Back to Journals » Clinical Epidemiology » Volume 7
Oxaliplatin-based first-line chemotherapy is associated with improved overall survival compared to first-line treatment with irinotecan-based chemotherapy in patients with metastatic colorectal cancer – Results from a prospective cohort study
Authors Marschner N, Arnold D, Engel E, Hutzschenreuter U, Rauh J, Freier W, Hartmann H, Frank M, Jänicke M
Received 6 September 2014
Accepted for publication 6 December 2014
Published 20 April 2015 Volume 2015:7 Pages 295—303
DOI https://doi.org/10.2147/CLEP.S73857
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Professor Henrik Sørensen
Norbert Marschner,1 Dirk Arnold,2 Erik Engel,3 Ulrich Hutzschenreuter,4 Jacqueline Rauh,5 Werner Freier,6 Holger Hartmann,7 Melanie Frank,8 Martina Jänicke7
On behalf of the TKK Registry Group
1Praxis für Interdisziplinäre Onkologie und Hämatologie, 2Klinik für Tumorbiologie, Freiburg, Germany; 3Hämatologisch – Onkologische Praxis Altona, Hamburg, Germany; 4Hämatologisch – Onkologische Gemeinschaftspraxis, Nordhorn, Germany; 5Fachinternistische Gemeinschaftspraxis und Therapiezentrum, Witten, Germany; 6Onkologische Praxis, Hildesheim, Germany; 7Clinical Epidemiology and Health Economics, iOMEDICO, 8Statistics, iOMEDICO, Freiburg, Germany
Purpose: Several randomized trials investigating the preferable first-line combination chemotherapy regimen for metastatic colorectal cancer have shown inconsistent findings. Because a substantial number of patients are still being treated with "chemo-only" first-line therapies without targeted agents, we compared overall survival (OS) of patients treated in routine practice with oxaliplatin–fluoropyrimidine and irinotecan–fluoropyrimidine.
Patients and methods: Using the database of the Tumor Registry Colorectal Cancer, we identified 605 patients with metastatic colorectal cancer who received first-line fluoropyrimidine combination chemotherapy with either oxaliplatin (n=430) or irinotecan (n=175). The Tumor Registry Colorectal Cancer is a cohort study that prospectively documents treatment of colorectal cancer by office-based medical oncologists in Germany and has recruited over 5,000 patients. OS was estimated using the Kaplan–Meier method, and a multivariate Cox proportional hazard model was used to adjust for potentially confounding variables.
Results: Median OS was 26.8 (95% confidence interval [CI] 22.4–31.9) months with an oxaliplatin–fluoropyrimidine combination and 18.3 (95% CI 15.1–23.2) months with irinotecan–fluoropyrimidine first-line "chemo-only" therapy. Median progression-free survival was 9.0 (8.1–10.2) and 7.9 (7.2–10.2) months, respectively. The difference in OS was confirmed if analysis was restricted to patients with synchronous metastases (no prior treatment). Among other variables, proportion of patients receiving any second-line therapy did not differ between groups. Oxaliplatin-based first-line therapy was associated with improved OS in multivariate analysis adjusted for potentially confounding variables (hazard ratio 0.678, 95% CI 0.510–0.901, P=0.007).
Conclusion: In clinical routine practice, first-line treatment with oxaliplatin–fluoropyrimidine combination chemotherapy compared to irinotecan–fluoropyrimidine combination is associated with improved survival in patients with metastatic colorectal cancer, independent of all examined potentially confounding factors.
Keywords: colorectal neoplasms, epidemiology, irinotecan, oxaliplatin, cohort studies, treatment outcome
Introduction
The outcome of patients with metastatic colorectal cancer (mCRC) has improved significantly over the last two decades.
Three cytotoxic drugs are regularly used in the treatment of mCRC and form the backbone of all modern combination regimens: oxaliplatin, irinotecan, and fluoropyrimidines.1–4 Several randomized trials compared oxaliplatin–fluoropyrimidine versus irinotecan– fluoropyrimidine combination regimens4–10 but did not show consistent findings. Two meta-analyses favoring oxaliplatin–fluoropyrimidine combination chemotherapy as first-line treatment have been published, although the types of trials included are a subject of debate.11,12 In addition, non-interventional studies showed an association with oxaliplatin–fluoropyrimidine first-line treatment and improved survival.13–15 Nevertheless, irinotecan and oxaliplatin are regarded as equally effective agents, although having different mechanisms of action and toxicity profiles.16,17 Research focus has shifted to targeted agents, although a substantial number of patients are still being treated with “chemo-only” first-line therapies (database of the Tumorregister Kolorektales Karzinom [TKK, tumor registry colorectal cancer], unpublished data).
Randomized controlled trials are the most reliable method to establish efficacy of a given treatment, but they also include selected patient populations limiting the generalizability (external validity). Effectiveness in actual “real-life” clinical practice may differ, and clinical registries conducted at high methodological standards can provide additional evidence for a more realistic picture.18
Our study group of 269 German office-based medical oncologists has set up a registry in 2006 to prospectively document systemic treatment of colorectal cancer. Since 2006, data of more than 5,000 patients have been documented. We used our database to test the hypothesis that oxaliplatin–fluoropyrimidine is associated with improved OS compared to irinotecan–fluoropyrimidine as first-line chemotherapy in routine practice.
Patients and methods
Data source
The study cohort was derived from the TKK database. TKK was started in September 2006 and is a large ongoing, prospective, national registry conducted by a multicenter network of currently practicing 269 office-based medical oncologists in Germany. Participating physicians account for approximately 30% of all office-based specialists within the field of Hematology and Oncology in Germany.19 Patients with histologically confirmed colorectal cancer can be included if they signed informed consent no longer than 4 weeks after the start of systemic neoadjuvant/adjuvant treatment for nonmetastatic or first-line treatment for metastatic/inoperable disease. At the start of the registry in 2006, an additional 500 patients were recruited whose first-line treatment had started more than 4 weeks before consent. This was done so that treatment reality could be analyzed within the first year of the project. To minimize selection bias, study sites are asked to enroll patients consecutively and annual recruitment is restricted to eight patients per study site in neoadjuvant/adjuvant or palliative treatment, respectively. Patients are treated according to physicians’ choice. At the time of enrolment, data on patient and tumor characteristics are documented. During the course of therapy, all systemic antineoplastic treatments (substance, dose, and duration) as well as radiotherapies and/or surgeries are documented. Treatment outcome including best (clinical tumor) response(s) according to the assessment used by the study site, date(s) of progression, and date of death by any cause are recorded. All data, including data on mortality, are derived from patients’ medical records and transferred to a secure web-based electronic case report form by physicians or by trained study nurses. Data are updated after any examination, change in therapy, or at least every 6 months. All patients are followed up for a minimum of 3 years (or until death, lost to follow-up, or withdrawal of consent). There are automated plausibility and completeness checks and subsequently generated queries by the electronic data capture system. In addition, the database is checked regularly for completeness and plausibility, and study sites are contacted to correct data. Predefined analyses are performed biannually including descriptive analyses such as patients’ tumor characteristics, treatment patterns, and response to treatment. The study was reviewed by the ethics committee of the medical association of Baden-Würrtemberg, Germany.
Cohort definition
Data cut-off for the present interim analysis was March 31, 2012. By this time 4,593 patients with colorectal cancer had been recruited, of which 2,402 patients had started treatment for stage IV disease (Figure 1). Only patients who had signed informed consent no longer than 4 weeks after the start of palliative first-line treatment were included in further analysis to avoid immortal time bias, an overestimation of outcome data such as duration of OS. The cohort used for the present etiologic analysis included all patients who received first-line chemotherapy with fluoropyrimidine and oxaliplatin or irinotecan, without additional targeted agents (Figure 1). Fluoropyrimidine regimens were bolus or infusional regimens of 5-fluorouracil (5-FU), as well as capecitabine.
  | Figure 1 Cohort definition. |
Documentation of systemic therapies
The case report form (electronic case report form) does not capture predefined treatment regimens, such as FOLFOX6 or FOLFIRI. Instead, the individual drugs administered, the date of first and last dose, and the dosage and number of applications of each drug given are documented. Regarding fluoropyrimidines, administration route is specified (bolus 5-FU, infusional 5-FU, combination of both, or capecitabine). Neoadjuvant and adjuvant treatments are documented as such in the electronic case report form. A total of 11 patients (10 in the oxaliplatin-treated group and one in the irinotecan-treated group) started first-line treatment less than 6 months after the end of neoadjuvant/adjuvant treatment.
Statistical analysis
All analyses were performed using STATISTICA (StatSoft, Inc.) version 10.0 and R version 2.15.1. Time to events was analyzed using Kaplan–Meier estimates. OS was defined as the interval between the first administration of first-line chemotherapy and death from any cause. Patients alive or lost to follow-up were censored at last contact or at last documentation. Progression-free survival was defined as the interval between first administration and date of progression or death before the start of second-line therapy. Patients without such an event were censored at either the start of second-line therapy, end of first-line therapy, last contact, or last documentation. For estimates of treatment durations, patients who had not completed the respective line of treatment were censored at last contact or last documentation. As sensitivity analysis, OS was additionally analyzed for patients with synchronous metastases (M1, stage IV at initial diagnosis), who had thus not received any (neo)adjuvant chemotherapy.
A Cox proportional hazards model was used to account for potentially confounding variables. These variables were prospectively selected based on clinical relevance for either treatment decision making (potential confounding by indication) or differences in prognostic factors at baseline. Variables included were the following:
- patient characteristics at the start of first-line therapy: sex, Eastern Cooperative Oncology Group (ECOG) performance status, age, body mass index, Charlson comorbidity index,20 any comorbidity (yes or no);
- tumor characteristics: site of primary tumor (colon or rectum), stage at initial diagnosis (overall stage, T, N, M), tumor grading, lymph node ratio, Kirsten rat sarcoma (KRAS) status;
- treatment details: prior adjuvant or neoadjuvant treatment (yes or no), resection of primary tumor (yes or no), outcome of resection of primary tumor, time from initial diagnosis to start of first-line therapy, number of metastatic sites at the start of first-line therapy, fluoropyrimidine backbone, first-line combination therapy (oxaliplatin- or irinotecan-based).
The cut-off for lymph node ratio was prospectively defined based on literature.21 There was no imputation of missing data. As documentation in the registry reflects clinical routine practice, missing data are expected and unavoidable for some variables. Therefore, whenever possible, “missing” was included in the model as separate category.
Goodness of fit was measured by a likelihood-based pseudo R2. Internal model validation was performed using bootstrapping on the pseudo R2 and on hazard ratio (HR) and standard error of the oxaliplatin/irinotecan variable. A reduced model containing the most likely confounding variables, as well as sensitivity analysis (addition and reduction of parameters) all reported the oxaliplatin/irinotecan variable with a P-value <0.05.
Data were based on 546 patients because of missing data for individual variables.
All presented P-values are two-sided. There were no adjustments to the level of significance.
Results
Patient demographics
Of the 605 patients in our cohort, 430 patients received oxaliplatin–fluoropyrimidine and 175 patients received irinotecan–fluoropyrimidine combinations as first-line chemotherapy. Patient and tumor characteristics are listed in Table 1. A few imbalances were observed, regarding ECOG performance status, site of primary tumor, stage of disease at initial diagnosis, resection for primary tumor and synchronous metastasis. More patients in the oxaliplatin group had colon cancer or synchronous metastatic disease/tumor stage IV at initial diagnosis. More patients in the irinotecan-group underwent surgery for their primary tumor or had a poorer ECOG performance status.
  | Table 1 Patient and tumor characteristics of patients (N=605) with metastatic colorectal cancer treated in routine practice in Germany |
Systemic therapy
Duration of first-line chemotherapy and first-line progression-free survival did not differ between patients treated with oxaliplatin- or irinotecan-based chemotherapy: median treatment duration was 4.4 and 4.0 months (95% confidence interval [CI] 3.8–4.9 and 3.3–5.0), whereas median progression-free survival was 9.0 and 7.9 months (95% CI 8.1–10.2 and 7.2–10.2), respectively (Table 2). More patients treated with irinotecan had prior neoadjuvant or adjuvant chemotherapy and thus had been pretreated with “the other drug”, oxaliplatin. Conversely, more patients undergoing treatment with oxaliplatin received “the other drug”, irinotecan, in later line treatment. Overall, an equal number of patients received both drugs, irinotecan and oxaliplatin, within their course of disease (63% vs 60% in the oxaliplatin- and irinotecan-treated group, respectively).
Regimens of fluoropyrimidines differed between both groups: more patients treated with irinotecan combinations were given bolus or infusional 5-FU, whereas more patients treated with oxaliplatin received combined bolus/infusional 5-FU or capecitabine.
We found no differences in the proportion of patients receiving any second-line therapy (55.1% vs 51.4% in the oxaliplatin- and irinotecan-treated groups, 95% CI 50.3–59.9 and 43.8–59.0), and treatment duration of second-line therapy was comparable. A few more patients in the oxaliplatin-treated group were reported with complete or partial response in first-line (41.4% vs 31.4%) and in second-line (28.7% vs 16.7%) treatment. However, 95% CIs indicate no difference between the groups (Table 2).
Overall survival
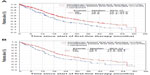
Patients treated with oxaliplatin combinations as first-line had a median OS of 26.8 months (95% CI 22.4–31.9) compared to 18.3 (95% CI 15.1–23.2) months for patients treated with irinotecan (Figure 2A). The median follow-up was 33.7 months for oxaliplatin and 35.7 months for the irinotecan combination.
The difference in OS favoring oxaliplatin combinations was confirmed if analysis was restricted to patients with synchronous metastatic disease, who had thus not received prior neoadjuvant or adjuvant therapy (Figure 2B). Median OS times were 26.1 months (95% CI 21.2–33.1) versus 18.2 months (95% CI 13.9–29.4), respectively.
Adjustment for potentially confounding variables
Cox proportional hazards model was used to verify the difference in Kaplan–Meier curves adjusted for potentially confounding variables.
Selection of an oxaliplatin-based first-line therapy was associated with improved survival in a univariate analysis (HR 0.671, 95% CI 0.525–0.858; P=0.001) and also in a multivariate analysis including all variables listed in Table 3 (HR 0.678; 95% CI 0.510–0.901, P=0.007).
  | Table 3 Cox regression analyses of overall survival of patients (N=605) with metastatic colorectal cancer treated with oxaliplatin- or irinotecan-based first-line chemotherapy in routine practice Germany |
Discussion
The data presented from the TKK registry show a difference of almost 8 months in median OS, favoring oxaliplatin–fluoropyrimidine combinations over irinotecan–fluoropyrimidine first-line chemotherapy and an association of oxaliplatin-based first-line therapy with improved OS after adjusting for multiple potentially confounding variables.
The results of this cohort study are limited by the non-interventional design. The observed difference in OS could be a result of differences in unknown baseline patient characteristics, not included into the multivariate model and reflecting either treatment decision making or differences in tumor biology (confounding by indication). To reduce bias to a minimum, all available data on potentially clinically relevant baseline characteristics were assessed. There were some imbalances in patient characteristics in our cohort, mostly reflecting the choice of first-line treatment in routine clinical practice. Patients with neoadjuvant or adjuvant pretreatment (which generally contains oxaliplatin) as well as patients with poor ECOG performance status more frequently received irinotecan-based regimens as first-line treatment.
More patients treated with oxaliplatin combinations had colon primary or synchronous metastatic disease. Nevertheless, the OS advantage for first-line oxaliplatin was confirmed in patients with synchronous metastatic disease (and thus without prior neoadjuvant or adjuvant treatment). We analyzed this elaborate number of potentially confounding variables in a multivariate analysis. Adjusted for the variables listed in Table 3, the association between oxaliplatin-based first-line therapy and improved OS remained.
It is possible that differences in factors downstream of exposure to first-line treatment account for the difference in OS, but we found no difference in the downstream variables (eg, proportion of second-line therapies).
Results similar to ours have been reported in both interventional and non-interventional studies.4–15,22 Several randomized trials compared different oxaliplatin–fluoropyrimidine and irinotecan–fluoropyrimidine combination regimens4–10 but did not show consistent findings.
The randomized Phase II GERCOR study4 reported similar median OS for sequential treatment with FOLFIRI followed by FOLFOX6 or vice versa (21.5 vs 20.6 months) in 220 evaluable patients. Of note, OS was a secondary endpoint, and there were imbalances between arms regarding second-line therapy and surgery to remove liver metastases.
Three randomized Phase III trials found a survival benefit for the oxaliplatin regimens, compared to the irinotecan regimens.5,6,9 An Italian study found a significant survival benefit for patients receiving first-line oxaliplatin (18.9 vs 15.6 months),6 where both drugs were combined with 5-FU bolus regimens. Two other trials compared oxaliplatin with infusional 5-FU to irinotecan with a 5-FU bolus regimens,5,9 potentially interfering with the assessment of the relative contribution of oxaliplatin and irinotecan.
A randomized Phase II study of oxaliplatin plus capecitabine versus irinotecan plus capecitabine as first-line treatment in 94 patients aged ≥70 years showed a 5.3-month difference in median OS in favor of the oxaliplatin regimen, although it did not reach statistical significance (P=0.162).10
In contrast, two trials found similar OS for oxaliplatin and irinotecan regimens. In a Phase III trial, oxaliplatin and irinotecan were combined with an infusional regimen,8 and in a Phase II trial, both drugs were combined with a bolus regimen.7
Two meta-analyses found oxaliplatin–FU regimens to be associated with superior survival.11,12 One may object that both analyses included the data of FOLFOX4 versus Irinotecan+5-FU,5,9 a bolus regimen no longer recommended for treatment of mCRC. However, a third meta-analysis came to a similar result favoring 5-FU + oxaliplatin.22 Compared to first-line treatment with 5-FU alone, the authors calculated a reduced risk of death by addition of oxaliplatin (HR 0.84) but a less pronounced reduced risk for irinotecan (HR 0.91). The risk was still reduced but almost identical when studies with bolus treatment were excluded (HR 0.91 vs 0.89, respectively).22
In addition to the randomized trials, several non-interventional studies using data from patients in real-world clinical practice have reported results similar to ours.13–15 A cohort study using a joint SEER-Medicare database showed markedly longer OS in seemingly comparable populations for patients who received only FOLFOX chemotherapy compared to FOLFIRI as first-line treatment (19.2 vs 13.3 months).13 Improved median OS for oxaliplatin-based versus irinotecan-based combination therapy was estimated for elderly (≥75 years, HR 0.62), younger (<75 years, HR 0.67), and all patients (HR 0.65) with stage IV colon cancer using a different SEER-Medicare data set.15 Finally, a pharmacoeconomic study is worth mentioning, which also found a significant survival advantage by Cox analysis for FOLFOX over FOLFIRI (HR 5.2) in patients identified from a database using medicine and pharmacy.14
In conclusion, we believe that the concept that combination chemotherapies with oxaliplatin or irinotecan are equally effective as first-line treatment of mCRC should be reconsidered. Our data and results from both randomized controlled trials as well as other non-interventional studies repeatedly show an association of oxaliplatin-based first-line therapies with improved survival compared to irinotecan-based first-line therapy. While more and more patients are now being treated with chemotherapy in combination with targeted agents, a substantial number does not receive these novel substances, highlighting the importance of this question. It will also be of interest, whether the use of targeted agents will affect effectiveness of these two chemotherapy regimens differently. Because our analysis was restricted to “chemo-only” first-line therapies, it is planned to investigate these data in patients treated with first-line targeted therapies in a forthcoming analysis.
Acknowledgments
The authors thank all members of the TKK Registry Group and all patients for participating in this study. The TKK Registry Group collaborates with the Arbeitsgemeinschaft Internistische Onkologie and the Arbeitskreis Klinische Studien. The authors thank Susanne Hell for writing the initial draft of the manuscript and Stefanie Kopfmann for support during the revisions. The TKK is funded by iOMEDICO.
Disclosure
The authors report no conflicts of interest in this work.
References
Van Cutsem E, Nordlinger B, Cervantes A. Advanced colorectal cancer: ESMO clinical practice guidelines for treatment. Ann Oncol. 2010;21(Suppl 5):v93–v97. | |
NCCN. NCCN Clinical Practice Guidelines: Colon Cancer. Fort Washington, PA: NCCN; 2013. | |
Grothey A, Sargent D, Goldberg RM, Schmoll H-J. Survival of patients with advanced colorectal cancer improves with the availability of fluorouracil-leucovorin, irinotecan, and oxaliplatin in the course of treatment. J Clin Oncol. 2004;22(7):1209–1214. | |
Tournigand C, André T, Achille E, et al. FOLFIRI followed by FOLFOX6 or the reverse sequence in advanced colorectal cancer: a randomized GERCOR study. J Clin Oncol. 2004;22(2):229–237. | |
Goldberg RM, Sargent DJ, Morton RF, et al. A randomized controlled trial of fluorouracil plus leucovorin, irinotecan, and oxaliplatin combinations in patients with previously untreated metastatic colorectal cancer. J Clin Oncol. 2004;22(1):23–30. | |
Comella P, Massidda B, Filippelli G, et al. Oxaliplatin plus high-dose folinic acid and 5-fluorouracil iv bolus (OXAFAFU) versus irinotecan plus high-dose folinic acid and 5-fluorouracil iv bolus (IRIFAFU) in patients with metastatic colorectal carcinoma: a Southern Italy Cooperative Oncology Group phase III trial. Ann Oncol. 2005;16(6):878–886. | |
Kalofonos HP, Aravantinos G, Kosmidis P, et al. Irinotecan or oxaliplatin combined with leucovorin and 5-fluorouracil as first-line treatment in advanced colorectal cancer: a multicenter, randomized, phase II study. Ann Oncol. 2005;16(6):869–877. | |
Colucci G, Gebbia V, Paoletti G, et al; Gruppo Oncologico Dell’Italia Meridionale. Phase III randomized trial of FOLFIRI versus FOLFOX4 in the treatment of advanced colorectal cancer: a multicenter study of the Gruppo Oncologico Dell’Italia Meridionale. J Clin Oncol. 2005;23(22):4866–4875. | |
Goldberg RM, Sargent DJ, Morton RF, et al. Randomized controlled trial of reduced-dose bolus fluorouracil plus leucovorin and irinotecan or infused fluorouracil plus leucovorin and oxaliplatin in patients with previously untreated metastatic colorectal cancer: a North American Intergroup Trial. J Clin Oncol. 2006;24(21):3347–3353. | |
Rosati G, Cordio S, Bordonaro R, et al. Capecitabine in combination with oxaliplatin or irinotecan in elderly patients with advanced colorectal cancer: results of a randomized phase II study. Ann Oncol. 2010; 21(4):781–786. | |
Zhuang L, Bai J, Huang H, et al. Meta-analysis of chemotherapy with irinotecan or oxaliplatin-involved regimen for untreated metastatic advanced colorectal cancer. Oncol Res. 2010;18(9):437–444. | |
Liang X-B, Hou S-H, Li Y-P, Wang L-C, Zhang X, Yang J. Irinotecan or oxaliplatin combined with 5-fluorouracil and leucovorin as first-line therapy for advanced colorectal cancer: a meta-analysis. Chin Med J (Engl.). 2010;123(22):3314–3318. | |
Meyerhardt JA, Li L, Sanoff HK, Carpenter W 4th, Schrag D. Effectiveness of bevacizumab with first-line combination chemotherapy for medicare patients with stage IV colorectal cancer. J Clin Oncol. 2012;30(6):608–615. | |
Nelson MA, Shetty S, Kulakodlu M, Harley C, Seal B. A comparison of mortality and costs associated with FOLFOX versus FOLFIRI in stage IV colorectal cancer. J Med Econ. 2011;14(2):179–186. | |
Mullins CD, Hsiao F-Y, Onukwugha E, Pandya NB, Hanna N. Comparative and cost-effectiveness of oxaliplatin-based or irinotecan-based regimens compared with 5-fluorouracil/leucovorin alone among US elderly stage IV colon cancer patients. Cancer. 2012;118(12):3173–3181. | |
Van Cutsem E, Cervantes A, Nordlinger B, Arnold D; ESMO Guidelines Working Group. Metastatic colorectal cancer: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2014;25(Suppl 3):iii1–iii9. | |
Schmiegel W, Tannapfel A, Pox C, Aretz S, Bischoff SC, Graeven U. S3-Leitlinie Kolorektales Karzinom. Langversion 1.0, AWMF, 021-007OL, http://leitlinienprogramm-onkologie.de/Leitlinien.7.0.html. Accessed August 8, 2013. | |
Levine MN, Julian JA. Registries that show efficacy: good, but not good enough. J Clin Oncol. 2008;26(33):5316–5319. | |
Bundesärztekammer. Tätigkeitsbericht 2010 Der Bundesärztekammer [Activity Report of the German Medical Association 2010]. Kiel; 2011:1–643. Available from: http://www.bundesaerztekammer.de/downloads/Taetigkeit2010.pdf. Accessed October 21, 2012. | |
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383. | |
Noura S, Ohue M, Kano S, et al. Impact of metastatic lymph node ratio in node-positive colorectal cancer. World J Gastrointest Surg. 2010;2(3):70–77. | |
Golfinopoulos V, Salanti G, Pavlidis N, Ioannidis JP. Survival and disease-progression benefits with treatment regimens for advanced colorectal cancer: a meta-analysis. Lancet Oncol. 2007;8(10):898–911. | |
Edge S, Byrd DR, Compton CC, Fritz AG, Greene FL, Trotti A. AJCC Cancer Staging Manual. 7th ed. New York: Springer; 2010. |
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.