Back to Journals » HIV/AIDS - Research and Palliative Care » Volume 13
ART Adherence Among People Living with HIV Seeking Services from Public Health Facilities in Western Ethiopia
Authors Tolossa T , Wakuma B , Mulisa D , Besho M , Tsegaye R , Tigistu M , Kebebe H , Markos J , Hiko N, Hasen T, Wirtu D
Received 10 September 2021
Accepted for publication 10 December 2021
Published 29 December 2021 Volume 2021:13 Pages 1149—1158
DOI https://doi.org/10.2147/HIV.S336647
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Bassel Sawaya
Tadesse Tolossa,1 Bizuneh Wakuma,2 Diriba Mulisa,2 Merga Besho,3 Reta Tsegaye,2 Mekdes Tigistu,1 Habtamu Kebebe,3 Jote Markos,2 Nesru Hiko,2 Tahir Hasen,2 Desalegn Wirtu1
1Department of Public Health, Institute of Health Sciences, Wollega University, Nekemte, Ethiopia; 2Department of Nursing, Institute of Health Sciences, Wollega University, Nekemte, Ethiopia; 3Department of Midwifery, Institute of Health Sciences, Wollega University, Nekemte, Ethiopia
Correspondence: Tadesse Tolossa
Department of Public Health, Institutes of Health Sciences, Wollega University, P.O.Box: 395, Nekemte, Ethiopia
Tel +251911936804
Email [email protected]
Background: The burden of COVID-19 is more severe among the elderly and patients affected with chronic medical conditions like diabetes, cardiovascular diseases, and HIV/AIDS. There is no study regarding the level of adherence to antiretroviral therapy (ART) during the time of COVID-19 in Ethiopia. So, this study aimed to assess the level of HIV positive patient’s adherence to ART treatment and associated factors in Nekemte public health facilities, Western Ethiopia.
Methods: This study was conducted in Nekemte public health facilities, Western Ethiopia from August 1, 2020 to September 30, 2020. A facility-based cross-sectional study was employed among HIV positive patients on ART treatment. A single proportion formula was used to calculate a sample size of 384 . A systematic random sampling technique was employed to select the sample population. Face-to-face interview questionnaires were used during data collection. A binary logistic regression model was fitted to identify factors associated with dependent factor, and an adjusted odds ratio (AOR) was used to estimate the strength of the association between dependent and independent variables.
Results: A total of 361 HIV positive patients have participated in the study, yielding a response rate of 94%. The mean age of the participants was 33.8 (SD ± 9.8) years. Seventy-seven (21.3%) HIV-positive patients had not adhered to ART follow-up. The study found that living in rural areas (AOR=3.37, 95% CI=1.80– 6.24), age less than 25 years (AOR=3.41, 95% CI=1.26– 9.21), and substance use (AOR=5.42, 95% CI=1.8– 16.29) were independent predictors of poor adherence to ART.
Conclusion: Generally, non-adherence to antiretroviral treatment among people living with HIV during the pandemic outbreak was high in the study area. A home-based delivery of ART treatment and improving retention mechanism during pandemics is highly recommended for concerned bodies. In addition, counseling on avoidance of substance use should be strengthened to increase retention on treatment.
Keywords: adherence, ART, HIV, Ethiopia
Introduction
The symptoms and burden of corona virus disease (COVID-19) are more severe among the elderly, pregnant women, and patients who are affected with chronic non-communicable diseases such as Diabetes Mellitus, cardiovascular diseases, and HIV/AIDS.1 As a result, increasing cases of COVID-19 are anticipated to rapidly occur in people living with chronic medical diseases due to several comorbidities having been identified as risk factors for severe disease and death.2
Globally, Sub-Saharan Africa (SSA) shares the highest number of people living with HIV. In 2019, more than 20 million people were living with HIV in SSA and the prevalence of HIV among the adult population was 6.7% and more than 73% of the HIV positive population was on ART.3 The number of people living with HIV in this area is increasing over time, and the need for ART is also high. However, the rate of attrition to the treatment is low when compared with other WHO regions.3,4 A systematic review and meta-analysis done in SSA revealed the level of adherence to ART was 72.9%.5 A systematic review and meta-analysis conducted in Ethiopia showed that the level of ART adherence ranges from 32.9% to 94%.6
The consequences of poor adherence to ART include drug resistance, increase mortality rates, poor treatment outcome, occurrence of opportunistic infections, and increased susceptibility to different comorbidities.7 In SSA, the consequence of poor adherence to ART is high due to the distance of the health facility to access treatment, poor healthcare system, poor tracing mechanism, lack of advanced technology such as tele-health, and stigma related to the disease.8
Factors such as lack of disclosing the HIV sero-status,6,9 being unmarried,6,10 advanced stage of the disease,6,10 substance use,6,11,12 alcohol drinker,10 tobacco smoker,10 having mental illness,10,12 and bedridden functional status10 were factors that contributed to the poor adherence to ART. A qualitative study conducted in Southern Ethiopia, shows poor economic status, perceived stigma and discrimination, fasting, holy water, medication side-effects, and dissatisfaction with healthcare services were major reasons for non-adherence to ART.13
In addition, poor adherence to ART during the era of COVID-19 results from preventing health careworkers from home visits, inadequate infrastructure and staff shortages.14 People living with HIV may interrupt their treatment due to the stay home strategies of COVID-19 prevention.8 A study conducted in China showed that 32.6% of people living with HIV were at risk of discontinuing ART due to COVID-19 lockdown measures.15
Even though SSA is one of the regions least affected by the COVID-19 pandemic, the pandemic may tend to shift to this region due to different reasons such as the large amount of people living with HIV in this area, the public compliance to public health measures being very poor, the weak healthcare systems, and lack of trained human power.16 The international organizations such as WHO and UNAIDS are calling on all concerned bodies (governments, healthcare providers, and policy-makers) to develop and implement a mechanism that reduces interference in access and adherence to ART treatment for people living with HIV.17 In order to develop effective mechanisms for retention of HIV-positive patients on ART, identifying the level of adherence to treatment is of paramount importance. However, the level of ART adherence during the pandemic is not well studied in Ethiopia in general, and in this tudy area in particular. So, this study aimed to assess the level of adherence to ART and associated factors among HIV positive patients in western Ethiopia.
Methods
Study Setting and Study Period
The study was conducted in health facilities found in Nekemte town, Oromia regional state, western Ethiopia. The town is 331 km to the west of the capital city, Addis Ababa. There are two health centers, one specialized hospital, and one referral hospital in Nekemte town. The study period was from August 1, 2020 to September 30, 2020.
Study Design
An institutional-based cross-sectional study design was employed.
Population
Source populations were all HIV-positive patients in public health facilities of Nekemte town, and the study population were all HIV-positive patients in selected public health facilities of Nekemte town.
Sample Size and Sampling Procedure
Sample size was determined by using a single population proportion formula with the following assumptions: P=50%, with a margin of error 5%, and 95% confidence level. The final sample size for this study was 384.
Four public health facilities are found in Nekemte town (Wollega University referral hospital, Nekemte specialized hospital, Calalaki HC, and Bake Jama health center). Nekemte specialized hospital and Bake Jama health centers were selected purposely because Wollega University referral hospital served as a treatment center for COVID-19 cases and Calalaqi health center has been serving as an isolation center. Then to select samples from each hospital, samples were proportionally allocated to each hospital, which was estimated based on their average patient flow for outpatient services in the months prior to data collection. Accordingly, prior to data collection, 582 and 368 patients had visited the ART clinic at Nekemte specialized hospital and Bake Jama health center, respectively. After the sample was equally distributed to both health facilities, a systematic random sampling technique was used to select samples from each hospital with K=2. K was separately estimated for the two health facilities. For Nekemte specialized hospital, K=582/235=2 and for Bake Jama Health Center, K=374/149=2. Finally, the first participant was selected by lottery method for both health facilities (Figure 1).
 |
Figure 1 Schematic presentation of sampling procedure. |
Variables and Outcome Measurement
Adherence to ART was a dependent variable. Socio-demographic variables (such as age, sex, marital status, residence, educational status, religion, occupation, family size, number of children in the household, disclosure status), behavioral variables (physical activities, alcohol, coffee drinking), disease related variables (type of illness, severity, time of diagnosis, co-morbidity, and complication, family history), clinical and laboratory variables (CD4 level, functional status, and WHO clinical stage) were independent variables.
The level of adherence was assessed by counting the number of pills that remain from the last month prescribed drug when he/she comes for follow-up. Patients who reported an intake of ≥ 95% of the prescribed medication were considered as having adhered to ART (good adherence); and those with a reported intake of <95% were considered as having not adhered to ART (poor adherence).18,19
Data Collection Techniques and Data Quality Assurance
A questionnaire was developed after an extensive review of similar literature of previously published papers on ART adherence20–23 and WHO recommendations.24 A structured and pretested questionnaire was used to collect data through face-to-face interviews. The questionnaire was administered in locally spoken language (Afaan Oromoo) to ease the interview processes. The questionnaire was translated first into Afaan Oromoo and back to English to assure its consistency. Four diploma holder Nurses were recruited for data collection. The questionnaire was pre-tested on 5% of participants. Then possible amendments were done based on the findings. A discussion was had between investigators and data collectors, based on the result of the pre-test and, accordingly, some amendments were made. One day of training was given to the data collectors about the tool and data collection procedure. Data were checked for completeness, accuracy, clarity, and consistency by the supervisors and principal investigator on a daily basis.
Data Analysis
The collected questionnaire was checked manually for its completeness, and data entry was performed by using Epidata version 7.1 statistical packages. Finally, data analysis was performed by using STATA version 14.0. Data cleaning, edition, and exploration was done by using simple frequencies and cross-tabulation. Descriptive analysis, like frequencies, percentages, mean and standard deviation were computed. Re-categorization of categorical variables and categorization of continuous variables was done. The assumption of the logistic regression model was checked by the chi-square test. The binary logistic regression model was used to determine factors associated with poor adherence to ART. Factors that were associated with poor adherence to ART at a P-value of ≤0.25 significant level in the bivariable logistic regression were included in the multivariable logistic regression. The model was selected by using a backward stepwise selection process. Then crude and adjusted odds ratio (AOR) together with their corresponding 95% confidence intervals were presented in the final multivariable logistic regression table. A statistical significance was declared when it was significant at a 5% level (p-value<0.05). Multicollinearity (association between explanatory variables) was checked and the model goodness of fit test was checked by Hosmer and Lemeshow test.
Ethical Considerations
The study was approved by Wollega university research Ethics review board (WURB) and ethical clearance letters were obtained. After approval, a permission letter was obtained from the administrative body of the hospital to respective clinics. Verbal informed consent was approved by Wollega University research Ethics review board, and the patients were informed about the purpose of this study before commencing the interview. Everybody participated voluntarily, and the data was collected in accordance with the Declaration of Helsinki.
Results
Socio-Demographic Characteristics of the Patients
Three hundred and sixty-one (361) HIV positive patients participated in this study, yielding a response rate of 94%. The mean±standard deviation (SD) age of patients was 33.8±9.8 years. One hundred and forty-eight (41.0%) belong to age group 25–34 years. The study revealed that 196 (54.0%) study participants were female and 303 (83.9%) patients were residing in urban areas. Out of the total participants, 264 (73.1%) were married, and 111 (30.8%) participants had attended primary education. Two hundred and eighteen (60.4%) participants were protestant religion followers, followed by orthodox (26.6%) (Table 1).
 |
Table 1 Socio-Demographic Characteristics of HIV Positive Patients on ART in Nekemte Health Facilities, Western Ethiopia, 2020 |
Clinical, Laboratory, and Behavioral Characteristics of HIV Positive Patients
The mean CD4 level of patients on ART was 564 cells/µL with a SD of ±233.7 cells/µL. Two hundred and twenty-three (61.8%) patients CD4 levels were greater than ≥500 cells/µL and 328 (90.9%) HIV-positive patients were in WHO clinical stage I. The majority (93.6%) of the patient’s functional status was working and half (52.2%) had one or two types of comorbidity. The mean duration that patients had received treatment was 8.5 years with a SD of ±3.93 years. Regarding behavioral factors, 245 (67.8%) of the participants had participated in physical activities. Nearly half (52.9%) of the patients had a history of alcohol consumption prior to data collection (Table 2).
 |
Table 2 Clinical, Laboratory and Behavioral Characteristics of HIV Positive Patients on ART in Nekemte Public Health Facilities, Western Ethiopia, 2020 |
Magnitude of ART Adherence
From a total of 361 respondents, 284 (78.7%) had good adherence to ART treatment and 21.3% had poor adherence to ART treatment (Figure 2).
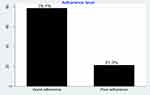 |
Figure 2 Level of ART adherence among HIV positive patients on ART in Western Ethiopia, 2020. |
Factors Associated with Poor Adherence to ART
The result of multivariable logistic regression showed that variables such as residence, age, and substance use were found to be significantly associated with poor adherence to ART treatment.
The odds of poor adherence to ART were 3.37-times higher among patients who resided in rural areas as compared to those patients who were from rural areas (OR=3.37, 95% CI=1.80–6.24). The odds of not adhering to ART were 3.41-times higher among patients aged less than 25 years as compared to their counterparts (OR=3.41, 95% CI=1.26–9.21). Substance use was also strongly associated with poor adherence to ART treatment. The odds of not adhering to ART was 5.42-times higher among substance user patients as compared to those patients who had not used substances (OR=5.42, 95% CI=1.8–16.29) (Table 3).
 |
Table 3 Multivariable Analysis of Adherence Status and Associated Factors Among HIV Positive Patients on ART Follow-Up in Nekemte Health Facilities, Western Ethiopia, 2020 |
Discussion
Non-adherence to ART among people living with HIV was 21.3% in the study area. Living in rural areas, a young age group, and substance use were independent determinants of poor adherence to ART of people living with HIV. Non-adherence to ART is the major determinant of missed virologic suppression, developing ART resistance, progression of HIV infection to disease, and low survival rate from the disease.7 Comprehensive medical care and treatment for people living with HIV can be affected by the overburden of the health services. The present study has pointed out that about 21.3% of people living with HIV poorly adhered to their routine ART medications. This is comparable to a study done in a regional hospital of Sokode, Togo (21.6%).25 However, this finding is higher compared to a study done in Vientiane, Laos in which 5% of people living with HIV were non-adherent to antiretroviral therapy,26 and lower than studies done in India (36.3%)27 and West Shewa in Ethiopia (33.8%).28 Besides, a previous study conducted in Nekemte town, Western Ethiopia, among the general population showed the magnitude of poor adherence to ART treatment was 19%29 and a higher non-adherent rate was observed in the current study compared to a study done in southwest Ethiopia (5%).30 This might be related with the time when the data were collected. The current study was collected during the time of the COVID-19 pandemic and this is scientifically supported by a previous study in which the level of adherence to ART was low during COVID-19 due to home stay measurements, closure of the health institution for COVID-19 treatment purposes, and fear of COVID-19.14 In addition, this may be due to the lockdown to mitigate the pandemic which resulted in reduced access to ART or missing the appointments fearing COVID-19. Coronavirus incurred an extra burden to people living with HIV. A study done by Fodjo et al31 in Belgium and Brazil has shown that 17.7% of people living with HIV had faced a challenge in obtaining ART due to COVID-19 related measures and thus interrupted HIV care. Moreover, a study done in Atlanta, GA also revealed that one in five participants missed a scheduled HIV care appointment due to COVID-19.32 A study done by Quiros-Roldan et al33 in Italy has also shown raised missed ART clinic visits following COVID-19.
With regard to determinants of ART adherence, living in a rural area, young age group, and substance use were independent determinants of poor ART adherence in the present study. The odds of poor ART adherence was more than 3-fold higher among patients who were living in rural areas than patients from urban areas. This is in line with studies conducted in different settings34,35 in which living in rural areas decreases the adherence to ART treatment. This may be related with the traveling time and cost to the health institution, and lack of availability of infrastructure and health services in a nearby area. In addition, this could be related to the educational status, in which the urban population are more educated with good access to media and information.
The level of poor adherence to ART therapy was significantly affected by the age of the patients, where patients in the age group of ≤24 years were more likely to be non-adherent to ART treatment. This is similar to studies conducted in Ethiopia36,37 that had found an increased level of adherence as age goes beyond 25 years. During the time of COVID-19, the young population may not visit health institutions due to fear of discrimination and stigma. So it is better to reach this group of people with contextually appropriate interventions. Government communication channels should continue with additional efforts to reach all individuals.
Moreover, the present study showed that substance abusers were 5.33-times more likely to have poor adherence to ART. This finding is supported by existing pieces of evidences from Togo, India, and Vientiane, Laos.25–27 This can be explained as substance abusers might have their own temporary world and cannot realize the real world that influenced them to have poor ART adherence during the pandemic. Staying at home was among the COVID-19 preventive measures that can expose patients to stress/depression and as a result substance use to treat the experienced stress/depression, which eventually resulted in poor ART adherence during the pandemic.
Conclusion and Recommendation
Generally, non-adherencve to ART among people living with HIV was high in the study area. Living in a rural area, being in a young age group, and substance use were independent determinants of poor adherence to antiretroviral treatment of people living with HIV. Since the population of rural settings are at higher risk of not adhering to ART follow-up, home-based delivery of ART treatment and improving the retention mechanism during pandemics is highly recommended for concerned bodies. Moreover, discouraging substance use has a vital role in improving adherence to ART, as this negatively influences adherence to antiretroviral treatment of people living with HIV.
Abbreviations
ART, Antiretro viral therapy; AOR, Adjusted Odds Ratio; COR, Crude Odds Ratio; HIV, Human Immune virus; NGO, Non-governmental organization; WHO, World Health Organization; SSA, Sub Saharan Africa.
Data Sharing Statement
All data analyzed during this study are included in the manuscript.
Acknowledgments
We would like to acknowledge Wollega University for covering data collectors and supervisors per diem. In addition, this manuscript was presented at the 31st annual research conference of Ethiopia Public Health Association (EPHA) in March 2021 (https://etpha.org/conference/index.php/32ndConference/32ndConference/paper/view/3156), and we would like to acknowledge EPHA for disseminating our research findings for research communities. Also, we would like to thank Nekemte town health office, Nekemte specialized hospital, and Chalalaki Health center for their invaluable co-operation during data collection and our deep thanks also goto the data collectors and supervisors for their interest and commitment in carrying out the study.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
No funding was obtained for this study.
Disclosure
The authors declare that they have no competing interests.
References
1. WHO. Coronavirus; 2020. Available from: https://www.who.int/health-topics/coronavirus#tab=tab_1.
2. Härter G, Spinner CD, Roider J, et al. COVID-19 in people living with human immunodeficiency virus: a case series of 33 patients. Infection. 2020:1. doi:10.1007/s15010-020-01438-z
3. UNAIDS. HIV and AIDS in East and Southern Africa regional overview; 2019.
4. Hardon AP, Akurut D, Comoro C, et al. Hunger, waiting time and transport costs: time to confront challenges to ART adherence in Africa. AIDS Care. 2007;19(5):658–665. doi:10.1080/09540120701244943
5. Heestermans T, Browne JL, Aitken SC, et al. Determinants of adherence to antiretroviral therapy among HIV-positive adults in sub-Saharan Africa: a systematic review. BMJ Glob Health. 2016;1(4):e000125. doi:10.1136/bmjgh-2016-000125
6. Moges NA, Olubukola A, Micheal O, et al. HIV patients retention and attrition in care and their determinants in Ethiopia: a systematic review and meta-analysis. BMC Infect Dis. 2020;20(1):1–24.
7. Hogan DR, Salomon JA. Prevention and treatment of human immunodeficiency virus/acquired immunodeficiency syndrome in resource-limited settings. Bull World Health Organ. 2005;83:135–143.
8. Chenneville T, Gabbidon K, Hanson P, et al. The impact of COVID-19 on HIV treatment and research: a call to action. Int J Environ Res Public Health. 2020;17(12):4548. doi:10.3390/ijerph17124548
9. Dessie G, Wagnew F, Mulugeta H, et al. The effect of disclosure on adherence to antiretroviral therapy among adults living with HIV in Ethiopia: a systematic review and meta-analysis. BMC Infect Dis. 2019;19(1):1–8. doi:10.1186/s12879-019-4148-3
10. Gesesew HA, Ward P, Hajito KW, et al. Discontinuation from antiretroviral therapy: a continuing challenge among adults in HIV care in Ethiopia: a systematic review and meta-analysis. PLoS One. 2017;12(1):e0169651. doi:10.1371/journal.pone.0169651
11. Arage G, Tessema GA, Kassa H. Adherence to antiretroviral therapy and its associated factors among children at South Wollo Zone Hospitals, Northeast Ethiopia: a cross-sectional study. BMC Public Health. 2014;14(1):1–7. doi:10.1186/1471-2458-14-365
12. Gebrezgabher BB, Kebede Y, Kindie M, et al. Determinants to antiretroviral treatment non-adherence among adult HIV/AIDS patients in northern Ethiopia. AIDS Res Ther. 2017;14(1):1–7. doi:10.1186/s12981-017-0143-1
13. Bezabhe WM, Chalmers L, Bereznicki LR, et al. Barriers and facilitators of adherence to antiretroviral drug therapy and retention in care among adult HIV-positive patients: a qualitative study from Ethiopia. PLoS One. 2014;9(5):e97353. doi:10.1371/journal.pone.0097353
14. Nyoni T, Okumu M. COVID-19-compliant strategies for supporting treatment adherence among people living with HIV in Sub-Saharan Africa. AIDS Behav. 2020;24(9):2473–2476. doi:10.1007/s10461-020-02888-0
15. Jiang H, Zhou Y, Tang W. Maintaining HIV care during the COVID-19 pandemic. Lancet HIV. 2020;7(5):e308–e309. doi:10.1016/S2352-3018(20)30105-3
16. Baggaley RF, Irvine MA, Leber W, et al. Cost-effectiveness of screening for HIV in primary care: a health economics modelling analysis. Lancet HIV. 2017;4(10):e465–e474. doi:10.1016/S2352-3018(17)30123-6
17. World Health Organization. Mental health and psychosocial considerations during the COVID-19 outbreak, 18 March 2020. World Health Organization; 2020.
18. Federal Ministry of Health (FMoH). Competency based national comprehensive PMTCT/MNCH training participant’s manual. Addis Ababa; 2017.
19. Federal Ministry of Health (FMOH) Ethiopia. National consolidated guidelines for comprehensive HIV prevention, care and treatment; 2018.
20. Iradukunda PG, Pierre G, Muhozi V, et al. Knowledge, attitude, and practice towards COVID-19 among people living with HIV/AIDS in Kigali, Rwanda. J Community Health. 2021;46(2):245–250. doi:10.1007/s10900-020-00938-1
21. Akalu Y, Ayelign B, Molla MD. Knowledge, attitude and practice towards COVID-19 among chronic disease patients at Addis Zemen Hospital, Northwest Ethiopia. Infect Drug Resist. 2020;13:1949. doi:10.2147/IDR.S258736
22. Defar A, Molla G, Abdella S, et al. Knowledge, practice and associated factors towards the prevention of COVID-19 among high-risk groups: a cross-sectional study in Addis Ababa, Ethiopia. PLoS One. 2021;16(3):e0248420. doi:10.1371/journal.pone.0248420
23. Adhena G, Hidru HD. Knowledge, attitude, and practice of high-risk age groups to coronavirus disease-19 prevention and control in Korem District, Tigray, Ethiopia: cross-sectional study. Infect Drug Resist. 2020;13:3801. doi:10.2147/IDR.S275168
24. World Health Organization. Infection prevention and control guidance for long-term care facilities in the context of COVID-19: interim guidance, 21 March 2020. World Health Organization; 2020.
25. Yaya I, Landoh DE, Saka B, et al. Predictors of adherence to antiretroviral therapy among people living with HIV and AIDS at the regional hospital of Sokodé, Togo. BMC Public Health. 2014;14(1):1308. doi:10.1186/1471-2458-14-1308
26. Hansana V, Sanchaisuriya P, Durham J, et al. Adherence to antiretroviral therapy (ART) among people living with HIV (PLHIV): a cross-sectional survey to measure in Lao PDR. BMC Public Health. 2013;13(1):617. doi:10.1186/1471-2458-13-617
27. Madi D, Bhaskaran U, Ramapuram J, et al. Adherence to antiretroviral therapy among people living with HIV. N Am J Med Sci. 2013;5(3):220. doi:10.4103/1947-2714.109196
28. Yadeta AD, Chaka EE. Predictors of art adherence among people living with human immune virus attending treatment at hospitals in West Shewa Zone, Oromia Region, Ethiopia, 2015. J Health Med Nurs. 2016;29.
29. Ejigu M, Desalegn Z, Mulatu B, et al. Adherence to combined antiretroviral therapy and associated factors among people living with HIV attending Nekemte Specialized Hospital, Oromia, Ethiopia: a cross-sectional study. HIV/AIDS (Auckland, NZ). 2020;12:97.
30. Tiyou A, Belachew T, Alemseged F, et al. Predictors of adherence to antiretroviral therapy among people living with HIV/AIDS in resource-limited setting of southwest Ethiopia. AIDS Res Ther. 2010;7(1):39. doi:10.1186/1742-6405-7-39
31. Fodjo JNS, de Moura Villela EF, Van Hees S, et al. Impact of the COVID-19 pandemic on the medical follow-up and psychosocial well-being of people living with HIV: a cross-sectional survey. J Acquir Immune Defic Syndr. 2020;85(3):257–262. doi:10.1097/QAI.0000000000002468
32. Kalichman SC, Eaton LA, Berman M, et al. Intersecting pandemics: impact of SARS-CoV-2 (COVID-19) protective behaviors on people living with HIV, Atlanta, Georgia. J Acquir Immune Defic Syndr. 2020;85(1):66–72. doi:10.1097/QAI.0000000000002414
33. Quiros-Roldan E, Magro P, Carriero C, et al. Consequences of the COVID-19 pandemic on the continuum of care in a cohort of people living with HIV followed in a single center of Northern Italy. AIDS Res Ther. 2020;17(1):1–8. doi:10.1186/s12981-020-00314-y
34. Molla AA, Gelagay AA, Mekonnen HS, et al. Adherence to antiretroviral therapy and associated factors among HIV positive adults attending care and treatment in University of Gondar Referral Hospital, Northwest Ethiopia. BMC Infect Dis. 2018;18(1):1–8. doi:10.1186/s12879-018-3176-8
35. Hailasillassie K, Etana B, Alemayehu M, et al. Factors associated with adherence of highly active antiretroviral therapy among adult HIV/AIDS patients in Mekelle Hospital Northern Ethiopia. Sci J Public Health. 2014;2(4):367–372. doi:10.11648/j.sjph.20140204.30
36. Letta S, Demissie A, Oljira L, et al. Factors associated with adherence to Antiretroviral Therapy (ART) among adult people living with HIV and attending their clinical care, Eastern Ethiopia. BMC Int Health Hum Rights. 2015;15(1):1–7. doi:10.1186/s12914-015-0071-x
37. Angelo AT, Alemayehu DS. Adherence and its associated factors among adult HIV-infected patients on antiretroviral therapy in South Western Ethiopia, 2020. Patient Prefer Adherence. 2021;15:299. doi:10.2147/PPA.S298594
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
