Back to Journals » Patient Preference and Adherence » Volume 16
Anti-Hyperglycemic Medication Adherence and Health Services Utilization in People with Diabetes: A Longitudinal Study of Alberta’s Tomorrow Project
Authors Ye M, Vena JE, Johnson JA, Shen-Tu G, Eurich DT
Received 15 February 2022
Accepted for publication 13 May 2022
Published 11 June 2022 Volume 2022:16 Pages 1457—1467
DOI https://doi.org/10.2147/PPA.S362539
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Ming Ye,1 Jennifer E Vena,2 Jeffrey A Johnson,1 Grace Shen-Tu,2 Dean T Eurich1
1School of Public Health, University of Alberta, Edmonton, Alberta, Canada; 2Alberta’s Tomorrow Project, CancerCare Alberta, Alberta Health Services, Calgary, Alberta, Canada
Correspondence: Dean T Eurich, School of Public Health, University of Alberta, Canada, Email [email protected]
Background: Little is known about the long-term (> 2 years) relationship between the time-varying drug adherence and healthcare utilization for patients with diabetes.
Objective: To characterize the relationship between time-varying anti-hyperglycemic medication adherence and healthcare utilization in patients with diabetes, using data from Alberta’s Tomorrow Project, a population-based cohort study in Alberta, Canada.
Methods: Incident cases of diabetes with at least 24 months of follow-up were included in the study. Anti-hyperglycemic drug adherence was measured by proportion of days covered (PDC) in the past 12 months for each year after diagnosis. The rate of healthcare utilization was assessed for the subsequent 12 months, 36 months and 60 months. A time-varying, negative binomial generalized estimating equation model was used to examine the association between medication adherence and healthcare utilization.
Results: Among 2155 incident cases of diabetes, average age at diagnosis was 59.6± 9.3, 51.0% were female and average duration of follow-up was 7.3± 3.7 (range, 2.0– 16.2) years. The proportion of patients taking anti-hyperglycemic medications was 47.6% during the first year of diagnosis, which increased to 77.3% by the end of follow-up. Compared to adherent patients (PDC≥ 0.8), non-adherent patients (PDC< 0.8) had substantially higher rate of all-cause hospitalization [incident rate ratio, IRR=1.48 (1.22– 1.79), ED visits [1.30 (1.15– 1.47)] and GP visits [1.17 (1.08– 1.27)] in the subsequent 12 months. However, these associations became weaker with longer follow-up [eg, IRR=1.18 (0.98– 1.39) and 1.05 (0.94– 1.18) for all-cause hospitalization in the subsequent 36 and 60 months, respectively].
Conclusion: Poor adherence among diabetic patients was associated with substantially higher rate of healthcare utilization in the short term (eg, 12 months); however, this association weakened over a longer period (eg, 36– 60 months).
Keywords: diabetes, anti-hyperglycemia, adherence, time-varying, healthcare, longitudinal
Background
Anti-hyperglycemic medication is critical for diabetes control and management. Failure to maintain adherence to anti-hyperglycemic medication often leads to worse health outcomes, such as poor glycemic control,1 higher level of LDL cholesterol,2 higher systolic and diastolic blood pressure3 and increased risk of cardiovascular diseases.4 The risk of all-cause mortality in non-adherent patients has been reported to be approximately 50% higher than in adherent patients.5
Non-adherent patients also require higher amount of healthcare compared to adherent patients. Using administrative claim data in the US, Lau et al have shown that the risk of being admitted to hospital was approximately 1.5 times higher in patients non-adherent to anti-hyperglycemic medication.6 Other than hospitalization, the rate of outpatient care visits7,8 and emergency room (ER) visits8 are also remarkably higher in non-adherent diabetes patients than adherent patients. A systematic review of economic impact of medication adherence has suggested that poor adherence to anti-hyperglycemic medication was associated with increased cost in almost every aspect of healthcare, especially in care of patients with related complications.9
While adherence to anti-hyperglycemic medication has noticeable benefit for diabetes control and management, poor adherence is documented to be common among patients with diabetes. A meta-analysis of 70 observational studies has estimated that the prevalence of adhering to anti-hyperglycemic medication was ranged from 38% to 93% in patients with diabetes10 and the average medication possession rate (MPR) was approximately 75% over a 12-month period for diabetes patients.11 More importantly, adherence to anti-hyperglycemic medication should be a continuing effort for disease management and maintaining drug adherence over time is essential for achieving better long-term outcomes for diabetes patients.12
Research on health behaviors and associated factors have suggested the ongoing and time-varying nature of medication adherence.12,13 However, only a few studies have documented the trajectory of anti-hyperglycemic medication status, including the time-varying nature of drug adherence,12,14,15 and very few have characterized its long-term (>2 years) relationship with health outcomes for patients with diabetes.4,16,17 Moreover, only few, if any, have been able to account for lifestyle factors in their analysis. In this study, we used data from Alberta’s Tomorrow Project (ATP), a population-based cohort study of chronic diseases in Alberta, Canada, linked with Alberta Health (AH) administrative healthcare and medication dispense databases, to characterize the longitudinal pattern of potentially time-varying adherence to anti-hyperglycemic drugs and its relationship with healthcare utilization for patients with diabetes, over 15 years following the diagnosis.
Methods
Study Design
We conducted a longitudinal cohort study to characterize the association between time-varying anti-hyperglycemic medication adherence and healthcare utilization for patients with diabetes, using data from ATP and the linked administrative healthcare data. We also structured our manuscript and reported our results following the STROBE (Strengthening the Reporting of Observational studies in Epidemiology) guidelines.18 Supplementary Figure S1 shows the study design and the timeline of time-varying exposure (medication adherence status) and outcome (healthcare utilization) measurement. ATP participants with diabetes were followed from the date of diagnosis (index date) to March 31, 2018 (or until death).
Study Participants
In 2000–2008, ATP randomly recruited a total of 29,876 participants aged 35–69 years, living in Alberta, Canada, with no history of cancer other than non-melanoma skin cancer at the time of enrollment, to explore how lifestyle, genetics and environment influence the health and wellbeing of Albertan. All these 29,876 ATP participants had completed the ATP baseline health and lifestyle questionnaires and provided valid written consent to data linkage to administrative healthcare data and use of the linked health data in research at the time of enrollment. For this study, 2467 incident cases of diabetes (ie, diabetes diagnosed after enrollment in ATP) were identified in this ATP cohort, among which 2155 incident cases with at least 24 months of follow-up after diagnosis until March 31, 2018 (the end of the study) were included in the final analysis.
Data Sources
Alberta Health (AH) administrative datasets utilized in this study include all drug dispense records from Alberta Blue Cross (ABC) and Pharmaceutical Information Network (PIN) and health services records from Ambulatory Care, Inpatient and Practitioner/Physician Claims datasets. Detailed descriptions of AH administrative datasets for research can be obtained from Alberta Health (http://www.health.alberta.ca/initiatives/health-research.html). Individual-level AH administrative data from October 1, 2000-March 31, 2018 were linked to the ATP cohort using the unique identifier Personal Health Number (PHN) provided by participants during the consent process. After data linkage, AH healthcare data were de-identified before release to the authors of this study.
Other than the linked AH healthcare data, a wide range of information on exposures and risk factors for chronic diseases, including sociodemographic and socio-economic factors, anthropometrics and lifestyle behaviors (eg, diet history and physical activities), were self-reported by the ATP participants using well-validated questionnaire, including the Canadian Dietary History Questionnaire (CDHQ)19 and Past-Year Total Physical Activity Questionnaire (PYTPAQ),20 at time of enrollment. Detailed information on the ATP self-administered questionnaires can be found at www.myATP.ca.
Diabetes Cases
Diabetes cases were identified using a modified version of the well-validated Canadian National Diabetes Surveillance System (NDSS) algorithm:21
One hospitalization record with an ICD code of diabetes (ICD-9: 250, ICD-10: E10-E14) OR two physician claims within two years with an ICD code of diabetes OR self-report by participants, plus any of the following conditions: i) one hospitalization with ICD code for diabetes, ii) one physician claim with ICD code for diabetes, or iii) one diabetes medication with Anatomical Therapeutic Chemical Classification (ATC) code for insulin (A10A) or glucose-lowering drugs [A10B]
The index date of diabetes was determined by the earliest date of medical records that contribute to the case definition. Cases were identified as “incident” only if the index date was more than 6 months after ATP enrollment to ensure true incident cases were identified for the study.
Anti-Hyperglycemic Drug Adherence
We used drug prescription records to compute proportion of days covered (PDC) as measurement of drug adherence.22 Specifically, anti-hyperglycemic drug prescription records were identified using the ATC code of A10 in the linked ABC and PIN datasets. For each chemical class of drugs (lowest level of ATC code), PDC was calculated as a ratio of the number of days covered by the medication (based on days supplied) divided by the total number of days within the specified time window (eg, in the past 12 months or in the cumulative number of months since index date).22 A gap of less than 60 days was allowed for being considered as persistent treatment.23 The mean PDC was obtained by dividing the summed PDC of each anti-hyperglycemic drug class over the total number of drug classes.24 A dichotomized variable was generated based on the value of mean PDC to indicate adherence (PDC ≥ 0.8) vs non-adherence (PDC < 0.8) as is routinely done in health services research.25 A third category of “no medication” was also used for individuals who were patients with diabetes but did not have anti-hyperglycemic medication records (eg, some patients may have used diet and lifestyle efforts to control diabetes). As medication adherence may potentially change over time, we estimated adherence using a time-varying approach. Specifically, the patient’s anti-hyperglycemic medication status (no medication, adherent or non-adherent) was updated every 12 months, beginning from the date of diagnosis (index date), for each year following the diagnosis. The estimated medication adherence was then used to predict the subsequent rate of healthcare utilization.
Healthcare Utilization Variables
All-cause hospitalization was defined as any hospital admission within the linked hospital discharge abstract data (DAD). Diabetes-specific hospitalization was identified by ICD code of diabetes (ICD-9: 250 or ICD-10: E10-E14) as the most responsible condition for hospitalization. Hospitalization for ambulatory care sensitive (ACS) conditions was identified by ICD codes of a set of 28 ACS conditions.26 ED visit was identified using Alberta Management Information System (MIS) codes (71310, 71313 and 71314) in the linked AH ambulatory care dataset. Primary care visits were identified using specialty group codes in Practitioner/Physician Claims data for a visit to a general practitioner (GP) or a specialist in an outpatient environment (eg, at physician’s office). The rate of healthcare utilization was calculated as a ratio of the number of health services encounters divided by the total person-years for a subsequent period. Specifically, we evaluated whether anti-hyperglycemic medication adherence was associated with healthcare utilization within the subsequent period (eg, 12 months) of follow-up in a rolling time-varying manner (ie, year 1 adherence was used to predict year 2 healthcare utilization, then year 2 adherence was used to predict year 3 healthcare utilization).
Statistical Analysis
The baseline characteristics of study participants and rate of healthcare utilization were summarized based on participants’ anti-hyperglycemic medication adherence status (no medication, adherent or no adherent). Means and standard deviations were calculated for continuous variables; proportions were calculated for categorical variables; incidence rates (density) were calculated for person-year data. Comparisons between groups were made using Student’s t-test for continuous variables and χ2 test for categorical variables and incidence rates.
The association between the time-varying anti-hyperglycemic medication adherence status and rate of healthcare utilization was examined using generalized estimating equation (GEE) model, with medication status as the time-varying exposure variable, the number of health services encounters in the subsequent 12 months as the outcome variable, and person-year as the offset variable. In our study, the outcome variables were measured repeatedly in every 12 months for each patient, which potentially leads to “within-subject” correlation for the outcome. Therefore, we chose to use GEE model, a semiparametric model with Huber–White “sandwich” estimator, to estimate the population average effect after controlling the “within-subject” correlation.27 In addition, given a large number of patients with no events (ie, zero inflated count data with over-dispersion), a negative binomial distribution was assumed in the GEE model.
Incident rate ratio (IRR) and 95% CIs were computed after adjusting for the following covariates in the GEE model: age at diagnosis (35–44 years, 45–64 years, 65+ years), sex (male/female), ethnicity (Caucasian vs other), living in rural vs urban areas, education attainment (secondary or less, some post-secondary, post-secondary), body mass index (BMI) categories (under/normal weight ≤24.9 kg/m2, overweight 25.0–29.9 kg/m2, obese ≥30.0 kg/m2), smoking status (yes/no), physically active (yes/no, based on whether or not accumulating at least 210 min moderate-to-vigorous intensity recreational physical activities per week in the past 12 months),28 tertiles of Healthy Eating Index for diet quality assessment,29 and time-varying covariates (healthcare utilization and Elixhauser comorbidities [0, 1–2, 2+] in the past 12 months).30 For participants who had missing values in these covariates (Supplementary Table S1), a “missing indicator” category was created to ensure all participants were included and results were minimally affected by missing values.
We also undertook several additional analyses to evaluate the robustness of our main results: 1) instead of measuring adherence in the past 12 months, PDC was calculated over the cumulative number of months for each year after diagnosis (eg, adherence over years 1–5 following diagnosis were used to predict year 6 adherence as opposed to just 12 months prior); 2) assessing the impact of drug adherence on subsequent healthcare utilization for a longer period (eg, 36 or 60 months vs 12 months in the primary analysis) with a subgroup of patients with at least 72 months of follow-up; 3) other than unadjusted and fully adjusted models, relevant covariates were progressively adjusted in the regression analysis, from basic demographic factors (age, sex, urban/rural) and standard administrative health records (co-mortifies and prior healthcare use) to difficult-to-capture patient characteristics (ethnicity, education attainment and BMI) and lifestyle factors (smoking, physical activity, and diet quality), to evaluate the relative potential of confounding effect, including the healthy user bias. All statistical analyses, with significant level at alpha=0.05, were conducted using STATA®14 software.
Results
Characteristics of Study Participants
This longitudinal cohort study included 2155 incident cases of diabetes with an average (SD) follow-up of 7.3 (3.7) years (range 2.0–16.2 years) from diagnosis to March 31, 2018 (or death). The baseline characteristics of study participants were summarized based on anti-hyperglycemic medication adherence status in the first 12 months of diagnosis (Supplementary Table S1). The average (SD) age at incidence was 59.6 (9.3) years and 51.0% of the participants are women. The majority (87.1%) of participants self-reported as being of Caucasian ethnicity and 27.2% of the participants lived in rural areas. Overall, there was a higher percentage of non-adherent patients living in rural areas, with more comorbid conditions and higher rates of hospitalization, ED visits and GP visits in the first 12 months following diagnosis (Supplementary Table S1).
Anti-Hyperglycemic Drug Adherence Profile
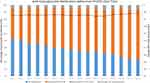
During the follow-up period after diagnosis (up to 16 years), the percentage of patients taking anti-hyperglycemic medications increased over time (p-value <0.01 for trend test), from 47.6% in the first 12 months up to 77.3% in the final year of follow-up (Figure 1). In addition, in patients who took anti-hyperglycemic medications, the average PDC and the ratio of adherent vs non-adherent patients did not significantly change over time after diagnosis (Figure 1).
Anti-Hyperglycemic Drug Adherence and Healthcare Utilization
Even though the adherence to anti-hyperglycemic drugs may change over time (Figure 1), patients with diabetes who did not take any anti-hyperglycemic medications in the past 12 months had a significantly lower (p-value <0.01) rate of healthcare utilization in the subsequent 12 months, compared to patients who did take the medications (except for all-cause hospitalization, Table 1). In unadjusted analyses, compared to the adherent patients, non-adherent patients had a significantly higher rate of all-cause hospitalization (0.260 vs 0.162 per person-year), diabetes-specific hospitalization (0.030 vs 0.004 per person-year), hospitalization for ACS conditions (0.052 vs 0.021 per person-year), ED visits (1.042 vs 0.729 per person-year) and GP visits (8.684 vs 7.800 per person-year); all p-values <0.01 (Table 1). Similar to the 12 months results, non-adherent patients also had higher rates of health services utilization compared to adherent patients in the subsequent 36 (or 60) months (Supplementary Tables S2).
 |
Table 1 Rate of Healthcare Utilization in the Subsequent 12 Months by Anti-Hyperglycemic Medication Status (n=2155)† |
In multivariable regression models, any use of anti-hyperglycemic drugs during the past 12 months, irrespective of adherence status, was associated with higher rates of healthcare utilization in the subsequent 12 months (Table 2). In addition, compared to adherent patients, non-adherent patients had substantially higher rates of all-cause hospitalization (IRR=1.48, 95% CI=1.22–1.79), diabetes-specific hospitalization (IRR=4.73, 95% CI=2.38–9.40), hospitalization for ACS conditions (IRR=2.01, 95% CI=1.31–3.07), ED visits (IRR=1.30, 95% CI=1.15–1.47) and GP visits (IRR=1.17, 95% CI=1.08–1.27) in the subsequent 12 months (Table 2).
Additional analyses using PDC calculated from a cumulative number of months since diagnosis showed similar results, compared to the main analysis with PDC calculated within any of the time segments of past 12 months. Moreover, in a sub-cohort study of patients with at least 72 months of follow-up, rates of healthcare utilization in the subsequent 36 or 60 months was still significantly higher in patients using anti-hyperglycemic medication compared to patients not taking medications (data available upon request). However, in examining the relationship between drug adherence and healthcare utilization in the subsequent 36 or 60 months, the observed associations were weaker (eg IRR=1.18 [0.98–1.39] and 1.05 [0.94–1.18] for all-cause hospitalization and IRR=1.12 [0.99–1.27] and 1.07 [0.96–1.18] for ED visits in the subsequent 36 months and 60 months, respectively) (Table 3). In multivariable regression analyses with covariates progressively adjusted in the model, no appreciable changes were observed in IRR, although there was a relative smaller IRR when lifestyle factors (eg, physical activities and diet quality) and other difficult-to-capture patient characteristics (eg, BMI and education attainment) were adjusted (Supplementary Figure S2).
 |
Table 3 Past 12 Months Drug Adherence and Healthcare Utilization in the Subsequent 12, 36 and 60 Months: Sub-Group Analysis of Patients with at Least 72 Months of Follow-Up* |
Discussion
This longitudinal cohort study showed that after taking into account the potential time-varying impact, poor adherence to anti-hyperglycemic medication was still associated with substantially higher rates of healthcare utilization, including hospitalization, ED visits and GP visits, in the subsequent 12 months. However, this association became much weaker over longer period of follow-up (eg, 36 or 60 months). This observation may be related to the notion that tighter glycemic control has not shown to prevent downstream complications of diabetes during the long term (unless HbA1c is maintained to the level of <6.5% or 48 mmol/mol).31
In the previous studies in the literature, for the short-term impact (typically 12 months), similar to our study, many observational investigations have shown a significant protective effect of anti-hyperglycemic drug adherence.3,6,32–34 However, mixed results have been reported on the long-term impact of anti-hyperglycemic drug adherence and outcomes of diabetes. A randomized trial study conducted by the Action to Control Cardiovascular Risk in Diabetes (ACCORD) study group showed that compared to standard therapy, intensive anti-glycemic therapy, which requires high medication adherence, can achieve better control of glycated hemoglobin levels, but did not significantly reduced major cardiovascular events (hazard ratio=0.90, 95% CI: 0.78–1.04) over a period of 3.5 years.31 A longer-term follow-up (~9 years) of the surviving ACCORD participants also showed that there was a neutral effect of intensive anti-glycemic treatment on the composite outcome and all-cause mortality (hazard ratio=1.01, 95% CI: 0.92–1.10) in the long run. Conversely, during 30 years of follow-up in Diabetes Control and Complications Trial (DCCT)/Epidemiology of Diabetes Interventions and Complications (EDIC) study, intensive anti-diabetic treatment significantly reduced incidence of cardiovascular diseases by 30% (95% CI: 0.07–0.48) in type 1 diabetes. Moreover, a national cohort study of type 2 diabetes patients in Sweden showed that the risk of all-cause mortality was similar between patients with different levels of drug adherence, although the risk of cardiovascular diseases was lower in adherent patients.35 These studies, including ours, suggest that the beneficial impact of anti-hyperglycemic medications, including good adherence to medications, could be diminished over the long term; other factors, such as developing related complications (eg, cancer and cardiovascular diseases)36,37 and potential therapeutic inertia,38,39 may weaken the effectiveness of anti-hyperglycemic medications. Given the potential decline of the degree of benefit from anti-hyperglycemic treatment over time reported in our study, continuing effort of monitoring HbA1c level, timely intensification of anti-hyperglycemic treatment and effective control of related complications (such as CVD), should be enhanced in practice to gain better outcomes for patients with diabetes in the long run.
We also postulate that the reported short-term effect3,6,32–34 may be due to some uncontrolled confounding factors, potentially the healthy-user effect.40 Our data showed that patients adherent to anti-hyperglycemic medications, were more physically active, with higher diet quality, tended to be non-smokers and with fewer comorbid conditions and healthcare encounters at the baseline, compared to the non-adherent group, indicating adherent patients might be healthy users. However, in our multivariable regression models, in addition to socio-demographic factors (eg, age and sex) and standard clinical records from administrative data (eg, prior healthcare use and comorbidities), factors that potentially lead to healthy user bias, including education attainment and lifestyle behaviors (smoking status, physical activities and diet quality), were fully controlled to reduce bias from these confounders. Thus, healthy-user bias is less likely a factor in the results observed in the study, although it is still possible that some unknown/unmeasured patient’s characteristics or life events, which we could not control for, were influencing patient’s subsequent healthcare utilization.
The strength of our study includes linking and co-analyzing population-based cohort data with administrative healthcare data in characterizing the longitudinal impact of anti-glycemic drug adherence on healthcare utilization over 15 years. Compared to previous similar studies,3,6,32,33 this study, with difficult-to-capture lifestyle and other patient data (eg, education attainment and BMI) from the ATP, was able to control a wider range of confounding effects, including the potential healthy user bias, to make a more accurate estimation of the association. Another strength of our study is to consider drug adherence as a time-varying exposure variable when examining the association between drug adherence and subsequent healthcare utilization, which helps to avoid person-time related misclassification of exposure variables.41
Despite these strengths, there are several limitations in our study. First, although ATP participants were randomly recruited from Alberta’s general population, compared to the general population in Alberta, the ATP participants are older, with more women and living a relative healthy lifestyle.42 Results of our study might not be generalized to general populations in Canada. However, given the high internal validity (eg, fairly large number of participants and adjusting for a wide range of potential confounders), our study provides a better understanding of the longitudinal relationship between anti-hyperglycemic drug adherence and subsequent healthcare utilization. Secondly, while administrative health data is a useful data source for drug prescription records and related epidemiology studies, prescription records-based calculation of PDC is considered as an indirect measurement of drug adherence. However, compared to direct measures (eg, pill counts), prescription records-based measurement is more objective and reliable.43 In addition, potential data linkage and secondary analysis of these prescription records makes it more feasible to study drug adherence for large population-based cohort, compared to direct measures.
Conclusions
By linking administrative health data to the ATP cohort, our study shows that adherence to anti-hyperglycemic medications was substantially associated with reduced healthcare utilization in short term (12 months); however, this association becomes weaker for a longer period of follow-up (36–60 months). Results of this study, which will benefit not only the ATP participants, provide a cautionary new piece of evidence in the literature on how anti-hyperglycemic medications would affect outcomes of diabetes. Future research exploring why the beneficial effect of anti-hyperglycemic medication seems to be plateaued over a longer term is warranted.
Abbreviations
ABC, Alberta Blue Cross; ACCORD, Action to Control Cardiovascular Risk in Diabetes; ACS, Ambulatory Care Sensitive; AH, Alberta Health; ATC, Anatomical Therapeutic Chemical Classification; ATP, Alberta’s Tomorrow Project; BMI, body mass index; CI, confidence interval; DAD, discharge abstract data; DCCT, diabetes control and complications trial; ED, emergency department; EDIC, epidemiology of diabetes interventions and complications; GEE, generalized estimating equation; GP, general practitioner; IRR, incident rate ratio; MIS, management information system; NDSS, National Diabetes Surveillance System; PDC, proportion of days covered; PHN, personal health number; PIN, pharmaceutical information network; SD, standard deviation.
Data Sharing Statement
To comply with the Alberta Health (AH) Health Information Policy and Alberta Tomorrow Project (ATP) data disclosure guidelines, datasets used in this study are not available for readers.
Ethics Statement and Consent to Participate
This study was approved by the Health Research Ethics Board of the University of Alberta (study ID Pro00058561). This study also complied with the Declaration of Helsinki. All participants of this study have provided valid written consent for data linkage with administrative healthcare and other health-related data. The storage, use and disposition of participants’ data in this study complies with the Personal Information Protection and Electronic Documents Act (PIPEDA) in Canada.
Consent for Publication
All authors of this study have read the manuscript, accepted responsibility for the content of manuscript, consented for publication.
Acknowledgments
This study is based in part on data provided by Alberta Health. The interpretation and conclusions contained herein are those of the researchers and do not necessarily represent the views of the Government of Alberta. Neither the Government nor Alberta Health express any opinion in relation to this study. Alberta’s Tomorrow Project is only possible due to the commitment of its research participants, its staff and its funders: Alberta Health, Alberta Cancer Foundation, Canadian Partnership Against Cancer and Health Canada, and substantial in-kind funding from Alberta Health Services. The views expressed herein represent the views of the authors and not of Alberta’s Tomorrow Project or any of its funders. The authors declared no conflict of interest.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was supported by Alberta Health, Alberta Cancer Foundation, Canadian Partnership Against Cancer.
Disclosure
Dr Jennifer E Vena reports grants from Alberta Health, Alberta Cancer Foundation, Alberta Health Services, and the Canadian Partnership Against Cancer and Health Canada, during the conduct of the study. Dr Grace Shen-Tu reports grants from Alberta Health, during the conduct of the study. The authors declared no conflict of interest.
References
1. Egede LE, Gebregziabher M, Echols C, Lynch CP. Longitudinal effects of medication nonadherence on glycemic control. Ann Pharmacother. 2014;48(5):562–570. doi:10.1177/1060028014526362
2. Pladevall M, Williams LK, Potts LA, Divine G, Xi H, Lafata JE. Clinical outcomes and adherence to medications measured by claims data in patients with diabetes. Diabetes Care. 2004;27(12):2800–2805. doi:10.2337/diacare.27.12.2800
3. Ho PM, Rumsfeld JS, Masoudi FA, et al. Effect of medication nonadherence on hospitalization and mortality among patients with diabetes mellitus. Arch Intern Med. 2006;166(17):1836–1841. doi:10.1001/archinte.166.17.1836
4. Simpson SH, Lin M, Eurich DT. Medication adherence affects risk of new diabetes complications: a cohort study. Ann Pharmacother. 2016;50(9):741–746. doi:10.1177/1060028016653609
5. Currie CJ, Peyrot M, Morgan CL, et al. The impact of treatment noncompliance on mortality in people with type 2 diabetes. Diabetes Care. 2012;35(6):1279–1284. doi:10.2337/dc11-1277
6. Lau DT, Nau DP. Oral antihyperglycemic medication nonadherence and subsequent hospitalization among individuals with type 2 diabetes. Diabetes Care. 2004;27(9):2149–2153. doi:10.2337/diacare.27.9.2149
7. Nasseh KFS, Visaria J, Vlahiotis A, Tian Y. Cost of medication nonadherence associated with diabetes, hypertension, and dyslipidemia. Am J Pharm Benefits. 2012;4(2):e41–e47.
8. Roebuck MC, Liberman JN, Gemmill-Toyama M, Brennan,TA. Medication adherence leads to lower health care use and costs despite increased drug spending. Health Aff. 2011;30(1):91–99. doi:10.1377/hlthaff.2009.1087
9. Hajos TR, Polonsky WH, Pouwer F, Gonder-Frederick L, Snoek FJ. Toward defining a cutoff score for elevated fear of hypoglycemia on the hypoglycemia fear survey worry subscale in patients with type 2 diabetes. Diabetes Care. 2014;37(1):102–108. doi:10.2337/dc13-0971
10. Krass I, Schieback P, Dhippayom T. Adherence to diabetes medication: a systematic review. Diabetic Med. 2015;32(6):725–737. doi:10.1111/dme.12651
11. Iglay K, Cartier SE, Rosen VM, et al. Meta-analysis of studies examining medication adherence, persistence, and discontinuation of oral antihyperglycemic agents in type 2 diabetes. Curr Med Res Opin. 2015;31(7):1283–1296. doi:10.1185/03007995.2015.1053048
12. Chen CC, Cheng SH. Continuity of care and changes in medication adherence among patients with newly diagnosed diabetes. Am J Manag Care. 2016;22(2):136–142.
13. Campos LF, Glickman ME, Hunter KB. Measuring effects of medication adherence on time-varying health outcomes using Bayesian dynamic linear models. Biostatistics. 2019;22(3):662–683.
14. Donnelly LA, Doney AS, Morris AD, Palmer CN, Donnan PT. Long-term adherence to statin treatment in diabetes. Diabetic Med. 2008;25(7):850–855. doi:10.1111/j.1464-5491.2008.02476.x
15. Lindenmeyer A, Hearnshaw H, Vermeire E, Van Royen P, Wens J, Biot Y. Interventions to improve adherence to medication in people with type 2 diabetes mellitus: a review of the literature on the role of pharmacists. J Clin Pharm Ther. 2006;31(5):409–419. doi:10.1111/j.1365-2710.2006.00759.x
16. Hunt KJ, Gebregziabher M, Lynch CP, Echols C, Mauldin PD, Egede LE. Impact of diabetes control on mortality by race in a national cohort of veterans. Ann Epidemiol. 2013;23(2):74–79. doi:10.1016/j.annepidem.2012.11.002
17. Yu AP, Yu YF, Nichol MB. Estimating the effect of medication adherence on health outcomes among patients with type 2 diabetes–an application of marginal structural models. Value Health. 2010;13(8):1038–1045. doi:10.1111/j.1524-4733.2010.00787.x
18. von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008;61(4):344–349. doi:10.1016/j.jclinepi.2007.11.008
19. Csizmadi I, Kahle L, Ullman R, et al. Adaptation and evaluation of the National Cancer Institute’s Diet History Questionnaire and nutrient database for Canadian populations. Public Health Nutr. 2007;10(1):88–96. doi:10.1017/S1368980007184287
20. Friedenreich CM, Courneya KS, Neilson HK, et al. Reliability and validity of the past year total physical activity questionnaire. Am J Epidemiol. 2006;163(10):959–970. doi:10.1093/aje/kwj112
21. Public Health Agency of Canada. Report from the national diabetes surveillance system: diabetes in Canada; 2009.
22. Zongo A, Gregoire JP, Moisan J, Guenette L. Measuring adherence to oral antidiabetic multi-drug treatment: comparative validity of prescription claims-based adherence measures against hospitalization. Res Social Adm Pharm. 2019;15(6):738–743. doi:10.1016/j.sapharm.2018.09.005
23. McGovern A, Tippu Z, Hinton W, Munro N, Whyte M, de Lusignan S. Systematic review of adherence rates by medication class in type 2 diabetes: a study protocol. BMJ Open. 2016;6(2):e010469. doi:10.1136/bmjopen-2015-010469
24. Choudhry NK, Shrank WH, Levin RL, et al. Measuring concurrent adherence to multiple related medications. Am J Manag Care. 2009;15(7):457–464.
25. Karve S, Cleves MA, Helm M, Hudson TJ, West DS, Martin BC. Good and poor adherence: optimal cut-point for adherence measures using administrative claims data. Curr Med Res Opin. 2009;25(9):2303–2310. doi:10.1185/03007990903126833
26. Knight JC, Mathews M, Aubrey-Bassler K. Relation between family physician retention and avoidable hospital admission in Newfoundland and Labrador: a population-based cross-sectional study. CMAJ Open. 2017;5(4):E746–E752. doi:10.9778/cmajo.20170007
27. Armitage P, Matthews J. Statistical Methods in Medical Research. John Wiley and Sons; 2008.
28. Brown AF, Mangione CM, Saliba D, Sarkisian CA. Guidelines for improving the care of the older person with diabetes mellitus. J Am Geriatr Soc. 2003;51(5Suppl Guidelines):S265–280. doi:10.1046/j.1532-5415.51.5s.1.x
29. Garriguet D. Diet quality in Canada. Health Rep. 2009;20(3):41–52.
30. Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36(1):8–27. doi:10.1097/00005650-199801000-00004
31. Gerstein HC, Miller ME; Action to Control Cardiovascular Risk in Diabetes Study G. Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med. 2008;358(24):2545–2559.
32. Sokol MC, McGuigan KA, Verbrugge RR, Epstein RS. Impact of medication adherence on hospitalization risk and healthcare cost. Med Care. 2005;43(6):521–530. doi:10.1097/01.mlr.0000163641.86870.af
33. Juarez DT, Tan C, Davis J, Mau M. Factors affecting sustained medication adherence and its impact on health care utilization in patients with diabetes. J Pharm Health Serv Res. 2013;4(2):89–94. doi:10.1111/jphs.12016
34. Basak R, Bentley JP, McCaffrey DJ 3rd, West-Strum D, Przybyla SM, Banahan BF
35. Karlsson SA, Hero C, Svensson AM, et al. Association between refill adherence to lipid-lowering medications and the risk of cardiovascular disease and mortality in Swedish patients with type 2 diabetes mellitus: a nationwide cohort study. BMJ Open. 2018;8(3):e020309. doi:10.1136/bmjopen-2017-020309
36. Laakso M. Cardiovascular disease in type 2 diabetes from population to man to mechanisms: the Kelly West Award Lecture 2008. Diabetes Care. 2010;33(2):442–449. doi:10.2337/dc09-0749
37. Zanders MMJ, Haak HR, van Herk-Sukel MPP, van de Poll-Franse LV, Johnson JA. Impact of cancer on adherence to glucose-lowering drug treatment in individuals with diabetes. Diabetologia. 2015;58(5):951–960. doi:10.1007/s00125-015-3497-8
38. Okemah J, Peng J, Quinones M. Addressing clinical inertia in Type 2 diabetes mellitus: a review. Adv Ther. 2018;35(11):1735–1745. doi:10.1007/s12325-018-0819-5
39. Khunti K, Millar-Jones D. Clinical inertia to insulin initiation and intensification in the UK: a focused literature review. Prim Care Diabetes. 2017;11(1):3–12. doi:10.1016/j.pcd.2016.09.003
40. Eskin M, Simpson SH, Eurich DT. Evaluation of healthy user effects with metformin and other oral antihyperglycemia medication users in adult patients with Type 2 diabetes. Can J Diabetes. 2019;43(5):322–328. doi:10.1016/j.jcjd.2018.12.001
41. Austin PC. Generating survival times to simulate Cox proportional hazards models with time-varying covariates. Stat Med. 2012;31(29):3946–3958. doi:10.1002/sim.5452
42. Ye M, Robson PJ, Eurich DT, Vena JE, Xu JY, Johnson JA. Cohort profile: alberta’s tomorrow project. Int J Epidemiol. 2016;46(4):1097–8l.
43. Lam WY, Fresco P. Medication adherence measures: an overview. Biomed Res Int. 2015;2015:217047. doi:10.1155/2015/217047
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.