Back to Journals » Clinical, Cosmetic and Investigational Dermatology » Volume 16
Application Effect of Modified Through and Through Suture in Anterior Chondrectomy of Auricular Pseudocyst
Authors Tian C , Xie W, Chen L, Liu X, Hao Z
Received 21 December 2022
Accepted for publication 24 February 2023
Published 28 February 2023 Volume 2023:16 Pages 537—543
DOI https://doi.org/10.2147/CCID.S401509
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Anne-Claire Fougerousse
Chunhui Tian, Weipin Xie, Lifang Chen, Xuebao Liu, Zhongping Hao
Department of Otorhinolaryngology Head and Neck Surgery, Suzhou Hospital Affiliated to Anhui Medical University, Suzhou, People’s Republic of China
Correspondence: Chunhui Tian, Department of Otorhinolaryngology Head and Neck Surgery, Suzhou Hospital Affiliated to Anhui Medical University, 299 Bianhe Road, Suzhou, 234000, People’s Republic of China, Tel +86 18405576337, Email [email protected]
Objective: To introduce a novel method of modified through and through suture with collagen sutures in conjunction with anterior chondrectomy of auricular pseudocyst and assess its therapeutic efficacy.
Subjects and Methods: The study comprised 87 patients with unilateral auricular pseudocyst, treated in our department from December 2019 to November 2021. Following anterior chondrectomy of the cyst, modified through and through suture was performed using collagen sutures. Evaluation of successful resolution of the problem, assessment of complications, recurrence, and ultimate ear cosmesis was undertaken with a minimum of 6 months follow-up.
Results: There were 83 males and 4 females, ages ranged from 26– 78 years old, with a median age of 41 years. The right and left ears were affected in, 52 and 35 patients, respectively. Local skin color deepening was found in 15 patients within 3 months, which returned to normal within 5 months. During the follow-up, such complications as anaphylaxis, hematocele in the surgical cavity, incision infection, and deformity were not observed in any patients. All patients were cured with a single operation without relapse.
Conclusion: The modified through and through suture with collagen sutures in conjunction with anterior chondrectomy of an auricular pseudocyst is characterized by a straightforward, single-stage operation, with no relapses, few complications, restoration of normal ear cosmesis, and high patient acceptance.
Keywords: auricle pseudocyst, anterior resection, modified suture, management
Introduction
As a benign lesion typically located in the upper half of the anterior ear cartilage, an auricular pseudocyst is pathophysiologically manifested as a sterile, intercartilaginous serous fluid-filled cavity without epithelial lining. Its pathogenesis has not been fully clarified but has been postulated to result from local trauma.1 The cystic mass is often filled with yellowish or colourless fluid. Treatment has evolved from simple aspiration or incision and drainage which almost inevitably caused reaccumulation, to aspiration combined with pressure dressing, local steroid injection, and anterior chondrectomy.2–4 Specifically, anterior chondrectomy has been favored by surgeons due to a low recurrence rate using a straightforward, curative operation.2,5 Nevertheless, the development of postoperative hematocele-induced complications such as infection, swelling, and auricular deformity often occur.2,3 To address this problem, fixation with such materials as splints,6 rubber sheets,5 buttons,7,8 and plastic sheets9 have been employed following anterior chondrectomy, achieving some beneficial effects. However, these methods have added a somewhat complicated step, requiring postoperative return visits, yet they have been unable to completely avoid some complications. In our department, “through-and-through” collagen sutures have been used following anterior chondrectomy to close and obliterate the potentially dead space of the excised pseudocyst. The intent of the present study was to review the short and medium-term follow-up results of this treatment, specifically with regard to recurrence, complications and ultimate cosmetic outcome.
Materials and Methods
This retrospective study comprised 87 patients with unilateral auricular pseudocysts who were operatively treated at Suzhou Hospital of Anhui Medical University from December 2019 to November 2021. The exclusion criteria were as follows: 1) patients with preoperative local infection, 2) those with severe hematological diseases, and 3) those with simultaneous critical illness. An informed valid and written consent was obtained from all patients, and patients whose photographs were used provided informed consent for the images to be published. This study was approved by the Human Ethical Committee of Suzhou Hospital Affiliated to Anhui Medical University and was conducted according to the Declaration of Helsinki.
Surgical Procedure
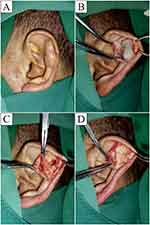
The patient was in a supine position with the affected ear facing upwards, and a drape was placed after local disinfection (Figure 1A). The external auditory canal, posterior sulcus of the auricle, and cyst surface were locally anesthetized using 2% lidocaine hydrochloride combined with 1:100,000 epinephrine. An arcuate incision was made at the fold of the helix closest to the cyst in a straight-line (or at the anthelix closest to the cyst if the cyst was located in the cavity of auricular concha), and the skin overlying the anterior wall of the pseudocyst was dissected slightly beyond the cyst margins (Figure 1B). Thereafter, the cyst was opened to completely expose the cyst cavity, the cyst fluid was aspirated, and the anterior wall cartilage was completely excised (Figures 1C and D). The cartilaginous surface of the posterior wall was moderately abraded with dry gauze, bleeding from the anterior wall skin and incision were controlled with careful bipolar electrocoagulation forceps, and the surgical cavity was thoroughly flushed with Entoiodine and normal saline. The anterior wall skin was replaced overlying the posterior cartilaginous surface and sutured as follows. The full-thickness auricle was sutured with through and through suture using a 5–0 collagen suture (Boda®, Shandong, China). Briefly, after being straightened, the needle was passed full-thickness through the auricle from posterior to anterior, then passed from anterior to posterior, approximately 2 mm from the initial penetration point. This continuous suture was repeated at 2–5 points throughout the cartilaginous base, as determined by the size and location of the cyst. The suture closure was completed by tying a knot behind the auricle (Figures 2A and B). Bandaging was not required, but chlortetracycline hydrochloride eye ointment was externally applied daily to all sutures until they were absorbed or completely detached (Figures 2C and D). In addition, oral antibiotics were administered for 3–5 days after surgery, but analgesics were not required. All patients were followed up for a minimum of 6 months.
Results
There were 83 males and 4 females, ranging in age from 26–78 years old, (mean, 41 years). The most commonly affected age group was 31–40 years with 29 (33.3%) patients (Table 1). Lesions affected the right ear of 52 patients, and the left ear of 35 patients and involved the scaphoid fossa (60.9%) in most cases (Table 2). The preoperative course of disease extended from 7–38 days, and 16 patients had a clear history of local trauma or bruises, and 22 patients had relapsed after prior puncture treatment.
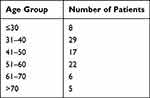 |
Table 1 Age Distribution of the Patients (n=87) |
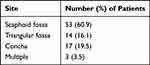 |
Table 2 Sites of Involvement (n=87) |
All 87 patients were cured with the single-stage operative procedure, with no recurrences. Mild deepening of local skin color was noted in 15 patients within 3 months, which returned to normal within 5 months. With a minimum of 6 months follow-up, none of the patients suffered complications such as anaphylaxis, hematocele in the surgical cavity, auricular infection, or auricular deformity.
Discussion
In 1966, Engel reported auricular pseudocyst for the first time, which he described as an endochondral cystic lesion, and described its pathological structure.10 It was characterized by a cystic cavity filled with sterile fluid and no epithelial tissue.11 The inciting event has been attributed to cartilage contusion or local circulatory disturbance after mechanical stimulation of the auricle; it also may have an association with such factors as immune abnormalities or congenital dysplasia of the auricle.1,4,5,8 In a pathological study of the resected anterior cartilage conducted by Zhang et al, the outer wall of the early auricular pseudocyst was actually the diseased perichondrium, which subsequently developed into new cartilage, and the whole cartilage was formed following continuous proliferation and thickening of the new cartilage,12 rendering a theoretical basis for the low recurrence rate after anterior chondrectomy.
In the present study, the scaphoid fossa was found to be the most common site of involvement (60.9%), in line with the findings of Lee et al.11 The possible reason is that the scaphoid fossa is closer to the edge of the auricle and relatively more vulnerable to injuries. The incidence rate was slightly higher in the right auricle (59.8%) than that in the left auricle, in keeping with the findings of studies carried out by Wu et al5 and Kanotra et al.8 An auricular pseudocyst has been unilateral in most cases, with bilateral auricular pseudocyst rarely reported, and it has shown a higher incidence rate in males than females,1,4,5 consistent with our incidence rate of 95.4% males.
The treatment of auricular pseudocyst aims to restore the normal anatomical morphology and cosmetic appearance of the auricle and prevent a recurrence. Even at the present time, minimally invasive therapeutic methods are commonly used, including physical therapy, aspiration of cyst fluid, and plaster compression.2,3 Moreover, a steroid injection is also commonly employed.2,4 However, these therapeutic methods have notable shortcomings. For example, about 30% of patients require repeated treatment and 10% of patients have varying degrees of skin thickening, as reported by Parajuli et al.4 Kanotra et al reported that the recurrence rate even reached 96.6% following the initial puncture treatment.8 Beutler et al cautioned that steroid injection may lead to permanent auricular deformity, and it should not be recommended as first-line therapy.4 Lee et al admonished that suppurative perichondritis of the auricle in 32% of patients could be attributed to inappropriate treatment of auricular pseudocyst.11 Therefore, even though seemingly simpler, less invasive management clearly has the potential for subsequent development of auricular infection, or even severe permanent auricular deformity.1,3
Studies have confirmed that the hydrops in pseudocysts is derived from the anterior wall cartilage, and the source of serous effusion is removed following resection of the anterior wall cartilage, thereby logically ensuring a high success rate.8,11 In addition, anterior chondrectomy results in good cosmesis with consequent high patient satisfaction rates, making it the preferred choice for the treatment of auricular pseudocyst.2,13 However, after anterior chondrectomy, the ventral surface of the auricle becomes uneven and a pressure bandage may not ensure complete prevention of dead space until final healing occurs. As a result, re-filling the dead space with a hematocele may compromise an initially excellent operative procedure. This is also the leading cause of postoperative infection and scar hyperplasia.
Direct through and through suture of the surgical area with collagen sutures following anterior chondrectomy provides a solution to this problem, eliminating the dead space and avoiding the development of a hematocele in the surgical cavity. The reports on this approach are few currently. Collagen sutures are prepared from highly purified type I collagen, which can be catalyzed by human collagenase into endogenous amino acids that can be reused by the body, with little rejection and good histocompatibility.14,15 Previous studies have demonstrated that collagen has good plasticity and fiber forming property, and can also promote platelet aggregation and enhance local blood coagulation ability, thus reducing the oozing of the blood.14,16 As a vital part of the skin, collagen stimulates the proliferation of immune cells and fibroblasts, reduces the content of matrix metalloproteinases, preserves the extracellular matrix structure, and facilitates tissue healing, thereby shortening the healing time of incisions.17,18 Collagen can be completely absorbed within 5–8 days after surgery, with the degradation time basically consistent with the healing time of hypotonic skin incisions, and the residual sutures will detach spontaneously, avoiding suture removal. For these reasons, collagen sutures have been widely applied in the suture of Class I and II incisions in the clinic, with satisfactory results.
Several important technical points of the operation deserve special emphasis. The thin layer of skin anterior to the perichondrium should be dissected close to the perichondrium so as to maximize its integrity and local blood supply. The anterior wall cartilage is uneven in thickness, so the cyst cavity should be opened after the anterior wall skin has been dissected somewhat beyond the margins of the pseudocyst, to avoid retained cartilage residues. To reduce the risk of hematocele in the surgical cavity, meticulous hemostasis of the anterior wall skin and incision must be complete but delicately achieved with bipolar electrocoagulation forceps adjusted to low power. When performing through and through suture, the number of points selected for suture should not be excessive. Generally, 2–5 points are selected for suture in the key position of shaping, with a distance between the withdrawal point and the penetrating point of about 2 mm. This suture method makes the anterior skin fit well on the posterior cartilage, eliminates dead space, and ensures the blood supply. A closed loop should be avoided on the anterior skin, which could lead to local skin ischemia, or even skin necrosis and infection. However, there is no special requirement for the posterior suture pattern since the posterior skin is not separated during surgery and the skin itself is thick with a good blood supply.
Many clinicians may worry that through and through suture, in which the auricular cartilage is directly passed through for suture, will increase the risk of auricular cartilage infection. According to existing studies, no severe anaphylaxis has been found.5,7–9 Genç et al applied tamponade and through and through suture after simulated nasal septal surgery in rabbits and carried out pathological reviews on the cartilage and mucosa of rabbits 6 weeks later. They discovered that the relevant inflammatory parameters and cartilage thickness were comparable between the two groups of specimens.19 At present, no similar basic studies on the auricle have been conducted. The results of this study, however, revealed that the through and through suture did not lead to additional damage to the auricle.
Conclusion
The critical final step in the treatment of auricular pseudocyst is the elimination of dead space. The use of modified through and through suture with collagen sutures obliterates the dead space, permits restoration of normal ear cosmesis, prevents complications that could develop with fluid accumulation in the surgical cavity, and prevents cyst recurrence with a single operation. With appropriate attention to technical detail, this technique is safe, effective, fully addresses the underlying pathology, and is very patient-friendly.
Acknowledgments
The authors thank Prof Mingliang Wang from Suzhou University for his assistance in sorting the pictures. Thanks also to Dr. Renwu Zhao and Dr. Qin Wang from the First Affiliated Hospital of Anhui Medical University for their assistance in the process of writing this paper. Thanks to their colleagues who were involved in the treatment of the patients. None of the material related to this manuscript has been published or is under consideration for publication elsewhere.
Author Contributions
All authors made a significant contribution to the work reported, whether it was in the conception, study design, execution, acquisition of data, analysis and interpretation, or more than one of these areas; took part in drafting, revising or critically reviewing the study; gave final approval of the version to be published; agreed on the journal to which the article was submitted; and agreed to be accountable for all aspects of the work.
Funding
This work was funded by the Suzhou Science and Technology Program (Grant No.: SZ2020GG09). The study sponsor was not involved in performing the research or in writing the paper.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Beutler BD, Cohen PR. Pseudocyst of the auricle in patients with movement disorders: report of two patients with ataxia-associated auricular pseudocysts. Dermatol Pract Concept. 2015;5(4):59–64. doi:10.5826/dpc.0504a15
2. Yu J, Lu Y, Yu Q, Guan B, Chen C, Yu S. Comparison and evaluation of three techniques for treating auricular pseudocyst. J Dermatolog Treat. 2022;33(1):494–497. doi:10.1080/09546634.2020.1770169
3. Liu L, Gao T, Wang Z. Anterior wall resection plus radiofrequency ablation versus simple aspiration in the treatment of auricular pseudocyst: a retrospective study. J Int Med Res. 2020;48(9):300060520950930. doi:10.1177/0300060520950930
4. Parajuli R, Kshetry J. Treatment of Auricular Pseudocyst with Intralesional Steroid: a Study with Short-Term Follow-Up. Clin Cosmet Investig Dermatol. 2020;13:579–585. doi:10.2147/CCID.S264755
5. Wu MY, Chen CB, Chen YH, Chang C, Chan KC. Sandwich compression with rubbery tourniquet sheets and cotton balls for auricular pseudocyst. Laryngoscope. 2018;128(7):1653–1657. doi:10.1002/lary.26884
6. Rao K, Jagade M, Kale V, Kumar D, Hekare A. An Economical Method of Auricular Splinting in Management of Auricular Pseudocyst. World J Plast Surg. 2018;7(2):220–225.
7. Göktay F, Aslan C. Successful treatment of auricular pseudocyst with clothing button bolsters alone. J Dermatolog Treat. 2011;22(5):285–287. doi:10.3109/09546631003762662
8. Kanotra SP, Lateef M. Pseudocyst of pinna: a recurrence-free approach. Am J Otolaryngol. 2009;30(2):73–79. doi:10.1016/j.amjoto.2008.02.008
9. Shan Y, Xu J, Cai C, Wang S, Zhang H. Novel modified surgical treatment of auricular pseudocyst using plastic sheet compression. Otolaryngol Head Neck Surg. 2014;151(6):934–938. doi:10.1177/0194599814549528
10. Engel D. Pseudocysts of the auricle in Chinese. Arch Otolaryngol. 1966;83(3):197–202. doi:10.1001/archotol.1966.00760020199003
11. Lee YJ, Kwon JG, Han HH. Surgical deroofing in the treatment of patients with auricular pseudocyst. Auris Nasus Larynx. 2019;46(4):576–582. doi:10.1016/j.anl.2018.10.017
12. Zhang XT, Sun B, Ling Y, et al. Investigation of clinical pathology and treatments on the auride pseudocyst. Chin J Otorhinolaryngol Head Neck Surgery. 2010;45:640–644.
13. Ungar OJ, Oron Y, Cavel O, et al. Case Series and Systematic Review of Treatment Outcomes for Auricular Pseudocysts. Otol Neurotol. 2021;42(5):774–782. doi:10.1097/MAO.0000000000003036
14. Shahidi M. Thrombosis and von Willebrand Factor. Adv Exp Med Biol. 2017;906:285–306. doi:10.1007/5584_2016_122
15. Byrne M, Aly A. The Surgical Suture. Aesthet Surg J. 2019;39(Suppl_2):S67–S72. doi:10.1093/asj/sjz036
16. Younesi M, Donmez BO, Islam A, Akkus O. Heparinized collagen sutures for sustained delivery of PDGF-BB: delivery profile and effects on tendon-derived cells In-Vitro. Acta Biomater. 2016;41:100–109. doi:10.1016/j.actbio.2016.05.036
17. Kallis PJ, Friedman AJ. Collagen Powder in Wound Healing. J Drugs Dermatol. 2018;17(4):403–408.
18. Ricci E, Cutting KF. Evaluating a native collagen matrix dressing in the treatment of chronic wounds of different aetiologies: a case series. J Wound Care. 2016;25(11):670–678. doi:10.12968/jowc.2016.25.11.670
19. Genç E, Ergin NT, Bilezikçi B. Comparison of suture and nasal packing in rabbit noses. Laryngoscope. 2004;114(4):639–645. doi:10.1097/00005537-200404000-00008
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.