 A feeling of “being cared for” was hypothesized as a potential mechanism of action. Simple daily SMS reminders have been shown not to be effective.5 Also, since study inception, it has become clear that a high frequency of messages can lead to message fatigue.6,34 This could explain the lack of effectiveness in the China and Pakistan trials.10,11 Our intervention frequency of four messages a week could thus have limited the potential for effectiveness.
Based on these reports and on our experience, we believe that future mobile technology interventions to improve adherence to TB control in resource-limited settings should be greatly simplified. We implemented the intervention in a highly functioning TB-HIV integrated urban clinic with relatively high staffing and where patient education was very good, as shown by the postcounseling TB-test scores. Mobile-phone interventions may have a greater potential in rural settings, where adjunctive interventions to fill health-workforce gaps may have greater impact. There is a need for large, high-quality randomized controlled trials to explore the optimum frequency and content of text messaging and its effectiveness, and to answer questions about phone coverage in rural areas, phone sharing, and confidentiality. Interventions tailored to the setting could be explored; reminders could be sent to community health workers providing DOT in rural areas instead of to the patients, as successfully piloted in Malawi.35 Comparisons are also needed across different mobile phone applications or modalities to determine the best way to offer treatment support using this technology.
Study limitations included the use of a preintervention control group: temporal changes could have influenced study outcomes, irrespective of the intervention. The mobile phone-access eligibility criteria were not the same between the intervention and control group, which could have led to selection bias. However, the availability of a phone number in the TB register is suggestive of access to a mobile phone (either their own or shared access), and the relative similarity in proportions of patients excluded due to the lack of a mobile phone (access or number in the register) suggests comparability. A quarter of participants felt the language used was too technical, despite our attempts to use simple language; piloting of the questions beforehand would have been beneficial. Due to the nature of the intervention, the study participants, the study nurse and the outcome assessor for the preintervention control group were not blinded to the exposure status of the participant. Tracing of LFU participants was the same in both groups. Lastly, this study was only among TB-HIV coinfected patients, which might impact the generalizability of our results. However, we have no reason to believe that the potential impact of the intervention would be different among HIV-negative TB patients.
Conclusion
An SMS reminder service did not show an effect on short-term risk of TB treatment LFU in this study, which was underpowered due to a lower-than-anticipated participant-recruitment rate and LFU risk in the control group. The SMS reminder service was highly rated, and there were no breaches of confidentiality, though substantial technological barriers have implications for larger scale implementation, not only for TB but also other disease modalities.
Acknowledgments
We are grateful to our study participants and to the IDI TB-HIV clinic for hosting and assisting our study team. We would like to extend our thanks to the AIDS Treatment and Information Centre (Christine Kihembo and Stella Zawedde) and to Text to Change Uganda (Jan-Willem Loggers and Marcus Wagenaar) for their support of this study. We appreciate Andy Hoepelman’s support during the inception of the study and Larry Chang for helpful scientific input.
This study was financially supported by Microsoft Research Limited (contract 2010-040, http://research.microsoft.com) and the KNCV Tuberculosis Foundation (contract U.10.0698, http://www.kncv.nl). Salary support for SH, SO, HT, and BH was provided through these grants. SH also received support from the Infectious Diseases Network for Treatment and Research in Africa (INTERACT) program, funded by the Netherlands Organization for Scientific Research – WOTRO Science for Global Development: NACCAP (grant W07.05.20100) and the European Union (grant SANTE/2006/105-316). SO was supported through NIH funding to the IMPAACT network and Microbicide Trials Network studies. Funding for YM was provided by the National Institutes of Health, DMID under the Tuberculosis Clinical Diagnostics Research Consortium (NIH/NIAID, HHSN272200900050C) and the NIH-funded medical education partnership initiative Medical Education for Services to All Ugandans (MEPI-MESAU). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author contributions
SMH, SE, and YCM conceived and designed the experiments. SMH, SE, HT, and BH were involved in collecting the data. SMH analyzed the data. SMH wrote the first draft of the manuscript. All authors contributed toward interpretation of the data, drafting and critically revising the paper and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
Mitchison DA. How drug resistance emerges as a result of poor compliance during short course chemotherapy for tuberculosis. Int J Tuberc Lung Dis. 1998;2(1):10–15. | ||
Weis SE, Slocum PC, Blais FX, et al. The effect of directly observed therapy on the rates of drug resistance and relapse in tuberculosis. N Engl J Med. 1994;330(17):1179–1184. | ||
Munro SA, Lewin SA, Smith HJ, Engel ME, Fretheim A, Volmink J. Patient adherence to tuberculosis treatment: a systematic review of qualitative research. PLoS Med. 2007;4(7):e238. | ||
International Telecommunication Union. Key global telecom indicators for the world telecommunication service sector. 2016. Available from: http://www.itu.int/en/ITU-D/Statistics/Documents/statistics/2016/ITU_Key_2005-2016_ICT_data.xls. Accessed July 17, 2017. | ||
Free C, Phillips G, Galli L, et al. The effectiveness of mobile-health technology-based health behaviour change or disease management interventions for health care consumers: a systematic review. PLoS Med. 2013;10(1):e1001362. | ||
Finitsis DJ, Pellowski JA, Johnson BT. Text message intervention designs to promote adherence to antiretroviral therapy (ART): a meta-analysis of randomized controlled trials. PLoS One. 2014;9(2):e88166. | ||
mHealth Alliance, Stop TB Partnership. The role of mHealth in the fight against tuberculosis. 2012. Available from: http://www.stoptb.org/assets/documents/getinvolved/psc/mHealth%20&%20TB%20by%20mHA%20&%20STBP%202012.pdf. Accessed April 14, 2013. | ||
Denkinger CM, Grenier J, Stratis AK, Akkihal A, Pant-Pai N, Pai M. Mobile health to improve tuberculosis care and control: a call worth making. Int J Tuberc Lung Dis. 2013;17(6):719–727. | ||
Nglazi MD, Bekker LG, Wood R, Hussey GD, Wiysonge CS. Mobile phone text messaging for promoting adherence to anti-tuberculosis treatment: a systematic review. BMC Infect Dis. 2013;13:566. | ||
Liu X, Lewis JJ, Zhang H, et al. Effectiveness of electronic reminders to improve medication adherence in tuberculosis patients: a cluster-randomised trial. PLoS Med. 2015;12(9):e1001876. | ||
Mohammed S, Glennerster R, Khan AJ. Impact of a daily SMS medication reminder system on tuberculosis treatment outcomes: a randomized controlled trial. PLoS One. 2016;11(11):e0162944. | ||
World Health Organization. Global Tuberculosis Report 2016. Geneva: WHO; 2016. | ||
Lukoye D, Cobelens FGJ, Ezati N, et al. Rates of anti-tuberculosis drug resistance in Kampala-Uganda are low and not associated with HIV infection. PLoS One. 2011;6(1):e16130. | ||
Uganda Communications Commission. UCC message for ATU Day 2014. 2014. Available from: http://www.ucc.co.ug/data/edposts/13/UCC-message-for-ATU-Day-2014.html. Accessed November 24, 2016. | ||
International Telecommunication Union. Mobile-cellular subscriptions 2000–2016 country data. 2016. Available from: http://www.itu.int/en/ITU-D/Statistics/Documents/statistics/2016/Mobile_cellular_2000-2015.xls. Accessed November 24, 2016. | ||
Hermans SM, Castelnuovo B, Katabira C, et al. Integration of HIV and TB services results in improved TB treatment outcomes and earlier prioritized ART initiation in a large urban HIV clinic in Uganda. J Acquir Immune Defic Syndr. 2012;60(2):e29–e35. | ||
Hermans S, van Leth F, Manabe Y, Hoepelman A, Lange J, Kambugu A. Earlier initiation of antiretroviral therapy, increased tuberculosis case finding and reduced mortality in a setting of improved HIV care: a retrospective cohort study. HIV Med. 2012;13(6):337–344. | ||
Uganda Ministry of Health. Manual of the National Tuberculosis and Leprosy Programme. 2nd ed. Kampala: Ministry of Health; 2010. | ||
Elbireer S, Guwatudde D, Mudiope P, Nabbuye-Sekandi J, Manabe YC. Tuberculosis treatment default among HIV-TB co-infected patients in urban Uganda. Trop Med Int Health. 2011;16(8):981–987. | ||
Des Jarlais DC, Lyles C, Crepaz N, Group T. Improving the reporting quality of nonrandomized evaluations of behavioral and public health interventions: the TREND statement. Am J Public Health. 2004;94(3):361–366. | ||
Castelnuovo B, Newell K, Manabe YC, Robertson G. Multi-media educational tool increases knowledge of clinical trials in Uganda. J Clin Res Bioeth. 2014;5:165. | ||
Danis CM, Ellis JB, Kellogg WA, et al. Mobile phones for health education in the developing world: SMS as a user interface. Poster presented at: First ACM Annual Symposium on Computing for Development; December 17–18, 2010; London, UK. | ||
World Health Organization. Treatment of Tuberculosis Guidelines. 4th ed. Geneva: WHO; 2010. | ||
Lester RT, Ritvo P, Mills EJ, et al. Effects of a mobile phone short message service on antiretroviral treatment adherence in Kenya (WelTel Kenya1): a randomised trial. Lancet. 2010;376(9755):1838–1845. | ||
Iribarren S, Beck S, Pearce PF, et al. TextTB: a mixed method pilot study evaluating acceptance, feasibility, and exploring initial efficacy of a text messaging intervention to support TB treatment adherence. Tuberculosis research and treatment. 2013;2013:349394. | ||
Bridges.org. Evaluation of the On Cue compliance service pilot: testing the use of SMS reminders in the treatment of tuberculosis in Cape Town, South Africa. 2005. Available at: http://www.kiwanja.net/database/document/report_tb_compliance.pdf. Accessed January 15, 2009. | ||
Kunawararak P, Pongpanich S, Chantawong S, et al. Tuberculosis treatment with mobile-phone medication reminders in northern Thailand. Southeast Asian J Trop Med Public Health. 2011;42(6):1444–1451. | ||
Owiti P, Gardner A, Szkwarko D, Diero L, Carter E. Mobile phone text messaging reminders to aid adherence to tuberculosis care in Eldoret, Kenya. Int J Tuberc Lung Dis. 2012;16(12 Suppl 1):S200. | ||
Gurol-Urganci I, de Jongh T, Vodopivec-Jamsek V, Atun R, Car J. Mobile phone messaging reminders for attendance at healthcare appointments. Cochrane Database Syst Rev. 2013;(12):CD007458. | ||
Interactive Research and Development. mHealth to Improve TB Care. Karachi: IRD; 2012. | ||
Albino S, Tabb KM, Requena D, et al. Perceptions and acceptability of short message services technology to improve treatment adherence amongst tuberculosis patients in Peru: a focus group study. PLoS One. 2014;9(5):e95770. | ||
Lei X, Liu Q, Wang H, Tang X, Li L, Wang Y. Is the short messaging service feasible to improve adherence to tuberculosis care? A cross-sectional study. Trans R Soc Trop Med Hyg. 2013;107(10):666–668. | ||
Van Beijma H, Hoefman B, Sparks SP. Uganda: mobile phone technology, whose rapid growth in Uganda provides an avenue to reach millions with HIV/AIDS messages in a relatively easy, practical and cost-effective way. 2010. Available from: http://www.itu.int/dms_pub/itu-d/opb/stg/D-STG-SG02.14.2-2010-PDF-E.pdf. Accessed March 28, 2013. | ||
Mbuagbaw L, van der Kop ML, Lester RT, et al. Mobile phone text messages for improving adherence to antiretroviral therapy (ART): an individual patient data meta-analysis of randomised trials. BMJ Open. 2013;3(12):e003950. | ||
Mahmud N, Rodriguez J, Nesbit J. A text message-based intervention to bridge the healthcare communication gap in the rural developing world. Technol Health Care. 2010;18(2):137–144. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


