Back to Journals » Clinical Ophthalmology » Volume 14
Anterior Lamellar Recession versus Posterior Lamellar Tarsal Rotation for Lower Lid Trachomatous Trichiasis: A Randomized Controlled Trial
Authors Abdelaziz FM, Kamal MA, Said MM, Diab MM
Received 13 May 2020
Accepted for publication 1 July 2020
Published 22 July 2020 Volume 2020:14 Pages 2043—2050
DOI https://doi.org/10.2147/OPTH.S261783
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Fatma M Abdelaziz, Mahmoud Ahmed Kamal, Mohamed M Said, Mostafa M Diab
Department of Ophthalmology, Faculty of Medicine, Fayoum University, Al Fayoum, Egypt
Correspondence: Mostafa M Diab
Department of Ophthalmology, Faculty of Medicine, Fayoum University, 12 George Nirose St, Al Mesalla, Fayoum, Al Fayoum 63514, Egypt
Tel +20 842152290
Email [email protected]
Purpose: To compare the outcomes of anterior lamellar recession (ALR) versus posterior lamellar tarsal rotation (PLTR) procedure for the repair of lower eyelid trachomatous trichiasis (TT).
Design: Prospective randomized comparative trial.
Methods: Study Population and Interventions: Patients with lower eyelid TT were enrolled. Patients with a history of lower lid surgery, marked horizontal lid laxity, another evident cause for the trichiasis, and those under 18 years were excluded. Participants were randomized to either PLTR or ALR. The sequence was computer-generated by an independent statistician, and the allocation sequence was concealed in sealed opaque envelops. Patients were evaluated at 1 week and 1, 3, 6, and 12 months. Main Outcome Measures: postoperative trachomatous trichiasis (PTT) and cosmetic satisfaction.
Results: A total of 60 patients were randomly assigned with 30 patients in each group. Two (3.3%) participants in PLTR group did not follow up and were excluded from the analysis. At 1, 3, and 6 months, PTT was significantly more frequent in the PLTR group than the ALR group (14.3% vs 0%; p= 0.048, 25% vs 0%; p= 0.004, 35.7% vs 10%; p= 0.019, respectively). In the ALR group, 6 patients (20%) had PTT at their 12-month follow-up visit compared with 15 patients (53.6%) in the PLTR group (P = 0.008) with absolute risk reduction of 33.6% (95% (CI= 9% − 58%)). Cosmetic dissatisfaction was significantly more frequent in the ALR group at the initial follow-up visits compared to the PLTR group. However, this difference was no longer significant at 6 and 12 months follow-up.
Conclusion: These data provide strong evidence that ALR is more effective in correction of lower eyelid trachomatous trichiasis with acceptable cosmesis compared with PLTR.
Keywords: lower lid, trichiasis, anterior lamellar recession, posterior lamellar tarsal rotation
Introduction
Entropion with trichiasis is the end-stage of trachomatous scarring that occurs following recurrent conjunctival infection with chlamydia trachomatis. Untreated trachomatous trichiasis (TT) of either the upper or lower eyelids can result in irreversible visual loss from corneal opacity.1,2 World Health Organization (WHO) recommends surgery for TT as a core pillar of the SAFE strategy for trachoma elimination.3 Although recent studies have shown high prevalence of lower eyelid TT among trachoma patients, attention has been concentrated on surgery for the upper eyelids in trachoma programs.4
Various surgical techniques have been described for trachomatous trichiasis correction, nevertheless most are used to treat the upper eyelid.5 Some researchers use the tarsotomy procedure, adopted by WHO for upper eyelids to rectify lower lids.6 Tarsotomy procedures carry the advantage of being simple and easy to teach to non- ophthalmologists making it suitable in trachoma control programs; however, the overall failure rates are high.7 On the other hand, other studies have reported good results with tarsus sparing procedures.8,9
The aim of this study is to compare the outcomes of 2 different techniques for correction lower eyelid trachomatous trichiasis: posterior lamellar tarsus rotation (PLTR) and anterior lamellar recession (ALR).
Patients and Methods
This prospective, randomized, controlled, single-blinded trial with identifier PACTR201807153376731 was registered at the Pan African Clinical Trials Registry following ethics committee approval by the Fayoum University Ethics Committee (registration number: M 334/2018). The study adhered to the tenets of the Declaration of Helsinki.
Patients with lower eyelid trachomatous trichiasis were enrolled in the study from June 2018 to March 2019 after signing a written informed consent. Lower lid trachomatous trichiasis was defined as one or more rubbing lashes in the presence of characteristic trachomatous scarring of both upper and lower tarsal conjunctiva, post trachomatous degenerations and concretions, and superior corneal pannus with Herbert’s pits. Patients with a history of lower lid surgery, marked horizontal lid laxity, another evident cause for the trichiasis, such as autoimmune diseases, trauma, or severe blepharitis, and those under 18 years were excluded. Eligible patients were randomized to either to PLTR or to ALR. The sequence was computer-generated by an independent statistician, and the allocation sequence was concealed in sealed opaque envelops.
A complete preoperative ocular examination was performed including slit lamp examination of the cornea with fluorescein staining, eyelid margin, and tarsal conjunctiva. The number, type (misdirected, metaplastic, entropic, and mixed)2 and location of pathologic lashes were determined. According to the number of lashes touching the globe, trichiasis was subdivided into major TT (6 or more rubbing lashes) and minor TT (five or less). Trichiasis was classified as corneal, conjunctival, and combined based on where the lashes touched the globe in the primary gaze position. The lid margin position was graded as normal, marginal entropion (rounding of the posterior lid margin edge and anteriorization of the mucocutaneous junction), and frank entropion.
Surgical Technique
All surgeries were performed by a single surgeon (MMD) who has good experience in performing lower lid TT procedures. The surgery was performed under local anesthesia with intravenous sedation using 3x binocular loupes. The surgical technique was completed as per standard protocols.6,10,11 Briefly, in the ALR a gray-line incision is made along the length of the lower eyelid using a Bard-Parker No. 11 blade from the lateral canthus to just lateral to the lacrimal punctum. In cases of metaplastic lashes, the incision was performed in a more posterior location along the lid margin. Complete lamellar division with exposure of lower lid retractors is then performed. Three mattress sutures (repositioning sutures) are passed through the lower lid retractors and brought through anterior lamella at higher level below the lash line. The anterior lamella is sutured to the anterior tarsal surface using 3 to 4 interrupted 6-0 mattress sutures leaving 2 mm of bare tarsus (Supplementary Figure 1). For PLTR, the eyelid is everted, a full-thickness incision is made through the tarso-conjunctival layer, parallel to and 2 mm below the lid margin. The posterior lamella is separated from the anterior lamella (skin and orbicularis muscle). Three horizontal mattress 6-0 vicryl sutures are placed to externally rotate the distal tarsus (Supplementary Figure 2).
Patients were examined at 7–10 days, 1, 3, 6 and 12 months after surgery. At 1st follow up visit, participants were assessed for postoperative trichiasis, degree of lid eversion, any complications, and improvement in subjective discomfort before suture removal. Cosmetic satisfaction was evaluated at 1, 3, 6, and 12 months. Patients were asked about cosmetic acceptability of the results of the procedure (satisfied, indifferent, and dissatisfied). Postoperative trachomatous trichiasis (PTT) was defined as 1 or more eyelashes touching the globe and/or evidence of epilation at any follow-up visit. The outcomes were evaluated by the first author who was not involved in the surgery.
Results
A total of 60 patients with lower eyelid trichiasis were enrolled and randomly assigned with 30 patients in each group. Two (3.3%) participants in PLTR group did not follow-up and therefore were excluded from the analysis. In bilateral cases, the right eyelid was used for analysis. Thirty-eight patients were female (65.5%). The mean age was 61.02± 11.1 (range: 20–78 years). Table 1 shows the patient characteristics, including age, gender, preoperative number, location, and type of trichiatic lashes, and the presence of upper lid trichiasis in each study group. No statistical difference was noted between the groups regarding baseline demographic and clinical characteristics (Table 1).
 |
Table 1 Demographic and Clinical Characteristics of Participants in Both Groups of the Study |
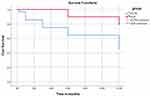
At one week postoperatively, PTT was present in one eyelid in the PLTR group and none in the ALR group. At 1, 3, and 6 months, PTT was significantly more frequent in the PLTR group than the ALR group (14.3% vs 0%; p= 0.048, 25% vs 0%; p= 0.004, 35.7% vs 10%; p= 0.019 respectively). In the ALR group, 6 patients (20%) had PTT at their 12-month follow-up visit compared with 15 patients (53.6%) seen in the PLTR group (P = 0.008) (Table 2). Absolute risk reduction was 33.6% (95% (CI= 9% −58%)). Figure 1 demonstrates PTT 6 months following PLTR in spite of initial good correction. Out of the 6 patients with PPT in ALR group, 4 patients had anterior lamellar laxity pressing the lashes against the globe (Figure 2). Kaplan-Meier analysis revealed that the mean time for recurrence was 8.8 months in the PTLR group (95% CI=7.1–10.5 months), while the mean time for recurrence in the ALR group was 11.4 months (95% CI=10.7–12.1 months), p-value = 0.005 (Figure 3).
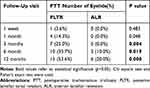 |
Table 2 Comparison of the Recurrence Rate (PTT) Between Both Study Groups at Different Points of Follow-Up |
Cosmetic dissatisfaction was significantly more frequent in the ALR group at 1 week, 1 month and 3 months of follow up compared to the PLTR group. However, this difference was no longer significant at 6 months and 12 months follow up (Table 3). Figure 4 demonstrates gradual softening of the split lid margins following ALR with final good position and cosmesis. Logistic regression model showed no association between preoperative location, number, and type of trichiatic lashes or the lid margin position with the rate of recurrence. No intraoperative or other postoperative complications were encountered in either group.
 |
Table 3 Cosmetic Satisfaction of Participants in Each Group |
Discussion
Although TT in the lower eyelids is not uncommon (11.5% of patients with TT),4 there is a scarcity of data on surgical correction of this condition. Universally, there is a paradigm shift toward the use of reconstructive surgical procedures rather than focal lash treatments for trichiasis.6
Many corrective surgical techniques have been described to address trichiasis for the upper lids and can be broadly separated into tarsus-involving and tarsus-sparing techniques.8 WHO adopts tarsotomy procedures for upper eyelid TT with no recommended technique to address this condition in the lower eyelid.7 Recently, studies have suggested that PLTR is superior to BLTR.12–14 The overall failure rates of these procedures are significant in the upper eyelid which cast doubt on their effectiveness to treat the vertically shorter lower eyelid. On the contrary, some authors have reported high success rates with lamellar splitting procedures which spare the tarsoconjunctiva.9,10
This study compares the effectiveness of a tarsus-involving procedure (PLTR) and a tarsus-sparing procedure (ALR) to address lower eyelid TT. To our best knowledge, this is the first RCT comparing PLTR with ALR for lower eyelid TT correction. In this trial, the results suggest that ALR is more effective than PLTR for correction of lower eyelid trachomatous trichiasis at the final follow-up visit.
ALR has the advantage that the surgery is being performed anterior to the tarsal plate, thereby avoiding trauma to the conjunctiva with its sequelae.8 In addition, it does not compromise the meibomian glands which is particularly advantageous in patients with chronic trachoma. Recently, AlDarrab et al reported significant meibomian gland atrophy with correlated affection of dry eye parameters in patients with trachoma sequelae.15 Therefore, preserving meibomian glands during trachomatous trichiasis surgery helps prevent additional ocular surface compromise.
ALR is particularly important in cases of metaplastic lashes that arise at or near orifices of meibomian glands. Lamellar splitting gives access to these aberrant lash follicles to be extirpated.16 In addition, the lid margin incision can be performed posterior to the more posterior aberrant eyelashes.17
Anterior lamellar laxity with dermatochalasis was found in 4 patients with PTT who underwent ALR without repositioning sutures early in the study. However, the use of mattress sutures between lower lid retractors and anterior lamella has eliminated this complication in subsequent cases given the resultant anterior lamellar tightening.18 Additional potential advantage of these sutures is prevention of upward sliding of anterior lamella to its original position till firm adhesion between both lamellae form.19
The suboptimal surgical results among the PLTR group could be attributed for the following: first, a horizontal tarsal incision will leave a small distal segment of only 2mm to be rotated. This can hinder effective lid margin eversion.20,21 Habtamu et al13 found that cases with an incision height of ≥ 4 mm from the lid margin in PLTR surgery are less likely to have trichiasis recurrence which is impractical in lower lid surgery due to the shorter height of the lower tarsus. Second, the horizontal tarsotomy carries the disadvantage of violating the tarsal plate which may further shorten it and destabilize the eyelid.15,22 Third, tarsoconjunctival incision in PLTR theoretically aggravates inflammation and may further enhance the trachomatous scarring process with additional contracture of the conjunctiva and deeper tissues.23–25 This can explain the escalated recurrence rate of PTT with time following the initial good results.
A few studies9,10,21 have described the surgical results after the use of tarsus sparing procedures in patients with lower eyelid cicatricial entropion. Malhotra et al10 reported the outcomes of a gray-line split, retractor recession, anterior lamella repositioning. They achieved a final surgical success rate of 90%. However, 38% of the cases required a second operation within 1 year of the surgery. In addition, they defined their success by improvement in lid margin position without comment on PTT. Choi et al9 used a modified technique of anterior lamellar reposition with dissection being performed at two sites, ie the grey line and subciliary incision in patients with lower eyelid marginal entropion. Of included 30 eyelids, 27 (90%) had successful postoperative results as without trichiasis. In this study, we split lids at lid margin only just posterior to aberrant lashes without the need for additional skin incisions. Three sutures from retractors traversing anterior lamella were enough to maintain anterior lamellar recession in our used technique.11
Cruz et al21 described the use of autogenous tarsal graft that was interposed between the pretarsal anterior lamella and the tarsus to correct 23 lower lids with trichiasis. PPT was seen in 6 eyelids (in the graft area in 1 lid, and outside the graft area in 5 lids). However, the unpredictable lid margin re-thinning in addition to the presence of a second surgical site with possible related complications may negate the use of this technique.
Other authors26–29 used lamellar splitting with eyelash resection procedure for cicatricial entropion with good results. However, owing to cosmetic concerns and risk of lagophthalmos, we think that lash resection should be regarded as the last resort after failure of lash preserving methods. Ferraz et al30 compared the outcomes of lid split with graft versus lash resection in conjunction with skin advancement flap for non-trachomatous major trichiasis in 89 lower lids. PTT occurred in 80% and 52.5% lids in lid split and lash resection groups, respectively. They attributed the low success rate in both groups of their study to the persistence of the primary cause.
Regarding postoperative cosmesis, marginal thickening with abnormal appearance was noticed in all patients underwent ALR during the early postoperative period; however, this tends to soften with reversion to normal skin color within few weeks. Similarly, Ahmed and Abdelbaky17 showed that most separated lid margins reverted to their normal color with upward remigration of anterior lamella within 3 months. The authors believe that preoperative counseling regarding possible poor cosmesis in the early postoperative period following ALR is important to reduce postoperative patient’s anxiety.
The lack of masking of the used technique from outcome assessor is a limitation to the current study.
In conclusion, the ALR procedure is related to a much more favorable outcome, but it requires a more gradual learning curve. PLTR has a higher rate of postoperative trichiasis. Despite this, it remains a simple technique requiring basic surgical skills.
Data Sharing
The data that support the findings of this study are available upon reasonable request from the corresponding author, after deidentification. The data are not publicly available due to their containing information that could compromise the privacy of research participants. Study protocol will be also available. Data will be available beginning 3 months and ending 12 months following article publication for researchers who provide a methodologically sound proposal.
Acknowledgment
We acknowledge Richard C. Allen, MD PhD FACS for critical discussions and review of the manuscript.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Taylor HR, Burton MJ, Haddad D, West S, Wright H. Trachoma. Lancet. 2014;384:2142–2152. doi:10.1016/S0140-6736(13)62182-0
2. Rajak SN, Habtamu E, Weiss HA, et al. The clinical phenotype of trachomatous trichiasis in Ethiopia: not all trichiasis is due to Entropion. Invest Ophthalmol Vis Sci. 2011;52(11):7974–7980. doi:10.1167/iovs.11-7880
3. Merbs S, Resnikoff S, Kello AB, Mariotti S, Greene G, West SK. Trichiasis Surgery for Trachoma.
4. Cassard SD, Merbs SL, Harding JC, Munoz BE, West SK. The epidemiology of lower eyelid trachomatous trichiasis among upper eyelid trichiasis surgery patients [poster B0093, Association for Research in Vision and Ophthalmology 2013 Annual Meeting]. Invest Ophthalmol Vis Sci. 2013;54(15):869.
5. Rajak SN, Collin JR, Burton MJ. Trachomatous trichiasis and its management in endemic countries. Surv Ophthalmol. 2012;57(2):105–135. doi:10.1016/j.survophthal.2011.08.002
6. Nerad JA. Techniques in Ophthalmic Plastic Surgery: A Personal Tutorial. USA: Elsevier Health Sciences; 2009.
7. World Health Organization Alliance for the Global Elimination of Trachoma by 2020. Second Global Scientific Meeting on Trachomatous Trichiasis. Cape Town, South Africa; November 4–6, 2015. Available from: https://www.who.int/trachoma/resources/who_htm_ntd_2016.5/en/.
8. Diab MM, Allen RC, Gawdat TI, Saif AS. Trachoma elimination, approaching 2020. Curr Opin Ophthalmol. 2018;29(5):451–457. doi:10.1097/ICU.0000000000000504
9. Choi YJ, Jin HC, Choi JH, et al. Correction of lower eyelid marginal entropion by eyelid margin splitting and anterior lamellar repositioning. Ophthal Plast Reconstr Surg. 2014;30:51–56. doi:10.1097/IOP.0000000000000008
10. Malhotra R, Yau C, Norris JH. Outcomes of lower eyelid cicatricial entropion with grey-line split, retractor recession, lateral-horn lysis, and anterior lamella repositioning. Ophthal Plast Reconstr Surg. 2012;28(2):134–139. doi:10.1097/IOP.0b013e3182467c11
11. Sodhi PK, Yadava U, Mehta DK. Efficacy of lamellar division for correcting cicatricial lid entropion and its associated features unrectified by the tarsal fracture technique. Orbit. 2002;21(1):9–17. doi:10.1076/orbi.21.1.9.2600
12. Habtamu E, Wondie T, Aweke S, et al. Posterior lamellar versus bilamellar tarsal rotation surgery for trachomatous trichiasis in Ethiopia: a randomised controlled trial. Lancet Glob Health. 2016;4(3):e175–e184. doi:10.1016/S2214-109X(15)00299-5
13. Habtamu E, Wondie T, Aweke S, et al. Predictors of trachomatous trichiasis surgery outcome. Ophthalmology. 2017;124(8):1143–1155. doi:10.1016/j.ophtha.2017.03.016
14. Habtamu E, Wondie T, Tadesse Z, et al. Posterior lamellar versus bilamellar tarsal rotation surgery for trachomatous trichiasis: long-term outcomes from a randomised controlled trial. EClinicalMedicine. 2019;17:100202. doi:10.1016/j.eclinm.2019.10.015
15. AlDarrab A, Al-Faky YH, Mousa A, Alsuhaibani AH. Meibography of eyes with sequelae of trachoma. Cornea. 2018;37(4):416–420. doi:10.1097/ICO.0000000000001490
16. Chi MJ, Park MS, Nam DH, Moon HS, Baek SH. Eyelid splitting with follicular extirpation using a monopolar cautery for the treatment of trichiasis and distichiasis. Graefes Arch Clin Exp Ophthalmol. 2007;245(5):637–640. doi:10.1007/s00417-005-0176-3
17. Ahmed RA, Abdelbaky SH. Short term outcome of anterior lamellar reposition in treating trachomatous trichiasis. J Ophthalmol. 2015;2015:568363. doi:10.1155/2015/568363
18. Collin JRO. A Manual of Systematic Eyelid Surgery.
19. Aghai GH, Gordiz A, Falavarjani KG, Kashkouli MB. Anterior lamellar recession, blepharoplasty, and supratarsal fixation for cicatricial upper eyelid entropion without lagophthalmos. Eye (Lond). 2016;30(4):627–631. doi:10.1038/eye.2016.12
20. Rajak SN, Habtamu E, Weiss HA, et al. Epilation for trachomatous trichiasis and the risk of corneal opacification. Ophthalmology. 2012;119(1):84–89. doi:10.1016/j.ophtha.2011.06.045
21. Cruz AAV, Garcez C, Duarte A, Akaishi PMS. Interlamellar autogenous tarsal graft for the correction of lower eyelid trichiasis associated with eyelid margin thinning. Ophthal Plast Reconstr Surg. 2018;34(6):522–524. doi:10.1097/IOP.0000000000001073
22. Kersten RC, Kleiner FP, Kulwin DR. Tarsotomy for the treatment of cicatricial entropion with trichiasis. Arch Ophthalmol. 1992;110(5):714–717. doi:10.1001/archopht.1992.01080170136042
23. Burton MJ, Rajak SN, Hu VH, et al. Pathogenesis of progressive scarring trachoma in Ethiopia and Tanzania and its implications for disease control: two cohort studies. PLoS Negl Trop Dis. 2015;9(5):e0003763. doi:10.1371/journal.pntd.0003763
24. Burton MJ, Bailey RL, Jeffries D, et al. Conjunctival expression of matrix metalloproteinase and proinflammatory cytokine genes after trichiasis surgery. Invest Ophthalmol Vis Sci. 2010;51:3583–3590. doi:10.1167/iovs.09-4550
25. Burton MJ, Rajak SN, Ramadhani A, et al. Post-operative recurrent trachomatous trichiasis is associated with increased conjunctival expression of S100A7 (Psoriasin). PLoS Negl Trop Dis. 2012;6:e1985. doi:10.1371/journal.pntd.0001985
26. Moosavi AH, Mollan SP, Berry-Brincat A, Abbott J, Sutton GA, Murray A. Simple surgery for severe trichiasis. Ophthalmic Plast Reconstr Surg. 2007;23(4):296–297. doi:10.1097/IOP.0b013e318070cd26
27. Wu AY, Thakker MM, Wladis EJ, Weinberg DA. Eyelash resection procedure for severe, recurrent, or segmental cicatricial entropion. Ophthalmic Plast Reconstr Surg. 2010;26:112–116. doi:10.1097/IOP.0b013e3181b8c900
28. Kadyan A, Barry R, Murray A. Anterior lamellar excision and laissez-faire healing for aberrant lashes in ocular cicatricial pemphigoid. Eye (Lond). 2010;24(6):990–993. doi:10.1038/eye.2009.268
29. Wojno TH. Lid splitting with lash resection for cicatricial entropion and trichiasis. Ophthalmic Plast Reconstr Surg. 1992;8(4):
30. Ferraz LC, Meneghim RL, Galindo-Ferreiro A, et al. Outcomes of two surgical techniques for major trichiasis treatment. Orbit (Lond). 2018;37(1):36–40. doi:10.1080/01676830.2017.1353108
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.