Back to Journals » International Journal of General Medicine » Volume 14
Anti-PD1 Therapy Plus Whole-Brain Radiation Therapy May Prolong PFS in Selected Non–Small Cell Lung Cancer Patients with Brain Metastases: A Retrospective Study
Authors Khan M , Zhao Z, Li X, Liao G
Received 12 August 2021
Accepted for publication 6 October 2021
Published 26 November 2021 Volume 2021:14 Pages 8903—8918
DOI https://doi.org/10.2147/IJGM.S333890
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Muhammad Khan,1,2 Zhihong Zhao,3 Xianming Li,1 Guixiang Liao1
1Department of Oncology, Shenzhen People’s Hospital, First Affiliated Hospital of Southern University of Science and Technology, Shenzhen, People’s Republic of China; 2Department of Oncology, First Affiliated Hospital of Anhui Medical University, Hefei, Anhui Province, People’s Republic of China; 3Department of Nephrology, Shenzhen People’s Hospital, Second Clinical Medicine Centre, Jinan University, Shenzhen, People’s Republic of China
Correspondence: Guixiang Liao; Xianming Li
Department of Radiation Oncology, Shenzhen People’s Hospital, First Affiliated Hospital of Southern University of Science and Technology, Shenzhen, 518020, People’s Republic of China
Email [email protected]; [email protected]
Background: Whole-brain radiotherapy (WBRT) remains an essential modality of treatment for brain metastases (BMs) derived from non-small cell lung cancer (NSCLC) patients and anti-PD-1 therapy has demonstrated intracranial responses in these patients. We aimed to evaluate if the combination of the two treatments could yield additive efficacy.
Methods: A retrospective review of our institution’s database was carried out to identify NSCLC patients with BMs who had been treated with anti-PD1 therapy and/or WBRT between 2015 and 2020. Patient characteristics, main outcomes, including progression-free survival (PFS) and overall survival (OS), and factors affecting these outcomes were analyzed. SPSS 24 was used for statistical analysis. Appropriate statistical tests were employed according to the type of data.
Results: Overall, 21 NSCLC BM patients were identified that had received WBRT. Of these, ten had been additionally treated with anti-PD1 therapy within 30 days of WBRT initiation. Median PFS was 3 (95% CI 0.8– 5.1) months with WBRT alone versus 11 (95% CI 6.3– 15.6) months with combined treatment. Risk of disease progression was 71% lower with the combined approach (HR 0.29, 95% CI 0.11– 0.80; p=0.016). A trend toward improved OS was also observed with the combined approach (HR 0.33, 95% CI 0.08– 1.12; p=0.107). Concurrent treatment (p=0.028) and male sex (p=0.052) were associated with improved PFS, while OS was associated only with age (p=0.02).
Conclusion: Concurrent WBRT and anti-PD1 therapy may delay progression and improve survival in BM patients with confirmed EGFR- and ALK-negative NSCLC histology. Prospective studies are warranted to validate and elucidate on the additive effect of the two modalities.
Keywords: brain metastasis, BM, whole-brain radiation therapy, WBRT, non–small cell lung cancer, NSCLC, immune checkpoint blockade, ICB, combination, combined therapy
Introduction
Lung cancer is the leading cause of death from cancer in the US.1 Non–small cell lung carcinoma (NSCLC) constitutes 85% of lung cancer cases.1,2 A majority of NSCLC cases are diagnosed at an advanced stage (around 60%) with a 5-year survival rate of merely 5%.1 In general, platinum-based chemotherapy is offered as first-line treatment for advanced-stage NSCLC patients, with a 20% response rate.3,4 Molecular targeted agents are recommended for NSCLC patients with specific genetic mutations, such as EGFR and ALK rearrangement, which are present in 10%–15% and 5% of NSCLC cases, respectively.5–7 Prevalence of EGFR+ (up to 30%) and ALK+ NSCLC is higher among Asian populations.8 However, ALK rearrangement is likely because of the high proportion of never-smokers (30% in Asia versus 10% in US) and younger age of onset in East Asian NSCLC cases.9 Recently, anti-PD1/PDL1 monoclonal antibodies have also been approved for advanced-stage NSCLC in first/second-line settings, alone or in combination with chemotherapy.10 Innovative strategies, such as addition of stereotactic ablative radiotherapy (RT) to immunotherapy, are also being pursued, and have demonstrated abscopal responses in metastatic sites and delayed disease progression.11,12
Around 40% of NSCLC patients experience brain metastases (BM) during disease progression.13,14 Depending on the presentation, management of BMs may comprise whole-brain radiation therapy (WBRT) alone, surgical resection with/without stereotactic radiosurgery (SRS)/WBRT, and SRS alone or with/without WBRT.15–18 A surge in the application of SRS has emerged in recent years.19 Nonetheless, WBRT alone remains a major component of BM management.15,19,20 Chemotherapy fails to attack BMs due to selective screening of the blood–brain barrier.21 On the other hand, molecularly targeted and immunotherapeutic agents have shown intracranial responses in NSCLC BM patients.22–42 Of the former, gefitinib (87.8%), erlotinib (82.4%), icotinib (67.1%), afatinib (35%), and osimertinib in EGFR+ NSCLC and crizotinib (21%), ceritinib (73%), alectinib (57%), brigatinib (42%–67%), lorlatinib (71%), and ensartinib (64%) in ALK+ NSCLC have shown excellent intracranial responses.22–33 Molecularly targeted agents have also displayed additive effects in combination with RT compared to RT alone, but these are restricted to a small percentage of NSCLC patients.43–46 For NSCLC BM patients with no genetic mutations (EGFR–/ALK–), immunotherapeutic agents, such as anti-CTLA4 and anti-PD1/PDL1 mAbs can be an optimal option. In fact, combination of RT and immunotherapeutic agents has demonstrated synergistic responses in BM patients.47–55 Herein, we present a retrospective review of NSCLC BM patients treated with WBRT alone or WBRT plus anti-PD1 to elucidate on additive effects of additional anti-PD1 therapy.
Methods
Patient Selection
A retrospective review was performed of 21 EGFR- and ALK-negative NSCLC patients with BMs who had been treated at our institution. Ethics approval was obtained from the institutional review board of Shenzhen People’s Hospital, Shenzhen, China. Written informed consent for participation was obtained from patients or their guardians in accordance with the Declaration of Helsinki.56 STROBE guidelines for cohort studies were followed for reporting.57 The patients had either received WBRT alone or WBRT plus anti-PD1 monoclonal antibodies during 2015–2020. All included patients had developed BMs after being treated with first-line platinum-based chemotherapy at initial lung cancer diagnosis. Patients in the control group had been offered second-line docetaxel chemotherapy for systemic disease and WBRT for BMs. The median dose of WBRT was 30 Gy/10 F for the entire cohort. Anti-PD1 therapy was initiated within 30 days of WBRT induction. A median of six cycles (three to 17) had been received by the patients. Baseline characteristics, eg, age, sex, smoking history, performance status, histopathology of lung cancer, and cancer differentiation, were recorded for the entire cohort.
Follow-Up and End Points
The primary end point was progression-free survival (PFS), defined as time from BM diagnosis to disease progression on clinical and radiological evaluation during follow-up or death following treatment induction. Progression of disease was defined according to RECIST 1.1 criteria, which characterizes new BM occurrence also as disease progression.58 Overall survival (OS) was the secondary end point and defined as time from BM diagnosis to death. Patients were followed up with clinical evaluation and radiological imaging (CTs and MRIs) obtained at 3-, 6-month, and 1-year intervals.
Statistical Analysis
Statistical analysis was carried out with SPSS 24. Relationships between groups for baseline characteristics were determined with chi–square tests for categorical variables, and Fisher’s exact test was used when small cells were encountered using 2×2 contingency tables. For continuous variables, two-tailed t-tests were used to examine comparisons. Median OS, PFS, and univariate analyses were performed using the Kaplan–Meier method. Factors with p<0.25 on univariate analyses were selected for multivariate analyses. The Cox proportional-hazard model was adopted for calculating HRs and 95% CIs for OS and PFS and to undertake multivariate analyses. p≤0.05 was considered to reflect statistical significance.
Results
Patient Characteristics
Our study looked at 21 patients with three or more BMs derived from confirmed EGFR-negative and ALK-negative stage IV NSCLC. A majority had poorly differentiated adenocarcinoma histopathology, as shown in Table 1. All patients were treated with WBRT between 2015 and 2020. Ten additionally received anti-PD1 antibody treatment initiated within 30 days of WBRT induction. Median age was 56 years and median follow-up 13 months. The cohorts differed significantly only in terms of smoking status (p=0.047). Never-smokers were predominant in the WBRT-alone group. The cohorts showed no significant differences for the other baseline characteristics: age, sex, histopathology, tumor differentiation, number of extracranial metastatic organs, and follow-up duration. Baseline characteristics of the participants are outlined in Table 1.
 |
Table 1 Baseline characteristics of study participants |
Progression-Free Survival
Median PFS was 3 (95% CI 0.8–5.1) months with WBRT alone versus 11 (95% CI 6.3–15.6) monthswith combined treatment (Figure 1). Risk of disease progression was 71% lower with the combined approach (HR 0.29, 95% CI 0.11–0.80; p=0.016). Potential predictors of PFS were examined: age, sex, smoking history, tumor histopathology and differentiation, KPS score, and existence of extracranial metastatic organs (Tables 2 and 3). With the exception of WBRT plus anti-PD1 treatment (p=0.010), none of the factors investigated was significantly associated with PFS. Three factors that showed close association (p<0.25) with PFS on univariate analyses were selected for multivariate analysis. Of the three factors, treatment type and male sex showed significant prognostic association with PFS on multivariate analyses.
 |
Table 2 Univariate analysis of progression-free survival |
 |
Table 3 Multivariate analysis of progression-free and overall survival |
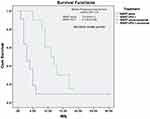 |
Figure 1 Kaplan–Meier progression-free survival (PFS) curves for WBRT alone (no PD1), and WBRT plus PD1 inhibition therapy (WBRT+PD1). Abbreviation: Cum, cumulative. |
Overall Survival
Median OS was 13 (95% CI 9.9–16.0) months with WBRT alone versus 24 months (95% CI not reached) with WBRT plus anti-PD1 therapy (Figure 2). The risk of death was 67% lower with WBRT plus anti-PD1 therapy than WBRT alone (HR 0.33, 95% CI 0.08–1.12; p=0.107). None of the factors examined on univariate analyses was significantly associated with improved OS (Table 4). Only treatment type was suggestive of prognostic value for OS (p=0.088). Multivariate analyses consisted of predictive factors that showed close association with OS: treatment type, age, sex, and number of metastatic organs. Only age was significantly associated with better OS (p=0.020). There was a suggestion of prognostic association for sex (p=0.073) and treatment type (p=0.070).
 |
Table 4 Univariate analysis of overall survival |
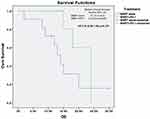 |
Figure 2 Kaplan–Meier overall survival (OS) curves for WBRT alone (no PD1), and WBRT plus PD1-inhibition therapy (WBRT+PD1). Abbreviation: Cum, cumulative. |
Discussion
Advances in systemic therapies, ie, molecularly targeted therapy and immunotherapy, have opened up new therapeutic options for BM patients.22–42,59,60 Both these systemic treatments have shown intracranial responses and prolonged survival.22–42 In our study, patients who had received WBRT were also treated with anti-PD1 therapy. In comparison to the cohort with only brain-directed WBRT, these patients showed prolonged PFS and OS.
Our results are supported by other studies carried out with similar designs, where adding immunotherapy to RT resulted in a benefit for NSCLC BM patients.42,47–55,61–64 In patients with a history of RT (brain and extracranial), pembrolizumab significantly improved PFS (HR 0.56, 95% CI 0.34–0.91; p=0.019) and OS (HR 0.58, 95% CI 0.36–0.94; p=0.026) compared to patients receiving pembrolizumab without RT history.47 Secondary analysis of a phase III trial also revealed superior PFS (HR 0.38. 95% CI 0.16–0.91; p=0.02) and OS (HR 0.74, 95% CI 0.49–1.13; p=0.16) with atezolizumab to chemotherapy in which both cohorts had received RT to the brain.48 A large retrospective study comprising 13,998 NSCLC patients revealed that addition of immunotherapy (n=545) to RT was associated with an improvement in OS (13.1 vs 9.7 months, p<0.0001).49 Unfortunately, no details were provided, and the study was published only as an abstract. In a separate study involving NSCLC, response rates were similar between patients with BMs (20.6%) and without BMs (22.7%) with the use of combined treatment (p=0.484). Although PFS (1.7 months vs 2.1, p=0.009) and OS (8.6 months vs 11.4, p=0.035) were significantly longer in patients without BMs, there was no association found for BMs on OS on multivariate analysis.50 In a retrospective matched-cohort study of NSCLC-derived BM patients who had received ICIs within 3 months showed significantly rapid regression of BMs (2.5 vs 3.1 months, p<0.0001) and improved CNS complete response (eight of 16 [50%] vs five of 32 [15.6%], p=0.012) for concurrent use of ICI and SRS (n=17, BMs 45) compared to SRS alone (n=34, BMs 92).51 Nonetheless, no survival benefit was exhibited in the form of PFS (HR 2.18, 95% CI 0.72–6.62; p=0.11) or OS (HR 0.99, 95% CI 0.39–2.52; p=0.99). Likewise, a retrospective study of 85 NSCLC BM patients showed no statistical difference in median survival for an IT group (n=39) and CT group (n=46) — median OS 10 vs 11.6 months, p=0.23 — despite significantly superior lesion shrinkage for the IT cohort in a subset of patients with lesion volume >500 mm3 (90% vs 47.8%, p=0.001).52 In conclusion, in accordance with our study, these studies provide firm support for the use of immune checkpoint inhibitors along with RT.
Several studies that included BM patients with other primary tumor sites, such as melanoma, RCC, and others, in addition to NSCLC, have also shown intracranial responses with/without an improvement in PFS and OS.42,53,54 An enhanced response rate of 60% was revealed with palliative RT plus durvalumab in a secondary analysis of BM patients (NSCLC, melanoma, RCC).42 Continuation of PD1-inhibition therapy (median 179 days) after RT in a small subgroup of 25 BM patients who had also received initial PD1-inhibition therapy before RT showed an additional 238 days’ improvement in survival.54 In another retrospective study (n=260), improved median OS was observed with SRS/SRT and ICIs compared to SRS/SRT alone (14.5 vs 12 months).53 However, this study failed to report any difference in PFS for treatment cohorts (PFS CI 2.3 vs nCI 2.3 vs SRS alone 3.7 months).53 In a study by Kotecha et al, significant improvement in overall best objective response was observed with concurrent RT compared to SRS alone (67% vs 57%, p=0.014).55
Our study fails to provide direct proof of an additive effect for the two treatments; therefore, medical literature was explored to gather such evidence in BMs. Two arguments can be given that support the additive effect of RT–ICI combination. Firstly, as outlined in Table 5, several studies have reported intracranial activity of ICIs in BMs. As monotherapy, immune checkpoint inhibitors targeted at the PD1/PDL1 checkpoint have reported 9%–33% intracranial response rates in NSCLC BM patients.36–41 Secondly, close sequencing of ICI with RT has been shown to enhance the additive effect of combined treatment, probably by taking advantage of local damage caused to the blood–brain barrier during RT, thereby providing a window of opportunity for immune checkpoint blockers to cross into the brain and be more effective.65 Several studies reporting failure of the combined approach in improving outcomes of patients have pointed out the importance of RT–ICI sequencing.51,53,55 For example, Chen et al found that patients receiving ICIs within 2 weeks (n=28) derived the best survival advantage (24.7 months), which was significantly better than other cohorts of nonconcurrent ICIs (HR 2.40, p=0.006) and SRS/SRT alone (HR 2.69, p=0.002).53 Similarly, Kotecha et al study found no difference in intracranial response for the treatment difference (59% vs 56%, p=0.34); however, significant intracranial response was observed in patients receiving immediate ICI (71% vs 53%, p=0.008).55 Alternatively, a longer window between the treatments may cause failure, as reported in Shepard et al (ICI within 3 months of RT).51 A 14-day window for palliative RT and immunotherapy has been considered safe, and early initiation of immunotherapy after RT may also capitalize on residual and ongoing radiation-induced tumor-antigeni stimulation.66,67 A concurrent approach is also supported by preclinical evidence to avert acquired resistance to fractionated RT.68 Several other studies that used combined treatment have also demonstrated the effect of RT–ICI sequencing on outcomes of BM patients.61–64 In a small cohort of NSCLC BM patients (n=17), delivery of anti-PD1 (nivolumab/durvalumab) before or concurrently (median 21 days before/after RT) with SRS/fractionated stereotactic RT demonstrated significantly improved 6-month distant brain control rate (57% vs 0, p=0.05) compared to patients receiving anti-PD1 after RT at a median 1.6 (range 0.2–4.7) months.61 Univariate analysis revealed timing was also significantly associated with OS (HR 9.2, 95% CI 1.9–65.3; p=0.006).61 Concurrent or after PD1-inhibitor induction was associated with higher intracranial 1-year local control (100% vs 72.3%, p=0.016) compared to patients receiving PD1-pathway inhibition before SRS in a retrospective study of 37 lung cancer patients with 85 BM lesions.63 Moreover, 1-year distal brain failure (p=0.042) and 1-year OS (p=0.008) also showed significant differences for PD1-therapy sequencing, as shown in Table 5. A study involving BM patients of multiple primary sites, however, showed no intracranial failure difference between concurrent (defined as ICI given within 4 weeks of SRS) versus noncurrent (within 5 months).64 Nonetheless, improved extracranial control and OS was higher in the concurrent group.
 |  |  |  |
Table 5 Studies reporting intracranial responses and clinical efficacy of immune checkpoint inhibitors alone or combined with RT in the management of brain metastasis–derived from NSCLC |
Efficacy of ICIs in lung cancer has also been associated with EGFR-mutation status.69 EGFR wild-type was associated with increased OS compared to EGFR-mutated NSCLC.69 Our study included only EGFR-negative NSCLC patients for better assessment of combined treatment. Most of these studies contained NSCLC patients that were positive for EGFR, ALK, and KRAS mutations.38,39,41,54,61,62,64 Inclusion of such patients in treatment/control groups may confound ultimate survival advantage, as molecularly targeted agents aimed at these oncoproteins have shown intracranial responses and improved outcome compared to RT alone.43–46 Such observations may explain failure of ICI + RT–induced intracranial response translation into PFS and survival advantage.51,52 In our study, male sex and age were associated with improved PFS and/or OS on univariate/multivariate analyses. However, this could mainly have been due to the revalence of male gender in the anti-PD1 cohort (nine vs one). Likewise, patients aged <60 years were predominant in the entire cohort (14 vs seven). Therefore, these factors may have contributed to the association between these factors and efficacy outcomes.
Our study is limited by the small cohort and retrospective nature of research design. The small cohort limits the reliability of multivariate analysis in our study. Moreover, our study was not powered sufficiently to detect OS advantage, and failure to register OS should be interpreted with caution. Retrospective research studies are prone to recall, observation, and selection biases.70 Men and smokers were predominant in the combined group, which may limit the efficacy outcomes observed in our study, as smoking is associated with induction of PDL1 expression, which in turn is used as a biomarker to predict response to ICI.71 No PDL1 expression was assessed for patient selection in our study. Our study is also prone to chronological bias, as participants in the two cohorts were not from the same period. PD1 inhibior–treated patients had been diagnosed more recently. Furthermore, lack of assessment of safety and adverse events also limits the application of our results.
Conclusion
Our results suggest anti-PD1 therapy as an alternative treatment option in NSCLC BM patients lacking EGFR and ALK mutations. NSCLC BM patients showed a trend toward improved PFS and OS with the combined approach. Further evaluation of WBRT and anti-PD1 therapy combinations are warranted in larger studies.
Data Sharing
The data sets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics Approval and Consent to Participate
Ethics approval was obtained from the tthical review board of Shenzhen People’s Hospital, Shenzhen, China. All study participants or legal guardians provided informed written consent prior to study enrollment.
Author Contributions
All authors made a significant contribution to the work reported, whether in conception, design, execution, acquisition of data, analysis and interpretation, or all these areas, took part in drafting, revising, or critically reviewing the article, gave final approval to the version to be published, have agreed on the journal to which the article has been submitted, and agree to be accountable for all aspects of the work.
Funding
The Natural Science Foundation of Shenzhen (JCYJ20170307095828424) and Shenzhen Health and Family Planning System Research Project ((SZBC2017024) provided support for this work.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2020. CA Cancer J Clin. 2020;70(1):7–30. doi:10.3322/caac.21590
2. Petersen I. The morphological and molecular diagnosis of lung cancer. Dtsch Arztebl Int. 2011;108(31–32):525–531. doi:10.3238/arztebl.2011.0525
3. Hanna N, Shepherd FA, Fossella FV, et al. Randomized phase III trial of pemetrexed versus docetaxel in patients with non-small-cell lung cancer previously treated with chemotherapy. J Clin Oncol. 2004;22(9):1589–1597. doi:10.1200/jco.2004.08.163
4. Schiller JH, Harrington D, Belani CP, et al. Comparison of four chemotherapy regimens for advanced non-small-cell lung cancer. N Engl J Med. 2002;346(2):92–98. doi:10.1056/NEJMoa011954
5. Travis WD, Brambilla E, Noguchi M, et al. International Association for the Study of Lung Cancer/American Thoracic Society/European Respiratory Society international multidisciplinary classification of lung adenocarcinoma. J Thor Oncol. 2011;6(2):244–285. doi:10.1097/JTO.0b013e318206a221
6. Gerber DE. EGFR inhibition in the treatment of non-small cell lung cancer. Drug Dev Res. 2008;69(6):359–372. doi:10.1002/ddr.20268
7. Khan M, Lin J, Liao G, et al. ALK inhibitors in the treatment of ALK positive NSCLC. Front Oncol. 2019;8:557. doi:10.3389/fonc.2018.00557
8. Sekine I, Yamamoto N, Nishio K, Saijo N. Emerging ethnic differences in lung cancer therapy. Br J Cancer. 2008;99(11):1757–1762. PubMed PMID: 18985035; PubMed Central PMCID: PMCPMC2600690. doi:10.1038/sj.bjc.6604721
9. Zhou W, Christiani DC. East meets West: ethnic differences in epidemiology and clinical behaviors of lung cancer between East Asians and Caucasians. Chin J Cancer. 2011;30(5):287–292. PubMed PMID: 21527061. doi:10.5732/cjc.011.10106
10. Huang Z, Su W, Lu T, et al. First-line immune-checkpoint inhibitors in non-small cell lung cancer: current landscape and future progress. Front Pharmacol. 2020;11:1591. doi:10.3389/fphar.2020.578091
11. Chicas-Sett R, Morales-Orue I, Castilla-Martinez J, et al. Stereotactic ablative radiotherapy combined with immune checkpoint inhibitors reboots the immune response assisted by immunotherapy in metastatic lung cancer: a systematic review. Int J Mol Sci. 2019;20(9):9. doi:10.3390/ijms20092173
12. Luke JJ, Lemons JM, Karrison TG, et al. Safety and clinical activity of pembrolizumab and multisite stereotactic body radiotherapy in patients with advanced solid tumors. J Clin Oncol. 2018;36(16):1611–1618. doi:10.1200/jco.2017.76.2229
13. Eichler AF, Chung E, Kodack DP, Loeffler JS, Fukumura D, Jain RK. The biology of brain metastases-translation to new therapies. Nat Rev Clin Oncol. 2011;8(6):344–356. doi:10.1038/nrclinonc.2011.58
14. Liao BC, Lin CC, Yang JC. Treating brain metastases in non-small cell lung cancer patients: what have we learnt from pharmaceutical recent clinical trials? Expert Opin Pharmacother. 2018;19(8):851–864. doi:10.1080/14656566.2018.1472765
15. Mehta MP, Aoyama H, Gondi V. The changing role of whole-brain radiotherapy: demise or time for selective usage? JAMA Oncol. 2017;3(8):1021–1022. PubMed PMID: 28056151. doi:10.1001/jamaoncol.2016.5414
16. Linskey ME, Andrews DW, Asher AL, et al. The role of stereotactic radiosurgery in the management of patients with newly diagnosed brain metastases: a systematic review and evidence-based clinical practice guideline. J Neurooncol. 2010;96(1):45–68. doi:10.1007/s11060-009-0073-4
17. Lippitz B, Lindquist C, Paddick I, Peterson D, O’Neill K, Beaney R. Stereotactic radiosurgery in the treatment of brain metastases: the current evidence. Cancer Treat Rev. 2014;40(1):48–59. doi:10.1016/j.ctrv.2013.05.002
18. Khan M, Lin J, Liao G, et al. Comparison of WBRT alone, SRS alone, and their combination in the treatment of one or more brain metastases: review and meta-analysis. Tumour Biol. 2017;39(7):1010428317702903. doi:10.1177/1010428317702903
19. Barbour AB, Jacobs CD, Williamson H, et al. Radiation therapy practice patterns for brain metastases in the United States in the stereotactic radiosurgery era. Advan Rad Oncol. 2020;5(1):43–52. doi:10.1016/j.adro.2019.07.012
20. Khan M, Arooj S, Li R, et al. Tumor primary site and histology subtypes role in radiotherapeutic management of brain metastases. Front Oncol. 2020;10:781. doi:10.3389/fonc.2020.00781
21. Angeli E, Nguyen TT, Janin A, Bousquet G. How to make anticancer drugs cross the blood–brain barrier to treat brain metastases. Int J Mol Sci. 2019;21(1):22. doi:10.3390/ijms21010022
22. Iuchi T, Shingyoji M, Sakaida T, et al. Phase II trial of gefitinib alone without radiation therapy for Japanese patients with brain metastases from EGFR-mutant lung adenocarcinoma. Lung Cancer (Amsterdam, Netherlands). 2013;82(2):282–287. PubMed PMID: 24021541. doi:10.1016/j.lungcan.2013.08.016
23. Porta R, Sánchez-Torres JM, Paz-Ares L, et al. Brain metastases from lung cancer responding to erlotinib: the importance of EGFR mutation. Eur Respir J. 2011;37(3):624–631. PubMed PMID: 20595147. doi:10.1183/09031936.00195609
24. Hoffknecht P, Tufman A, Wehler T, et al. Efficacy of the irreversible ErbB family blocker Afatinib in epidermal growth factor receptor (EGFR) tyrosine kinase inhibitor (TKI)-pretreated non-small-cell lung cancer patients with brain metastases or leptomeningeal disease. J Thor Oncol. 2015;10(1):156–163. PubMed PMID: 25247337; PubMed Central PMCID: PMCPMC4276567. doi:10.1097/jto.0000000000000380
25. Schuler M, Wu YL, Hirsh V, et al. First-line Afatinib versus chemotherapy in patients with non-small cell lung cancer and common epidermal growth factor receptor gene mutations and brain metastases. J Thor Oncol. 2016;11(3):380–390. PubMed PMID: 26823294. doi:10.1016/j.jtho.2015.11.014
26. Wu YL, Yang JJ, Zhou C, et al. PL03.05: BRAIN: a Phase III trial comparing WBI and chemotherapy with Icotinib in NSCLC with brain metastases harboring EGFR mutations (CTONG 1201). J Thor Oncol. 2017;12(1):S6. doi:10.1016/j.jtho.2016.11.007
27. Mok TS, Wu Y-L, Ahn M-J, et al. Osimertinib or platinum–pemetrexed in EGFR T790M–positive lung cancer. N Engl J Med. 2016;376(7):629–640. doi:10.1056/NEJMoa1612674
28. Solomon BJ, Cappuzzo F, Felip E, et al. Intracranial efficacy of crizotinib versus chemotherapy in patients with advanced ALK-positive non-small-cell lung cancer: results from PROFILE 1014. J Clin Oncol. 2016;34(24):2858–2865. PubMed PMID: 27022118. doi:10.1200/jco.2015.63.5888
29. Soria JC, Tan DSW, Chiari R, et al. First-line ceritinib versus platinum-based chemotherapy in advanced ALK-rearranged non-small-cell lung cancer (ASCEND-4): a randomised, open-label, Phase 3 study. Lancet (London, England). 2017;389(10072):917–929. PubMed PMID: 28126333. doi:10.1016/s0140-6736(17)30123-x
30. Ou SH, Ahn JS, De Petris L, et al. Alectinib in crizotinib-refractory ALK-rearranged non-small-cell lung cancer: a Phase II global study. J Clin Oncol. 2016;34(7):661–668. PubMed PMID: 26598747. doi:10.1200/jco.2015.63.9443
31. Kim DW, Tiseo M, Ahn MJ, et al. Brigatinib in patients with crizotinib-refractory anaplastic lymphoma kinase-positive non-small-cell lung cancer: a randomized, multicenter Phase II trial. J Clin Oncol. 2017;35(22):2490–2498. PubMed PMID: 28475456. doi:10.1200/jco.2016.71.5904
32. Shaw AT, Bauer TM, de Marinis F, et al. First-line lorlatinib or crizotinib in advanced ALK-positive lung cancer. N Engl J Med. 2020;383(21):2018–2029. doi:10.1056/NEJMoa2027187
33. Horn L, Wang Z, Wu G, et al. Ensartinib vs crizotinib for patients with anaplastic lymphoma kinase−positive non–small cell lung cancer: a randomized clinical trial. JAMA Oncol. 2021. doi:10.1001/jamaoncol.2021.3523
34. Dagogo-Jack I, Gill CM, Cahill DP, Santagata S, Brastianos PK. Treatment of brain metastases in the modern genomic era. Pharmacol Ther. 2017;170:64–72. doi:10.1016/j.pharmthera.2016.10.011
35. Martínez P, Mak RH, Oxnard GR. Targeted Therapy as an alternative to whole-brain radiotherapy in EGFR-mutant or ALK-positive non-small-cell lung cancer with brain metastases. JAMA Oncol. 2017;3(9):1274–1275. doi:10.1001/jamaoncol.2017.1047
36. Dudnik E, Yust-Katz S, Nechushtan H, et al. Intracranial response to nivolumab in NSCLC patients with untreated or progressing CNS metastases. Lung Cancer. 2016;98:114–117. doi:10.1016/j.lungcan.2016.05.031
37. Hellmann MD, Rizvi NA, Goldman JW, et al. Nivolumab plus ipilimumab as first-line treatment for advanced non-small-cell lung cancer (CheckMate 012): results of an open-label, Phase 1, multicohort study. Lancet Oncol. 2017;18(1):31–41. doi:10.1016/s1470-2045(16)30624-6)30624-6
38. Spigel DR, Chaft JE, Gettinger S, et al. FIR: efficacy, safety, and biomarker analysis of a Phase II open-label study of atezolizumab in PD-L1-Selected patients with NSCLC. J Thor Oncol. 2018;13(11):1733–1742. doi:10.1016/j.jtho.2018.05.004
39. Gauvain C, Vauléon E, Chouaid C, et al. Intracerebral efficacy and tolerance of nivolumab in non-small-cell lung cancer patients with brain metastases. Lung Cancer. 2018;116:62–66. doi:10.1016/j.lungcan.2017.12.008
40. Crinò L, Bronte G, Bidoli P, et al. Nivolumab and brain metastases in patients with advanced non-squamous non-small cell lung cancer. Lung Cancer (Amsterdam, Netherlands). 2019;129:35–40. doi:10.1016/j.lungcan.2018.12.025
41. Goldberg SB, Gettinger SN, Mahajan A, et al. Pembrolizumab for patients with melanoma or non-small-cell lung cancer and untreated brain metastases: early analysis of a non-randomised, open-label, Phase 2 trial. Lancet Oncol. 2016;17(7):976–983. doi:10.1016/s1470-2045(16)30053-5
42. Levy A, Massard C, Soria JC, Deutsch E. Concurrent irradiation with the anti-programmed cell death ligand-1 immune checkpoint blocker durvalumab: single centre subset analysis from a phase 1/2 trial. Eur J Cancer. 2016;68:156–162. doi:10.1016/j.ejca.2016.09.013
43. Magnuson WJ, Yeung JT, Guillod PD, Gettinger SN, Yu JB, Chiang VL. Impact of deferring radiation therapy in patients with epidermal growth factor receptor-mutant non-small cell lung cancer who develop brain metastases. Int J Radiat Oncol Biol Phys. 2016;95(2):673–679. doi:10.1016/j.ijrobp.2016.01.037
44. Magnuson WJ, Lester-Coll NH, Wu AJ, et al. Management of brain metastases in tyrosine kinase inhibitor-naïve epidermal growth factor receptor-mutant non-small-cell lung cancer: a retrospective multi-institutional analysis. J Clin Oncol. 2017;35(10):1070–1077. doi:10.1200/jco.2016.69.7144
45. Ou SH, Klempner SJ, Azada MC, Rausei-Mills V, Duma C. Radiation necrosis presenting as pseudoprogression (PsP) during alectinib treatment of previously radiated brain metastases in ALK-positive NSCLC: implications for disease assessment and management. Lung Cancer (Amsterdam, Netherlands). 2015;88(3):355–359. doi:10.1016/j.lungcan.2015.03.022
46. Mak KS, Gainor JF, Niemierko A, et al. Significance of targeted therapy and genetic alterations in EGFR, ALK, or KRAS on survival in patients with non-small cell lung cancer treated with radiotherapy for brain metastases. Neuro Oncol. 2015;17(2):296–302. doi:10.1093/neuonc/nou146
47. Shaverdian N, Lisberg AE, Bornazyan K, et al. Previous radiotherapy and the clinical activity and toxicity of pembrolizumab in the treatment of non-small-cell lung cancer: a secondary analysis of the KEYNOTE-001 phase 1 trial. Lancet Oncol. 2017;18(7):895–903. PubMed PMID: 28551359; PubMed Central PMCID: PMCPMC5538772. doi:10.1016/s1470-2045(17)30380-7
48. Gadgeel SM, Lukas RV, Goldschmidt J, et al. Atezolizumab in patients with advanced non-small cell lung cancer and history of asymptomatic, treated brain metastases: exploratory analyses of the phase III OAK study. Lung Cancer (Amsterdam, Netherlands). 2019;128:105–112. PubMed PMID: 30642441. doi:10.1016/j.lungcan.2018.12.017
49. Patruni S, Khattab A, Abel S, et al. A comparative analysis of survival in patients with non-small cell lung cancer with brain metastases receiving intracranial radiation with and without immunotherapy. J Clin Oncol. 2019;37(15_suppl):9025. doi:10.1200/JCO.2019.37.15_suppl.9025
50. Hendriks LEL, Henon C, Auclin E, et al. Outcome of patients with non-small cell lung cancer and brain metastases treated with checkpoint inhibitors. J Thor Oncol. 2019;14(7):1244–1254. PubMed PMID: 30780002. doi:10.1016/j.jtho.2019.02.009
51. Shepard MJ, Xu Z, Donahue J, et al. Stereotactic radiosurgery with and without checkpoint inhibition for patients with metastatic non-small cell lung cancer to the brain: a matched cohort study. J Neurosurg. 2019:1–8. PubMed PMID: 31349225. doi:10.3171/2019.4.Jns19822
52. Singh C, Qian JM, Yu JB, Chiang VL. Local tumor response and survival outcomes after combined stereotactic radiosurgery and immunotherapy in non-small cell lung cancer with brain metastases. J Neurosurg. 2019;132(2):512–517. PubMed PMID: 30771783. doi:10.3171/2018.10.Jns181371
53. Chen L, Douglass J, Kleinberg L, et al. Concurrent immune checkpoint inhibitors and stereotactic radiosurgery for brain metastases in non-small cell lung cancer, melanoma, and renal cell carcinoma. Int J Rad Oncol Biol Phys. 2018;100(4):916–925. PubMed PMID: 29485071. doi:10.1016/j.ijrobp.2017.11.041
54. Pike LRG, Bang A, Ott P, et al. Radiation and PD-1 inhibition: favorable outcomes after brain-directed radiation. Radiother Oncol. 2017;124(1):98–103. PubMed PMID: 28662869. doi:10.1016/j.radonc.2017.06.006
55. Kotecha R, Kim JM, Miller JA, et al. The impact of sequencing PD-1/PD-L1 inhibitors and stereotactic radiosurgery for patients with brain metastasis. Neuro-Oncology. 2019;21(8):1060–1068. PubMed PMID: 30796838. doi:10.1093/neuonc/noz046
56. World Medical Association. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310(20):2191–2194. PubMed PMID: 24141714. doi:10.1001/jama.2013.281053.
57. von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008;61(4):344–349. PubMed PMID: 18313558. doi:10.1016/j.jclinepi.2007.11.008
58. Eisenhauer EA, Therasse P, Bogaerts J, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer. 2009;45(2):228–247. PubMed PMID: 19097774. doi:10.1016/j.ejca.2008.10.026
59. Khan M, Zhao Z, Arooj S, Zheng T, Liao G. Lapatinib plus local radiation therapy for brain metastases from HER-2 positive breast cancer patients and role of trastuzumab: a systematic review and meta-analysis. Front Oncol. 2020;10:2315. doi:10.3389/fonc.2020.576926
60. Khan M, Zhao Z, Arooj S, Liao G. Impact of Tyrosine Kinase Inhibitors (TKIs) combined with radiation therapy for the management of brain metastases from renal cell carcinoma. Front Oncol. 2020;10:1246. doi:10.3389/fonc.2020.01246
61. Ahmed KA, Kim S, Arrington J, et al. Outcomes targeting the PD-1/PD-L1 axis in conjunction with stereotactic radiation for patients with non-small cell lung cancer brain metastases. J Neurooncol. 2017;133(2):331–338. PubMed PMID: 28466250. doi:10.1007/s11060-017-2437-5
62. Lesueur P, Escande A, Thariat J, et al. Safety of combined PD-1 pathway inhibition and radiation therapy for non-small-cell lung cancer: a multicentric retrospective study from the GFPC. Cancer Med. 2018;7(11):5505–5513. PubMed PMID: 30311424; PubMed Central PMCID: PMCPMC6247050. doi:10.1002/cam4.1825
63. Schapira E, Hubbeling H, Yeap BY, et al. Improved overall Survival and locoregional disease control with concurrent PD-1 pathway inhibitors and stereotactic radiosurgery for lung cancer patients with brain metastases. Int J Radiat Oncol Biol Phys. 2018;101(3):624–629. PubMed PMID: 29678530. doi:10.1016/j.ijrobp.2018.02.175
64. Koenig JL, Shi S, Sborov K, et al. Adverse radiation effect and disease control in patients undergoing stereotactic radiosurgery and immune checkpoint inhibitor therapy for brain metastases. World Neurosurg. 2019;126:e1399–e411. PubMed PMID: 30902777. doi:10.1016/j.wneu.2019.03.110
65. Sprowls SA, Arsiwala TA, Bumgarner JR, et al. Improving CNS delivery to brain metastases by blood–tumor barrier disruption. Trends Cancer. 2019;5(8):495–505. doi:10.1016/j.trecan.2019.06.003
66. Gerber DE, Urbanic JJ, Langer C, et al. Treatment design and rationale for a randomized trial of cisplatin and etoposide plus thoracic radiotherapy followed by nivolumab or placebo for locally advanced non-small-cell lung cancer (RTOG 3505). Clin Lung Cancer. 2017;18(3):333–339. PubMed PMID: 27923550; PubMed Central PMCID: PMCPMC5406261. doi:10.1016/j.cllc.2016.10.009
67. Iyengar P, Gerber DE. Locally advanced lung cancer: an optimal setting for vaccines and other immunotherapies. Cancer j. 2013;19(3):247–262. PubMed PMID: 23708072. doi:10.1097/PPO.0b013e318292e51a
68. Dovedi SJ, Adlard AL, Lipowska-Bhalla G, et al. Acquired resistance to fractionated radiotherapy can be overcome by concurrent PD-L1 blockade. Cancer Res. 2014;74(19):5458–5468. PubMed PMID: 25274032. doi:10.1158/0008-5472.Can-14-1258
69. Khan M, Lin J, Liao G, et al. Comparative analysis of immune checkpoint inhibitors and chemotherapy in the treatment of advanced non-small cell lung cancer: a meta-analysis of randomized controlled trials. Medicine. 2018;97(33):e11936. doi:10.1097/md.0000000000011936
70. Sedgwick P. Retrospective cohort studies: advantages and disadvantages. BMJ. 2014;348:g1072. doi:10.1136/bmj.g1072
71. Wang G-Z, Zhang L, Zhao X-C, et al. The Aryl hydrocarbon receptor mediates tobacco-induced PD-L1 expression and is associated with response to immunotherapy. Nat Commun. 2019;10(1):1125. doi:10.1038/s41467-019-08887-7
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
