Back to Journals » Clinical Ophthalmology » Volume 17
Anti-Vascular Endothelial Growth Factor Therapy with or Without Initial Steroid Therapy for Macular Edema in Branch Retinal Vein Occlusion
Authors Noma H, Yasuda K, Nonaka R, Sasaki S, Shimura M
Received 26 April 2023
Accepted for publication 20 July 2023
Published 9 August 2023 Volume 2023:17 Pages 2267—2275
DOI https://doi.org/10.2147/OPTH.S418843
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Scott Fraser
Hidetaka Noma, Kanako Yasuda, Ryota Nonaka, Shotaro Sasaki, Masahiko Shimura
Department of Ophthalmology, Hachioji Medical Center, Tokyo Medical University, Tokyo, Japan
Correspondence: Hidetaka Noma, Department of Ophthalmology, Hachioji Medical Center, Tokyo Medical University, 1163, Tatemachi, Hachioji, Tokyo, 193-0998, Japan, Tel + 81-42-665-5611, Fax + 81-42-665-1796, Email [email protected]
Purpose: In branch retinal vein occlusion (BRVO), administering steroid injections to inhibit expression of inflammatory factors in the first phase of macular edema may reduce recurrence of the edema. The purpose of our study was to investigate the functional and morphological prognosis and frequency of recurrence after injection of an anti-vascular endothelial growth factor (VEGF) with and without initial steroid therapy to treat macular edema with BRVO.
Patients and Methods: Patients with BRVO and macular edema (41 eyes) received intravitreal ranibizumab injection (IRI) alone (IRI group, 21 eyes) or subtenon triamcinolone (STTA) injection and IRI (combination group, 20 eyes). Patients in both groups with recurrent macular edema received further IRI as appropriate. A laser flare meter was used to assess aqueous flare values, and an optical coherence tomography device was used to measure central macular thickness (CMT). Before the first treatment, we obtained samples of aqueous humor and analyzed them by the suspension array method to evaluate VEGF, placental growth factor (PlGF), platelet-derived growth factor (PDGF)-AA, soluble intercellular adhesion molecule (sICAM)-1, monocyte chemoattractant protein 1 (MCP-1), interleukin (IL)-6, IL-8, and interferon-inducible 10-kDa protein (IP-10).
Results: The two groups were not significantly different with regard to levels of VEGF, PlGF, PDGF-AA, sICAM-1, MCP-1, IL-6, IL-8, or IP-10. Best-corrected visual acuity, CMT, and aqueous flare value (IRI group, baseline 8.69 ± 4.55 photon counts/ms; combination group, baseline 9.21 ± 3.72 photon counts/ms) improved significantly in both groups without significant intergroup differences. Analyses showed no significant intergroup differences in the mean number of IRIs during the 12-month follow-up, but the proportion of patients without recurrence (ie, who received only one IRI) was significantly higher in the combination group than in the IRI group (P = 0.032). Furthermore, the time to initial recurrence was significantly longer in the combination group than in the IRI group (P = 0.003).
Conclusion: These findings suggest that initial STTA injection and IRI may have a synergistic effect in patients with BRVO and macular edema in that they increase the time between anti-VEGF treatments.
Keywords: branch retinal vein occlusion, macular edema, ranibizumab, subtenon triamcinolone, recurrence, cytokine
Introduction
One of the most common retinal disorders in older individuals is branch retinal vein occlusion (BRVO), which affects vision and causes retinal hemorrhage and macular edema.1 BRVO is caused by proximal branch retinal vein thrombosis, which causes venous engorgement and stasis in the affected retinal quadrant. Untreated macular edema causes permanent visual impairment in two out of three patients, but anti-VEGF agents were developed as a treatment after studies showed that macular edema in BRVO involves overexpression of vascular endothelial growth factor (VEGF).1–3
After the initial treatment with an anti-VEGF agent, the majority of patients with BRVO experience recurrence of macular edema at some time, although the associated mechanisms remain unclear. Previously, we reported that inflammatory factors are increased in patients with recurrent macular edema and BRVO4 and that the number of recurrences of macular edema is significantly correlated with the baseline levels of inflammatory factors.5 These findings suggest that inhibiting expression of inflammatory factors by administering steroid injections in the first phase of macular edema may reduce recurrence. Recent meta-analyses found superiority of intravitreal anti-VEGF agents over steroids in the treatment of macular edema secondary to BRVO with regards to visual acuity, anatomic outcomes, and safety endpoints.6,7 In light of this finding, we felt it was important to study functional and morphological prognosis, frequency of recurrence, and aqueous flare values after injection of an anti-VEGF agent with or without initial steroid therapy for macular edema associated with BRVO because inhibiting expression of inflammatory factors by administering steroid injections in the first phase of macular edema may reduce inflammation and recurrence of macular edema. Accordingly, we investigated functional and morphological prognosis, frequency of recurrence, and aqueous flare values after injection of an anti-VEGF agent with or without initial steroid therapy for macular edema associated with BRVO.
Methods
Subjects
This retrospective study was conducted at the Department of Ophthalmology at the Tokyo Medical University Hachioji Medical Center. From October 2017 through October 2019, patients with BRVO and macular edema (41 eyes) received intravitreal ranibizumab injection (IRI; 0.5 mg in 0.05 mL, Lucentis, Novartis, Buläch, Switzerland) alone (IRI group, 21 eyes) or initial subtenon triamcinolone acetonide (STTA) injection followed by IRI (combination group, 20 eyes). No loading dose was used. Patients with subsequent recurrence of macular edema received further IRI treatment pro re nata. Recurrence of macular edema was defined as an increase of foveal thickness by more than 100 µm compared to the value after the initial IRI treatment if the thickness had decreased to less than 300 µm at least once after the initial treatment.
Patients were treated by IRI if their central macular thickness (CMT) was more than 300 μm and their best corrected visual acuity (BCVA, reported as the logarithm of the minimum angle of resolution [LogMAR]) was below 25/30. All patients were treatment naive. Because IRI treatment was administered pro re nata, a full eye examination and optical coherence tomography (OCT) were performed every month for 12 months, and IRI was repeated if CMT was above 300 μm. The criterion for reinjection was prolonged macular edema or recurrence of CMT greater than 300 μm.8 As an index of intraocular inflammation, laser flare was measured with a laser flare meter (FC-600, Kowa Co. Ltd., Tokyo, Japan) according to a previously published method.9
Patients were excluded if their medical history included any of the following conditions: glaucoma, uveitis, other retinal disease or retinal ischemia (ischemic type), type 1 or type 2 diabetes, diabetic retinopathy, rubeosis iridis, and eye infection. Additional exclusion criteria were previous treatment by laser photocoagulation; cataract or other intraocular surgery; and intravitreal injection of an anti-VEGF agent or triamcinolone acetonide.
A measurement of high blood pressure was defined as systolic pressure of at least 140 mm Hg and diastolic pressure above 90 mm Hg at the same examination; systolic pressure of at least 140 mm Hg on one day and diastolic pressure above 90 mm Hg on another day; or use of antihypertensive drugs. Hyperlipidemia was defined as the presence of one of the following: cholesterol, at least 240 mg/dL; triglycerides, at least 160 mg/dL; low-density lipoprotein cholesterol, at least 130 mg/dL; or use of statins or other cholesterol-lowering drugs. Intraocular pressure (IOP) was measured monthly, and the current World Health Organization Simplified Cataract Grading System was used to rate nuclear, posterior subcapsular, and cortical cataracts; cataract was defined as a grade of II.
The ethics committee of Tokyo Medical University Hachioji Medical Center approved the study (approval no. T2022-0174), which was performed in accordance with the principles defined in the Declaration of Helsinki.
Fundus Findings
At baseline, ophthalmoscopy and slit-lamp and fundus contact lens examinations were performed, together with standard fundus color photography and fluorescein angiography with a Topcon TRC-50EX fundus camera (Tokyo Optical Co. Ltd., Tokyo, Japan), a preset lens and slit lamp, and a Topcon IMAGEnet system (Tokyo Optical Co. Ltd.). Fluorescein angiography was performed to confirm the degree of ischemia (particularly severe ischemia) and the degree of vascular hyperpermeability.
Patients were examined by spectral domain OCT (Spectralis, Heidelberg Engineering, Heidelberg, Germany) in the week before IRI and CMT was calculated by measuring the distance between the inner limiting and basal membrane of the retinal pigment epithelium (including all intermediary compartments). Two retinal specialists, who were blind to BCVA and cytokine values, measured CMT with calipers linked to the software of the Spectralis device.
Treatment with IRI and STTA Injection
Oxybuprocaine eye drops 0.4% (Benoxil; Santen Pharmaceutical, Osaka, Japan) were administered to the eye 3 times or more for topical anesthesia. The combination group received 20 mg triamcinolone acetonide (Kenacort; Bristol-Myers Squibb, Tokyo, Japan) administered as a 0.5 mL transconjunctival subtenon injection into the superotemporal quadrant by using a 21-gauge tri-port subtenon cannula (Eagle Lab, Rancho Cucamonga, CA, USA).
Immediately after the STTA injection, the first IRI was administered. At that time, a 30-gauge needle attached to an insulin syringe was used to obtain 0.1 mL of aqueous humor (mean value) from the anterior chamber by limbal paracentesis; the samples were subsequently stored in sterile plastic tubes at −80°C until the time of analysis. Then, IRI was performed at a distance of 3.5 mm from the limbus through the pars plana. After IRI, eyes were treated for 3 days with antibiotic eye drops.
The same retinal specialist (H. N.) performed all injections and confirmed the absence of a drug reflex (ie, reflux by injection) every time.
Cytokine and Growth Factor Measurements
Suspension array assay (xMAP; Luminex Corp. Austin, TX) was used to evaluate aqueous humor samples.10 VEGF, placental growth factor (PlGF), soluble intercellular adhesion molecule (sICAM)-1, monocyte chemoattractant protein 1 (MCP-1), platelet-derived growth factor (PDGF)-AA, interleukin (IL)-6, IL-8, and interferon-inducible 10-kDa protein (IP-10) were detected with Beadlyte capture bead kits (Upstate Biotechnology, Lake Placid, NY) according to the manufacturer’s instructions in 25 μL of undiluted aqueous humor samples after incubation in a dark room at room temperature for 2 hours or, in the case of PlGF and sICAM1, for 16 to 18 hours (overnight). The reference cytokine concentrations in the measurement kits were used to create duplicate cytokine standard curves. All samples from a patient, ie, from before and after IRI, were analyzed in the same run to avoid potential run-related heterogeneity and compared with the reference curves. All factors were at high enough levels to be detected (minimum detectable concentrations: VEGF, 0.64 pg/mL; PlGF, 0.37 pg/mL; sICAM-1, 0.03 ng/mL; MCP-1, 1.2 pg/mL; PDGF-AA, 0.64 pg/mL; IL-6, 0.29 pg/mL; IL-8, 0.14 pg/mL; and IP-10, 0.55 pg/mL).
Statistical Analysis
We used SAS System 9.4 software (SAS Institute Inc., Cary, North Carolina, USA) to analyze data. Results are shown as means ± SD or frequencies. Differences between the IRI and combination groups were assessed by Student’s t test and Chi-squared test. One- or two-way repeated measures analysis of variance (ANOVA) was used to evaluate changes in BCVA, CMT, aqueous flare values, and IOP. Statistical significance was assumed for two-tailed P values below 0.05.
Results
The characteristics of the IRI and combination groups are summarized in Table 1. The baseline aqueous flare value was 8.69 ± 4.55 (photon counts/ms) in the IRI group and 9.21 ± 3.72 in the combination group. We found no significant differences between the two groups with respect to the mean age (P = 0.793), ratio of women to men (P = 0.272), prevalence of high blood pressure measurements (P = 0.929), prevalence of hyperlipidemia (P = 0.878), duration of macular edema (P = 0.403), baseline BCVA (P = 0.684), BCVA at 12 months (P = 0.946), baseline CMT (P = 0.679), CMT at 12 months (P = 0.820), or baseline aqueous flare value (P = 0.687; Table 1). The levels of cytokines and growth factors in the IRI Group were as follows: VEGF, 94.2 ± 70.4 pg/mL; PlGF, 8.19 ± 9.21 pg/mL; PDGF-AA, 18.2 ± 4.85 pg/mL; sICAM-1, 36.7 ± 72.8 ng/mL; MCP-1, 2611 ± 1141 pg/mL; IL-6, 13.2 ± 15.5 pg/mL; IL-8, 28.9 ± 21.5 pg/mL; and IP-10, 193 ± 67.5 pg/mL. In the combination group, the levels were as follows: VEGF, 91.8 ± 64.7 pg/mL; PlGF, 6.44 ± 6.09 pg/mL; PDGF-AA, 15.9 ± 3.32 pg/mL; sICAM-1, 25.7 ± 27.1 ng/mL; MCP-1, 2238 ± 828 pg/mL; IL-6, 10.3 ± 7.46 pg/mL; IL-8, 29.7 ± 28.7 pg/mL; and IP-10, 148 ± 116 pg/mL. The two groups were also not significantly different with regard to VEGF (P = 0.908), PlGF (P = 0.488), PDGF-AA (P = 0.080), sICAM-1 (P = 0.559), MCP-1 (P = 0.239), IL-6 (P = 0.450), IL-8 (P = 0.912), and IP-10 (P = 0.135; Table 1).
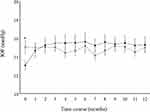
BCVA improved significantly over time in both the IRI group (P < 0.001) and the combination group (P < 0.001) (Figure 1A). Furthermore, CMT improved significantly over time in both the IRI (P < 0.001) and combination groups (P < 0.001) (Figure 1B). In addition, aqueous flare values improved significantly over time in both the IRI (P = 0.017) and combination groups (P < 0.001) (Figure 1C). No significant intergroup differences were seen in the trend profile of BCVA, CMT, or aqueous flare values (P = 0.729, P = 0.698, and P = 0.476, respectively) (Figures 1A-C). At 2 months, there was a significant difference between the two groups with respect to the CMT (IRI group, 382 ± 190 μm; combination group, 275 ± 127 μm, P = 0.041).
The mean number of IRIs during the 12-month follow-up period was 3.9 ± 1.5 (1 dose in 1 patient, 2 doses in 2 patients, 3 doses in 4 patients, 4 doses in 9 patients, 5 doses in 2 patients, 6 doses in 1 patient, and 7 doses in 2 patients) in the IRI group and 3.1 ± 1.8 (1 dose in 6 patients, 2 doses in 1 patient, 3 doses in 6 patients, 4 doses in 3 patients, 5 doses in 1 patient, 6 doses in 3 patients, and 7 doses in 0 patients) in the combination group without significant intergroup differences (Table 2). The proportion of patients with no recurrence (ie, who received only 1 dose of IRI) was significantly higher in the combination group (6/20, 30%) than in the IRI group (1/21, 4.8%; P = 0.032) (Table 2), and the time to initial recurrence was significantly longer in the combination group (3.7 ± 1.5 months) than in the IRI group (2.5 ± 0.5 months; P = 0.003; Table 2). There was no significant difference in CMT between the group with edema recurrence (683 ± 191 μm) and the group without it (581 ± 175 μm; P = 0.195).
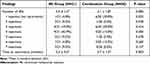 |
Table 2 Features of Intravitreal Ranibizumab Injection (IRI) in Patients Treated by IRI Alone (IRI Group) and by IRI Combined with Subtenon Triamcinolone Acetonide Injection (Combination Group) |
At baseline, IOP was significantly different between the two groups (IRI group, 15.1 ± 3.17 mmHg; combination group, 13.1 ± 2.37 mmHg, P = 0.031). IOP increased significantly over time in the combination group (P = 0.006) but not in the IRI group (P = 0.282), and the trend of IOP was significantly different between the two groups (P = 0.007; Figure 2). In the 12 months after combination treatment, IOP increased in 2 of the 20 patients (10.0%) in the combination group, but this increase could be controlled without medication.
At baseline, none of the patients had a cataract that was grade II or higher, and after initial STTA, there were no new cataracts or existing cataracts that progressed and no infectious endophthalmitis.
Discussion
This retrospective study did not confirm our hypothesis that fewer IRIs would be needed after STTA and found that the additional use of STTA did not affect the number of IRIs performed. This finding is in contrast to another study in which STTA significantly reduced the number of IRIs.11 We may not have found significant effects of STTA because it was injected only at the start of treatment. Osaka et al12 found no significant difference in the number of injections between the two groups, even though they performed STTA a mean of 2.7 times per year. Their study population included patients with an intraocular lens or type 2 diabetes. Intraocular surgery is an invasive retinal procedure that may stimulate repair and immune mechanisms and is likely to alter the chemokine profile in ocular tissues. Furthermore, diabetes may also affect cytokine levels and injection intervals. Even if patients with diabetes have no diabetic retinopathy, they already express VEGF.13 These findings may explain why the number of injections was not significantly lower in the combination group.
Ach et al14 reported that anti-VEGF therapy has no effect on macular edema associated with retinal vein occlusion, and other studies found that additional cytokines besides VEGF are involved in macular edema and that inflammatory factor concentration is correlated with macular edema severity and the size of areas without a blood supply.15,16 These findings may explain why repeated injections of anti-VEGF agents are needed.
One study found that only the presence of subfoveal fluid was associated with the density of macrophage-like cells in eyes with BRVO.17 Subfoveal retinal fluid is a known biomarker of inflammation in RVO and was shown to be correlated with the levels of inflammatory factors.18,19 The high density of macrophage-like cells in newly diagnosed BRVO, together with other inflammatory biomarkers, may indicate the potential benefit of corticosteroids in the treatment of BRVO.
Triamcinolone acetonide acts indirectly to downregulate VEGF and other inflammatory mediators in the retina and decrease the permeability of capillaries.20 Research indicates that its anti-inflammatory effects may also prevent adhesion of leukocytes and damage to the blood-retinal barrier,21–23 actions that maintain normal vascular permeability.24,25 Considering these findings, adding this steroid to IRI might be effective in extending the time to recurrence of macular edema in patients with BRVO.
In this study, the proportion of patients with no recurrence (ie, those who received only 1 dose of IRI) was significantly higher in the combination group than in the IRI group and the time to initial recurrence was significantly longer. Thus, combining IRI with initial STTA appears to have some benefits, as was shown also in an earlier study.11 Initial STTA may delay recurrence because of its long half-life: In animal studies, triamcinolone acetonide could still be measured in the neural retina after about 42 days and in the retinal pigment epithelium/choroid after about 60 days.26 In addition, in the present study, an initial STTA injection before IRI suppressed the aqueous flare value, an index of inflammation, for several months (Figure 1C), although the value was not significantly different between the two groups. Previously, we suggested that IRI reduces inflammation in patients with BRVO and macular edema.1 Campochiaro et al27 proposed a positive feedback loop for VEGF in which vascular occlusion causes retinal ischemia and ischemic retinal cells release VEGF, leading to the exacerbation of retinal nonperfusion by provoking leukostasis, which is associated with inflammation. IRI neutralizes VEGF and interrupts this positive feedback loop; interruption of this loop may have decreased the aqueous flare in our patients with BRVO by suppressing inflammation. Moreover, stable remission of macular edema in BRVO is associated with recanalization and shunt formation.28 Combination therapy prolongs the treatment interval, which may promote microcirculatory remodeling.29 Thus, the significant increase in the time between treatments is hypothesized to be due to an additive effect of IRI and STTA, but this potential synergy needs to be confirmed in future studies. The study found that recurrences of macular edema occur also after pretreatment with STTA, suggesting that combination treatment may be helpful only in a subset of patients and that treatment needs to be individualized.
IOP increased significantly more in the months after IRI plus STTA that after IRI alone, which is in agreement with earlier results.30,31 In our retrospective study, no patient needed treatment for an increase in IOP. The mean IOP had increased by 2.22 mm Hg at 12 months after STTA, whereas Iwao et al found a mean increase of 6.7 mm Hg.30 The results of our study indicate that one STTA injection may not increase IOP to concerning levels.
The strengths of this study are that STTA was performed only once, at the start of treatment; the study evaluated not only the number of injections, but also the time to recurrence; the flare value was measured every month for 1 year, which enabled us to evaluate its progression; and factors affecting treatment efficacy (eg, macular BRVO, intraocular lens, type 2 diabetes) were excluded. Also, there was less variation between the two groups than in other studies because cytokine levels before treatment were not significantly different between the groups. However, the study also has some limitations. First, the sample size was small and the data are not very recent. We plan to perform further research on this topic in another retrospective study with a larger sample size or in an adequately powered prospective study. Second, combination treatment with STTA and IRI may have long-term effects on the visual field, so future studies should include a longer follow-up with visual field tests.
Conclusions
In conclusion, we found that in the combination group, the proportion of patients with no recurrence was significantly higher than in the IRI group and the time to initial recurrence was significantly longer. These findings suggest that anti-VEGF therapy and STTA may have an additive effect in that they increase the time between treatments in patients with BRVO and macular edema.
Data Sharing Statement
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Ethics Approval and Informed Consent
The procedures used in this study were approved by the Institutional Ethics Review Board of Tokyo Medical University Hachioji Medical Center (T2022-0174), and the study was registered at http://www.umin.ac.jp (UMIN ID 000049690). This study was conducted in accordance with the World Medical Association Declaration of Helsinki. Informed consent was obtained from all subjects involved in the study.
Acknowledgments
We thank Katsunori Shimada (Department of Biostatistics, STATZ Corporation, Tokyo) for assistance with the statistical analyses.
Funding
No funding, financial support, or sponsorship was received in this study.
Disclosure
The authors report no relevant financial or non-financial conflicts of interest for this work.
References
1. Noma H, Yasuda K, Shimura M. Cytokines and the pathogenesis of macular edema in branch retinal vein occlusion. J Ophthalmol. 2019;5185128.
2. Noma H, Funatsu H, Mimura T, Eguchi S, Hori S. Soluble vascular endothelial growth factor receptor-2 and inflammatory factors in macular edema with branch retinal vein occlusion. Am J Ophthalmol. 2011;152(4):669–677 e661.
3. Campochiaro PA, Heier JS, Feiner L, et al. Ranibizumab for macular edema following branch retinal vein occlusion: six-month primary end point results of a Phase III study. Ophthalmology. 2010;117(6):1102–1112 e1101.
4. Noma H, Yasuda K, Shimura M. Change of cytokines after intravitreal ranibizumab in patients with recurrent branch retinal vein occlusion and macular edema. Eur J Ophthalmol. 2021;31(1):204–210.
5. Noma H, Mimura T, Yasuda K, et al. Cytokines and recurrence of macular edema after intravitreal ranibizumab in patients with branch retinal vein occlusion. Ophthalmologica. 2016;236(4):228–234.
6. Lashay A, Riazi-Esfahani H, Mirghorbani M, Yaseri M. Intravitreal medications for retinal vein occlusion: systematic review and meta-analysis. J Ophthalmic Vis Res. 2019;14(3):336–366.
7. Patil NS, Hatamnejad A, Mihalache A, Popovic MM, Kertes PJ, Muni RH. Anti-vascular endothelial growth factor treatment compared with steroid treatment for retinal vein occlusion: a meta-analysis. Ophthalmologica. 2022;245(6):500–515.
8. Sakanishi Y, Tamaki K, Mashimo K, Sakuma T, Ebihara N. Relationship between recurrence of macular edema due to branch retinal vein occlusion and changes in choroidal thickness. Ophthalmic Res. 2021;64(3):363–368.
9. Noma H, Mimura T, Shimada K. Role of inflammation in previously untreated macular edema with branch retinal vein occlusion. BMC Ophthalmol. 2014;14:67.
10. Noma H, Mimura T, Yasuda K, Shimura M. Role of soluble vascular endothelial growth factor receptors-1 and −2, their ligands, and other factors in branch retinal vein occlusion with macular edema. Invest Ophthalmol Vis Sci. 2014;55(6):3878–3885.
11. Moon J, Kim M, Sagong M. Combination therapy of intravitreal bevacizumab with single simultaneous posterior subtenon triamcinolone acetonide for macular edema due to branch retinal vein occlusion. Eye. 2016;30(8):1084–1090.
12. Osaka R, Muraoka Y, Nakano Y, et al. One-year results of anti-vascular endothelial growth factor therapy combined with triamcinolone acetonide for macular edema associated with branch retinal vein occlusion. Jpn J Ophthalmol. 2020;64(6):605–612.
13. Cheung CM, Vania M, Ang M, Chee SP, Li J. Comparison of aqueous humor cytokine and chemokine levels in dia betic patients with and without retinopathy. Mol Vis. 2012;18:830–837.
14. Ach T, Hoeh AE, Schaal KB, Scheuerle AF, Dithmar S. Predictive factors for changes in macular edema in intravitreal bevacizumab therapy of retinal vein occlusion. Graefes Arch Clin Exp Ophthalmol. 2010;248(2):155–159.
15. Noma H, Funatsu H, Mimura T, Harino S, Sone T, Hori S. Increase of vascular endothelial growth factor and interleukin-6 in the aqueous humour of patients with macular oedema and central retinal vein occlusion. Acta Ophthalmol. 2010;88(6):646–651.
16. Noma H, Funatsu H, Mimura T, Eguchi S, Shimada K, Hori S. Vitreous levels of pigment epithelium-derived factor and vascular endothelial growth factor in macular edema with central retinal vein occlusion. Curr Eye Res. 2011;36(3):256–263.
17. Maltsev DS, Kulikov AN, Volkova YV, Burnasheva MA, Vasiliev AS. Retinal macrophage-like cells as a biomarker of inflammation in retinal vein occlusions. J Clin Med. 2022;11(24):56.
18. Koss M, Pfister M, Rothweiler F, et al. Correlation from undiluted vitreous cytokines of untreated central retinal vein occlusion with spectral domain optical coherence tomography. Open Ophthalmol J. 2013;7:11–17.
19. Pfister M, Rothweiler F, Michaelis M, et al. Correlation of inflammatory and proangiogenic cytokines from undiluted vitreous samples with spectral domain OCT scans, in untreated branch retinal vein occlusion. Clin Ophthalmol. 2013;7:1061–1067.
20. McAllister IL, Vijayasekaran S, Chen SD, Yu DY. Effect of triamcinolone acetonide on vascular endothelial growth factor and occludin levels in branch retinal vein occlusion. Am J Ophthalmol. 2009;147(5):838–846, 846 e831–832.
21. Kurtz RM, Elner VM, Bian ZM, Strieter RM, Kunkel SL, Elner SG. Dexamethasone and cyclosporin A modulation of human retinal pigment epithelial cell monocyte chemotactic protein-1 and interleukin-8. Invest Ophthalmol Vis Sci. 1997;38(2):436–445.
22. Sadowski T, Steinmeyer J. Effects of polysulfated glycosaminoglycan and triamcinolone acetonid on the production of proteinases and their inhibitors by IL-1alpha treated articular chondrocytes. Biochem Pharmacol. 2002;64(2):217–227.
23. Mizuno S, Nishiwaki A, Morita H, Miyake T, Ogura Y. Effects of periocular administration of triamcinolone acetonide on leukocyte-endothelium interactions in the ischemic retina. Invest Ophthalmol Vis Sci. 2007;48(6):2831–2836.
24. Miyamoto K, Khosrof S, Bursell SE, et al. Prevention of leukostasis and vascular leakage in streptozotocin-induced diabetic retinopathy via intercellular adhesion molecule-1 inhibition. Proc Natl Acad Sci U S A. 1999;96(19):10836–10841.
25. Nishijima K, Kiryu J, Tsujikawa A, et al. Inhibitory effects of antithrombin III on interactions between blood cells and endothelial cells during retinal ischemia-reperfusion injury. Invest Ophthalmol Vis Sci. 2003;44(1):332–341.
26. Nan K, Sun S, Li Y, et al. Characterisation of systemic and ocular drug level of triamcinolone acetonide following a single sub-Tenon injection. Br J Ophthalmol. 2010;94(5):654–658.
27. Campochiaro PA, Wykoff CC, Shapiro H, et al. Neutralization of vascular endothelial growth factor slows progression of retinal nonperfusion in patients with diabetic macular edema. Ophthalmology. 2014;121(9):1783–1789.
28. Suzuki N, Hirano Y, Tomiyasu T, et al. Collateral vessels on optical coherence tomography angiography in eyes with branch retinal vein occlusion. Br J Ophthalmol. 2019;103(10):1373–1379.
29. Cehofski LJ, Kruse A, Bøgsted M, et al. Retinal proteome changes following experimental branch retinal vein occlusion and intervention with ranibizumab. Exp Eye Res. 2016;152:49–56.
30. Iwao K, Inatani M, Kawaji T, Koga T, Mawatari Y, Tanihara H. Frequency and risk factors for intraocular pressure elevation after posterior sub-Tenon capsule triamcinolone acetonide injection. J Glaucoma. 2007;16(2):251–256.
31. Kawamura R, Inoue M, Shinoda H, et al. Incidence of increased intraocular pressure after subtenon injection of triamcinolone acetonide. J Ocul Pharmacol Ther. 2011;27(3):299–304.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.