Back to Journals » Clinical Ophthalmology » Volume 18
Application of a Revised Tissue Saving Protocol for Combined Topography-Guided Photorefractive Keratectomy and Cross-Linking in a Cohort Having Pellucid Marginal Degeneration
Authors Omar Yousif M, Elkitkat RS , Hamza MN, Abdelsadek Alaarag N
Received 14 November 2023
Accepted for publication 18 January 2024
Published 1 February 2024 Volume 2024:18 Pages 303—311
DOI https://doi.org/10.2147/OPTH.S449766
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Mohamed Omar Yousif,1,2 Rania Serag Elkitkat,1,3– 5 Mohamed Nabil Hamza,1 Noha Abdelsadek Alaarag1
1Ophthalmology department, Faculty of Medicine, Ain Shams University, Cairo, Egypt; 2Maadi Eye Subspecialty Center, Cairo, Egypt; 3Watany Eye Hospital, Cairo, Egypt; 4Watany Research and Development Center, Watany Eye Hospital, Cairo, Egypt; 5Ophthalmology Department, Faculty of Medicine, MTI University, Cairo, Egypt
Correspondence: Rania Serag Elkitkat, Email [email protected]; [email protected]
Purpose: To evaluate the efficiency, safety, and stability of a revised tissue-saving treatment protocol in a cohort having pellucid marginal degeneration (PMD).
Methods: A retrospective cohort study was conducted on patients with PMD and no previous treatments. A revised protocol of topo-guided photorefractive keratectomy to be followed by customized phototherapeutic keratectomy and then corneal crosslinking was evaluated by comparing the pre and postoperative outcomes regarding visual (subjective refraction) and topographic (using data from Sirius CSO topography software) outcomes.
Results: There were both statistically significant and clinically relevant improvements in the postoperative parameters, where each of the unaided and corrected visual acuity, spherical equivalent, refractive cylinder, K readings, topographic cylinder, inferior minus superior difference at the 2- and 4- mm diameters, coma aberration, and higher order aberrations were significantly better postoperatively (all p values were less than 0.01, except for maximum k readings where the p-value was 0.017). The safety and efficacy indices for the surgical procedure were remarkably high (1.53 ± 0.70 and 0.90 ± 0.32, respectively).
Conclusion: Our proposed tissue-saving protocol (which showed satisfactory results in keratoconus cases according to a previously published article by our research team) has proven its successful outcomes (both topographically and visually) in cases of PMD, which is a rare ectatic entity with guarded prognosis using the available conventional ectasia treatment modalities.
Keywords: pellucid marginal degeneration, recent treatment options for PMD, combined PTK and CXL for PMD, tissue saving protocol for PMD treatment, revised cross-linking with PTK for PMD
Introduction
Pellucid marginal degeneration (PMD) is an uncommon, progressive, non-inflammatory corneal ectatic disorder with thinning of the inferior cornea in a crescent-shaped pattern.1 The corneal ectatic transformation occurs concentric with the inferior limbus and is separated from it by a distance of 1–3 mm.2 Tissue loss and crescentic stromal thinning leads to flattening of the vertical meridian, with paradoxical steepening at the horizontal meridian resulting in high values of against-the-rule astigmatism.3
PMD has been more commonly diagnosed in males than females, and no specific geographic distribution has been previously reported for the disease.4,5 Although a specific genetic inheritance has not been validated, high astigmatism in family members of patients having PMD has been reported.6
Unlike other inflammatory corneal thinning disorders, PMD is not associated with corneal stromal vascularization or lipid depositions, hence the name “pellucid” meaning “clear”.7 Furthermore, it has been considered a peripheral form of keratoconus (KC), with a “crab-claw”, “butterfly”, or “kissing doves” appearance on performing corneal topography.8 However, an inferior KC can topographically resemble a case of PMD, and a full limbal-to-limbal corneal thickness map is more distinctive to differentiate these 2 similar corneal ectatic conditions.1
Although recent corneal imaging has successfully differentiated PMD from KC, this differentiation did not differ much in the available treatment options, where there are multiple common treatment modalities, including spectacles for cylinder correction, hard contact lenses, corneal cross-linking (CXL), intracorneal ring segments (ICRS), or keratoplasty in advanced conditions. For almost two decades, CXL has been regarded as a mainstay treatment modality for both KC9,10 and PMD.11,12 Combined CXL and surface regularization of the cornea ensued afterward after Kanellopoulos and Binder introduced the Athens protocol, in which they combined both CXL and topography-guided photorefractive keratectomy (PRK).13,14 Similarly, marked visual and topographic improvements were reported for the combined PRK/CXL protocol in cases of PMD.15–18
Our research team has recently published a more tissue-saving revised protocol for managing various topographic types of KC,19 which starts by performing topography-guided PRK without epithelial removal, which is followed by customization of PTK treatment depth for each case that transmits the treatment to the corneal stroma in all the treated areas with minimal stromal ablation, and then CXL is performed. This customized PTK is attained by studying the PTK depth needed to remove the remaining epithelium at the area of minimal ablation after the application of a topo-guided treatment, then determining the PTK depth needed to remove that epithelium and hence transmission of treatment to the corneal stroma in all the treated areas. Our team has proven the efficacy, safety, and stability of the introduced revised protocol in a wide range of keratoconus patients, where the visual quality can be safely improved on a wider optical zone with the minimum possible stromal tissue removed, hence increasing the range of patients amenable to our proposed treatment protocol.
This study aimed to evaluate our revised protocol on a cohort of patients who had PMD, to determine whether the protocol can be efficiently and safely applied to such patients, or whether the results will not be as satisfactory as in cases of KC.
Materials and Methods
This retrospective cohort study was conducted using the electronic medical files of patients who had PMD and performed our revised protocol. All the patients sought medical advice at Maadi Eye Subspeciality Center, Cairo, Egypt. Surgeries were performed during the time interval from January 2019 to May 2023. The study abided by the tenets of the Declaration of Helsinki and was approved by the Ethical Committee of Ain Shams University (the registration code is FMASU-R197/2023). The institutional review board granted a waiver of informed consent owing to the study’s retrospective nature.
The study included cases of PMD with no previous treatments performed. The exclusion criteria comprised any anterior segment pathology other than PMD (mainly keratitis, corneal scars, glaucoma, or uveitis), posterior segment pathologies, and patients on long-term steroid intake or those having collagen vascular diseases (where corneal healing is expected to be compromised). Moreover, any severe cases of ectasia or cases with poor quality scans of their corneal topography that would affect the accuracy of topo-guided treatment were excluded from the study. If both eyes of the same patient conformed with the study criteria, the right eye was chosen to be enrolled.
The electronic medical files were explored to retrieve all the relevant patients’ data, including age, sex, laterality, pre and post-operative subjective refraction (including Uncorrected Distance Visual Acuity “UDVA” and Corrected Distance Visual Acuity “CDVA” using Snellen acuity chart, and the spherical equivalent and the cylinder of the performed treatment). Any documented postoperative complications were collected and analyzed.
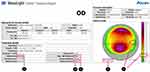
Regarding the laser treatment, data were obtained from the surgical planning printout of Contoura topography-guided ablation software of WaveLight EX500 excimer laser system (Alcon, USA). It included the maximum depth of the topo-guided treatment, the thickness of the removed epithelium (the depth of PTK), and the thinnest residual stromal bed thickness (all measured in microns). The maximum stromal ablation was then calculated by subtracting 50 microns (average epithelial thickness) from the sum of the topo-guided treatment maximum depth and the depth of PTK. Figure 1 illustrates the laser treatment screen showing the various parameters upon which the surgeon based the treatment protocol.
Regarding the corneal topography, data was obtained from the software of Sirius Topographer (CSO Italia) with software version Phoenix 3.2.1.60. The corneal thickness maps were well evaluated for the enrolled cohort of patients to ensure that all the cases were PMD rather than inferior KC, where a full limbal-to-limbal corneal thickness map evaluation was relied upon for reassuring PMD diagnosis rather than inferior KC. The data included in the study was the flattest corneal meridian (K1), steepest corneal meridian (K2), topographic cylinder, mean Keratometry (K mean), maximum Keratometry (K max), corneal thinnest location, corneal asphericity (Q value), pupil diameter, inferior minus superior keratometric difference at 2- and 4-mm diameters, and the root mean square (RMS) of coma aberration, spherical aberration, and higher order aberrations (HOAs).
The surgical procedure was done for all the enrolled participants by the same experienced surgeon (M.O.Y.). All the enrolled virgin corneas with PMD underwent topo-guided PRK at the beginning of the procedure before epithelial removal using WaveLight EX500 excimer laser system (Alcon, USA). This was followed by customized PTK (where the depth of laser treatment was tailored to each case after studying the topo-guided laser profile on the laser treatment screen) to transmit the laser treatment to the deeper stroma of the cornea at all the treated areas. In the end, CXL was done using the Avedro KXL System (Avedro Inc., USA). One second’s pulsed interval was used at a power of 30 mW/cm2 with an irradiation time of 4 minutes and a total treatment time of 8 minutes with a total energy delivered of 7.2 J/cm2. The details of the performed procedures and the methods adopted for maximal tissue saving while keeping a safe procedure are all detailed in our previously published work on KC patients.19
Noting that very high against-the-rule astigmatism was the main refractive component in most PMD patients, patients’ refraction that was chosen to be corrected with the topo-guided PRK was the highest cylinder that could be corrected without bypassing the cutoff points listed in our previously published paper for cases of KC.19 The topographic cylinder axis was chosen in the treatment profile for all cases even if it was not 100% coincident with the refractive cylinder axis.
The surgeon considered that cutoff values of 360 µm of minimal residual stromal thickness and a maximum stromal ablation depth of 70 µm were not to be exceeded for all cases. The 360 µm residual stromal bed was chosen to keep the efficacy of the CXL. We went beyond the classic 400 µm residual stromal depth. A similar protocol has already been published by Hafezi et al.20 We did not go beyond the 70µm ablation depth as we believe that this would have a higher risk of induced corneal haze. Three values were manipulated to design the treatment profile (PRK/PTK) that will not exceed the cutoff values, namely the treatment optical zone, the value of the treated corneal astigmatism, and the depth of PTK treatment.
Statistical Analysis
Data were collected, revised, coded, and entered into the Statistical Package for Social Science (IBM SPSS) version 23. The quantitative data were presented as mean, standard deviations, and ranges when parametric. Also, qualitative variables were presented as numbers and percentages. Comparisons between groups with qualitative data were made using the Chi-square test. Kolmogorov-Smirnoff test was used for checking data normality. Comparisons between two paired groups with quantitative data and parametric distribution were made using Paired t-test, while comparisons between two paired groups with quantitative data and non-parametric distribution were made using Wilcoxon signed-rank test. The confidence interval was set to 95% and the margin of error accepted was set to 5%. So, the p-value was considered significant if the p-value was <0.05.
Results
This study included 18 eyes of 18 patients who had PMD. The age had a mean ± SD of 35.72 years ± 4.07 (range of 29 to 40 years). The male-to-female percentage was 88.9% (16 eyes) to 11.1% (2 eyes), respectively, and 10 eyes were right while 8 eyes were left (percentage of 55.6% to 44%, respectively). The follow-up interval had a mean ± SD of 21.4 ± 13.2 months, with a range of 5 to 48 months.
Table 1 illustrates the details of the preoperative mean ± SD or median (IQR) of the patients’ treatment SE, cylinder, maximum treatment depth, the thickness of the removed epithelium, maximal stromal ablation, and the thinnest residual stromal bed.
The safety and efficacy indices of the revised protocol were calculated21 and showed high values of 1.53 ± 0.70 and 0.90 ± 0.32, respectively.
Table 2 and Table 3 demonstrate the pre and postoperative patients’ topographic indices and subjective refraction, respectively. The results declared both statistically significant and clinically relevant improvements in all the evaluated parameters (except for the spherical aberration). There were significant visual improvements in a considerable percentage of the cohort, where 66.6% of patients gained two lines or more postoperatively, and 33.3% either gained one line or kept a stable refraction postoperatively.
 |
Table 2 Comparisons Between the Pre and Postoperative Patients’ Topographic Indices Obtained from Sirius CSO Topography for the Enrolled Cohort Having Pellucid Marginal Degeneration |
 |
Table 3 Comparisons Between the Pre and Postoperative Subjective Refraction for the Enrolled Cohort Having Pellucid Marginal Degeneration |
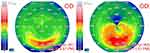
Figure 2 shows the pre and postoperative sagittal anterior curvature maps of Sirius CSO topography for a patient from the included cohort. The figure illustrates the marked topographic improvement in the curvature maps.
Regarding the detection of postoperative complications, two of the enrolled patients (with a percentage of 11.1%) experienced a relatively long period of delayed epithelial healing (more than 5 days). They were both treated with excessive topical lubricants and frequent changes of bandage contact lenses, and one of them needed the preparation of autologous serum. The latter patient developed prolonged, mild to moderate corneal haze for more than six months following the procedure. The haze was related to the persistent epithelial defect that took 19 days till complete healing. Although this patient developed delayed epithelial healing and some corneal haze, the electronic medical records showed that he still reported an improved visual quality postoperatively.
Discussion
In various medical fields, common entities of various diseases are always under the spotlight in research work, contrary to their rare counterparts which are always less frequently investigated owing to the sparsity of detected cases. This is the case for KC and its less common peripheral counterpart, namely PMD. The present study addressed a cohort of cases that had PMD and evaluated the efficacy, safety, and stability of a newly introduced revised tissue-saving protocol of management that was previously published by our research team19 with promising results for KC cases. This is the first report documenting its results for cases of PMD.
Although the available treatment options for both KC and PMD are almost similar, prognosis following either conservative or surgical procedures can vary in many instances. Fitting rigid scleral contact lenses is more difficult in cases of PMD due to the peripheral ectatic location.22 Corneal grafts are also more challenging and carry a higher rate of postoperative astigmatism as they require larger and more eccentric graft locations. ICRS is a competent way to address ectatic cases but requires a proper selection of candidates to avoid possible postoperative complications, especially in more advanced ectatic conditions and in the more peripheral cases of PMD.23 The more guarded prognosis for using ICRS in cases of PMD could be attributed to the fact that for the ring segment to flatten the horizontal steep corneal axis, it needs to be placed inferiorly on the flat corneal axis. This is a location that lies very close to the thinnest corneal location, which can increase the incidence of postoperative ring extrusion or migration, corneal thinning, or melting.
The protocol of CXL is undoubtedly a benchmark for managing cases of corneal ectasia with proven efficiency. It can slow down or even halt the ectatic progression by inducing an oxidation process that triggers the formation of corneal cross-links between the stromal collagen bundles.24,25
To date, a considerable number of case reports and case series studies have been published on patients having PMD who either performed CXL2,26,27 or combined PRK and CXL,15,16,18 where all the studies have shown satisfactory visual and topographic results postoperatively. Though CXL alone has been accepted as a sole treatment option for mild PMD cases with low astigmatism, cases with a high volume of against-the-rule astigmatism that exceeds the limits legible for correction by glasses or toric ICL represent a refractive challenge that necessitates having a more comprehensive solution to decrease the very high values of corneal astigmatism to levels that could be managed afterward, either conservatively with glasses or with toric ICL implantation (especially if associated with high spherical errors that failed to be corrected during the surgical procedure).
Our study results showed significant visual and topographic improvements in the evaluated cohort of patients. With high values of both efficacy and safety indices, and with a relatively long follow-up interval that reached up to 48 months, our proposed revised protocol of combined PRK to be followed by customized PTK then CXL can be successfully and safely used for cases of PMD. Because the protocol is a tissue-saving modality of treatment (where the stromal ablation depth could be maximally reduced and the residual stromal bed could be maximally preserved), it can significantly aid in enrolling a larger range of patients who were not suitable candidates for the classic Athens protocol (combined PTK and CXL) to benefit from this treatment modality.
As per the present study’s results, our revised tissue-saving protocol can be efficiently and safely used on a wide scale in cases of PMD, and it is not only successful in cases of KC as previously published.19 The included cohort of PMD cases ranged from mild to severe ectatic conditions (for instance, preoperative Kmax readings ranged from 48.54 to 64.92 D), and all the results were satisfactory from both topographic and visual aspects.
Our study reported a relatively long follow-up interval and included an acceptable number of PMD cases (considering the rarity of such cases). However, the major limitation of our study is its retrospective nature and that the cases were recruited from a single center in Cairo, Egypt. Although this private center receives cases from all over the Egyptian governorates, the study is still unicentric. Prospective multicentric studies on a larger scale of patients can further warrant the application of our revised protocol in cases of PMD. Besides, future longitudinal studies can more accurately detect patients’ postoperative satisfaction by subjectively evaluating their visual quality using contrast sensitivity evaluation and visual assessment questionnaires. Moreover, comparative studies with other available treatment options would more obviously elucidate the efficiency of the proposed protocol. We are also considering the implementation of a personalized epithelial thickness programming using anterior segment Optical Coherence Tomography, hoping for the providence of a better and more accurate picture of the corneal epithelium while planning the ablation profile.
Conclusions
The present study supports that our combined protocol of PRK to be followed by customized PTK then CXL can be an effective treatment option for cases of PMD. The promising results of the introduced protocol and the larger scale of patients to be included open a gateway for better prognosis in such a rare entity of corneal ectasia.
Data Sharing Statement
Available from the corresponding author upon reasonable request.
Ethics Approval and Informed Consent
The study was approved by the Ethical Committee of Ain Shams University (the registration code is FMASU-R197/2023). The institutional review board granted a waiver of informed consent owing to the study’s retrospective nature. Patients’ data were kept anonymous with utmost confidentiality.
Consent for Publication
All the material included in this paper can be published.
Acknowledgment
The authors would like to thank the statistician Mr. Hesham Elkady for the performance of the statistical analysis of the manuscript.
Author Contributions
All authors have made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis, and interpretation, or all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
There is no funding to report.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Lee BW, Jurkunas UV, Harissi-Dagher M, Poothullil AM, Tobaigy FM, Azar DT. Ectatic disorders associated with a claw-shaped pattern on corneal topography. Am J Ophthalmol. 2007;144(1):154–156. doi:10.1016/j.ajo.2007.02.032
2. Hassan Z, Nemeth G, Modis L, Szalai E, Berta A. Collagen cross-linking in the treatment of pellucid marginal degeneration. Indian J Ophthalmol. 2014;62(3):367–370. doi:10.4103/0301-4738.109523
3. Mamoosa B, Razmjoo H, Peyman A, Ashtari A, Ghafouri I, Moghaddam AG. The short-term result of collagen crosslinking in pellucid marginal degeneration. Adv Biomed Res. 2016;5(12):194. doi:10.4103/2277-9175.192732
4. Kompella VB, Aasuri MK, Rao GN. Management of pellucid marginal corneal degeneration with rigid gas permeable contact lenses. CLAO J. 2002;28(3):140–145.
5. Tzelikis PF, Cohen EJ, Rapuano CJ, Hammersmith KM, Laibson PR. Management of pellucid marginal corneal degeneration. Cornea. 2005;24(5):555–560. doi:10.1097/01.ico.0000153555.82278.5b
6. Taglia DP, Sugar J. Superior pellucid marginal corneal degeneration with hydrops. Arch Ophthalmol. 1997;115(2):274–275. doi:10.1001/archopht.1997.01100150276023
7. Sridhar MS, Mahesh S, Bansal AK, Nutheti R, Rao GN. Pellucid marginal corneal degeneration. Ophthalmology. 2004;111(6):1102–1107. doi:10.1016/j.ophtha.2003.09.035
8. Walker RN, Khachikian SS, Belin MW. Scheimpflug photographic diagnosis of pellucid marginal degeneration. Cornea. 2008;27(8):963–966. doi:10.1097/ICO.0b013e318170ae98
9. Males JJ, Viswanathan D. Comparative study of long-term outcomes of accelerated and conventional collagen crosslinking for progressive keratoconus. Eye. 2018;32(1):32–38. doi:10.1038/eye.2017.296
10. Aǧca A, Tülü B, Yasa D, et al. Accelerated corneal crosslinking in children with keratoconus: 5-year results and comparison of 2 protocols. J Cataract Refract Surg. 2020;46(4):517–523. doi:10.1097/j.jcrs.0000000000000101
11. Spadea L. Corneal collagen cross-linking with riboflavin and UVA irradiation in pellucid marginal degeneration. J Refract Surg. 2010;26(5):375–377. doi:10.3928/1081597X-20100114-03
12. Bayraktar S, Cebeci Z, Oray M, Alparslan N. Corneal collagen cross-linking in pellucid marginal degeneration: 2 patients, 4 eyes. Case Rep Ophthalmol Med. 2015;2015:840687. doi:10.1155/2015/840687
13. Kanellopoulos AJ, Binder PS. Collagen cross-linking (CCL) with sequential topography-guided PRK: a temporizing alternative for keratoconus to penetrating keratoplasty. Cornea. 2007;26(7):891–895. doi:10.1097/ICO.0b013e318074e424
14. Kanellopoulos AJ, Binder PS. Management of corneal ectasia after LASIK with combined, same-day, topography-guided partial transepithelial PRK, and collagen cross-linking: the Athens protocol. J Refract Surg. 2011;27(5):323–331. doi:10.3928/1081597X-20101105-01
15. Kymionis GD, Karavitaki EA, Kounis GA, Portaliou DM, Yoo SH, Pallikaris IG. Management of pellucid marginal corneal degeneration with simultaneous customized photorefractive keratectomy and collagen crosslinking. J Cataract Refract Surg. 2009;35(7):1298–1301. doi:10.1016/j.jcrs.2009.03.025
16. Stojanovic A, Zhang J, Chen X, Nitter TA, Chen S, Wang Q. Topography-guided transepithelial surface ablation followed by corneal collagen cross-linking performed in a single combined procedure for the treatment of keratoconus and pellucid marginal degeneration. J Refract Surg. 2010;26(2):145–152. doi:10.3928/1081597X-20100121-10
17. Kymionis GD, Grentzelos MA, Plaka AD, et al. Simultaneous conventional photorefractive keratectomy and corneal collagen cross-linking for pellucid marginal corneal degeneration. J Refract Surg. 2014;30(4):272–276. doi:10.3928/1081597X-20140320-06
18. Cagil N, Sarac O, Yesilirmak N, Caglayan M, Uysal BS, Tanriverdi B. Transepithelial phototherapeutic keratectomy followed by corneal collagen crosslinking for the treatment of pellucid marginal degeneration: long-term results. Cornea. 2019;38(8):980–985. doi:10.1097/ICO.0000000000002003
19. Yousif MO, Elkitkat RS, Edrees ES, Alaarag NA. Introducing a revised tissue saving protocol for combined topography-guided photorefractive keratectomy and cross-linking in keratoconic corneas. Cornea. 2023;42(6):755–765. doi:10.1097/ICO.0000000000003225
20. Hafezi F, Kling S, Gilardoni F, et al. Individualized Corneal Cross-linking With Riboflavin and UV-A in Ultrathin Corneas: the Sub400 Protocol. Am J Ophthalmol. 2021;224(4):133–142. doi:10.1016/j.ajo.2020.12.011
21. Gomel N, Negari S, Frucht-Pery J, Wajnsztajn D, Strassman E, Solomon A. Predictive factors for efficacy and safety in refractive surgery for myopia. PLoS One. 2018;13(12):e0208608. doi:10.1371/journal.pone.0208608
22. Rathi VM, Dumpati S, Mandathara PS, Taneja MM, Sangwan VS. Scleral contact lenses in the management of pellucid marginal degeneration. Cont Lens Anterior Eye. 2016;39(3):217–220. doi:10.1016/j.clae.2015.11.005
23. Bautista-Llamas MJ, Sánchez-González MC, López-Izquierdo I, et al. Complications and explantation reasons in Intracorneal Ring Segments (ICRS) implantation: a systematic review. J Refract Surg. 2019;35(11):740–747. doi:10.3928/1081597X-20191010-02
24. Nobari S, Villena C, Jadidi K. Myoring implantation alone versus corneal collagen crosslinking following Myoring implantation for management of keratoconus: 1-year follow-up. Acta Med Mediterr. 2016;32(2):1077.
25. Alio JL, Vega-Estrada A, Esperanza S, Barraquer RI, Teus MA, Murta J. Intrastromal corneal ring segments: how successful is the surgical treatment of keratoconus? Middle East Afr J Ophthalmol. 2014;21(1):3–9. doi:10.4103/0974-9233.124076
26. Koller T, Schumacher S, Fankhauser F, Seiler T. Riboflavin/ultraviolet a crosslinking of the paracentral cornea. Cornea. 2013;32(2):165–168. doi:10.1097/ICO.0b013e318269059b
27. Pilcher N, Lammer J, Holzer S, Gschließer A, Schmidinger G. Corneal crosslinking for pellucid marginal degeneration. J Cataract Refract Surg. 2019;45(8):1163–1167. doi:10.1016/j.jcrs.2019.03.018
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.