Back to Journals » Clinical Ophthalmology » Volume 17
Anatomical and Functional Outcomes in Delayed Onset versus Concurrent Retinal Detachment in Endophthalmitis
Authors Srinivasan R, Roy K, Mahesh M, Surya J , Raman R
Received 10 September 2022
Accepted for publication 21 December 2022
Published 7 January 2023 Volume 2023:17 Pages 115—121
DOI https://doi.org/10.2147/OPTH.S389474
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Ramyaa Srinivasan,* Krishnakanta Roy,* Meenakshi Mahesh, Janani Surya, Rajiv Raman
Shri Bhagwan Mahavir Vitreoretinal Services, Vision Research Foundation – Sankara Nethralaya, Chennai, Tamil Nadu, India
*These authors contributed equally to this work
Correspondence: Rajiv Raman, Shri Bhagwan Mahavir Vitreoretinal Services, Vision Research Foundation – Sankara Nethralaya, Sankara Nethralaya (Main Campus), No. 41 (Old 18), College Road, Chennai, Tamil Nadu, 600006, India, Tel +91 9444288708, Fax +91-44-28254180, Email [email protected]
Purpose: To determine the functional and anatomical outcomes of patients with endophthalmitis with concurrent or delayed onset retinal detachment (RD), and compare the preoperative, intraoperative and postoperative features.
Patients and Methods: This was a retrospective review of 121 eyes in 121 patients presenting with endophthalmitis and RD. Subjects were categorized into two groups: endophthalmitis with delayed onset RD (group 1, N=76) and endophthalmitis with concurrent RD (group 2, N=45).
Results: The mean age of patients in groups 1 and 2 was 38.21± 21.60 and 46.78± 24.42 years, respectively (P=0.047). Exogenous endophthalmitis was common in both groups 1 and 2 (86.84% and 84.44%, respectively). No significant differences were found between the groups in the type of RD, retinal breaks, number of quadrants involved or proliferative vitreoretinopathy grade. In the overall cohort, visual acuity improved post-surgery in one-third of the patients who were in the near or total blindness category at presentation. We found good anatomical success rates of an attached retina in both groups 1 and 2 (84.3% and 77.7%, P=0.376).
Conclusion: Our study presents the results of patients with endophthalmitis and delayed onset RD or concurrent RD. It shows a few differences in presentation between the groups, but the anatomical and functional outcomes were almost the same.
Keywords: endophthalmitis, delayed onset retinal detachment, concurrent retinal detachment, functional outcomes and anatomical outcomes
Introduction
Endophthalmitis is a devastating condition characterized by a severe intraocular infection that is often associated with poor visual outcomes.1 Although retinal detachment (RD) has been described as an uncommon complication in endophthalmitis, an early diagnosis is imperative as it significantly affects the management strategies and visual outcomes in these patients.2 The postoperative functional and anatomical outcomes of RD in endophthalmitis are dependent on the etiology, virulence of the causative microorganisms, severity of intraocular inflammation, status of proliferative vitreoretinopathy (PVR), time of diagnosis, visual acuity (VA) at presentation, presence of an intraocular foreign body and timing of treatment.2 In the setting of endophthalmitis, RD may be either diagnosed as a part of initial presentation or noted on follow-up after the therapeutic vitrectomy procedure.
A number of studies have analyzed the incidence and outcomes of concurrent or delayed RD in endophthalmitis. In a study by Nelson et al, 16% of cases exogenous endophthalmitis were noted to develop RD within 6 months of initial presentation; 21% of post-vitrectomy patients developed RD, and among the 22 patients managed conservatively, only 9% developed RD.3 Olsen et al evaluated 40 cases of postoperative endophthalmitis, with an overall rate of RD of 10%. RD was noted in 14% of vitrectomized eyes in this study.4 Foster et al discussed the risk factors for poor visual outcomes in eyes with concurrent endophthalmitis and RD, including open globe injuries, high virulence of organisms, retained intraocular foreign body, choroidal detachment at the time of diagnosis and posterior capsular rupture.5 In the Endophthalmitis Vitrectomy Study, the incidence of RD was noted to be 8.3% after the treatment of endophthalmitis. VA of 20/40 was achieved in 55.2% of patients who did not develop RD and 26.7% of those with RD.2 Dave et al recorded rates of 21.5% concurrent RD and 78.5% delayed onset RD in their cohort.6
These studies were limited by either a small sample sizes or a lack of microbiological correlations. The aim of our study is to determine the functional and anatomical outcomes of patients with endophthalmitis with concurrent or delayed onset RD, and to compare the preoperative, intraoperative and postoperative features in these two presentations of RD in patients with endophthalmitis.
Materials and Methods
The current study is a retrospective review of patients diagnosed with endophthalmitis and RD at a tertiary eye care hospital in South India. We identified 121 eyes in 121 patients presenting with endophthalmitis and concurrent or delayed onset RD between January 2005 and December 2017. Approval for the study was granted by the institutional review board of the Vision Research Foundation – Sankara Nethralaya. The study protocol followed the tenets of the Declaration of Helsinki. Written informed consent was obtained from all patients at the first hospital visit.
The study subjects were categorized into two groups: endophthalmitis with delayed onset RD as group 1 and endophthalmitis with concurrent RD as group 2. Subjects with delayed onset RD developed RD within the first 2 weeks after the intervention, but had no RD on presentation. Subjects with concurrent RD presented with RD along with endophthalmitis on the first visit. The following data were collected from the electronic medical records and were compared between the two groups (delayed onset RD vs concurrent RD): age, gender, etiology of endophthalmitis, VA, lens status at presentation, presence or absence of intraocular foreign body, microbiological profile, type of retinal breaks (if present), type of RD and quadrants involved, PVR status at presentation and details of initial treatment. Final follow-up details included the duration of follow-up, VA, and anatomical and functional outcomes. The etiology of endophthalmitis was divided into exogenous (post-surgery, post-trauma) and endogenous. Lens status was classified into clear, cataractous, pseudophakia and aphakia. The VA at presentation and at the last follow-up was recorded and then categorized as per the ICD visual impairment categories, into mild (LogMAR: 0.2–0.5), moderate (LogMAR: 0.6–0.9), severe (LogMAR: 1.0–1.3), profound (LogMAR: 1.4–1.7) and near blindness (LogMAR: ≥1.8) visual impairment.7 Aqueous and vitreous samples were obtained for the microbiological diagnosis of endophthalmitis. As a routine care procedure, aqueous tap was obtained. Vitreous tap was taken only in cases undergoing vitrectomy. RD was confirmed on clinical examination with either indirect ophthalmology or ultrasonography (in cases with a poor direct view of the fundus). We categorized RD as rhegmatogenous, tractional and combined. PVR was also graded.8 The line of management was decided by the vitreoretinal surgeon based on the severity of the disease. The anatomical outcome was described based on the status of the retina as attached, attached with atrophy or detached. The globe status at the final follow-up was described as normal architecture, phthisis bulbi, eviscerated or enucleated. Functional outcome was defined according to the ICD visual impairment category into mild, moderate, severe, profound and near/total blindness.
The data were entered in MS Excel, and statistical analysis was performed using a commercially available statistical software package (SPSS for Windows, version 21.0; IBM Corp., Armonk, NY). The data were tested for normality using the Kolmogorov–Smirnov test. The results were expressed as number and percentage for categorical data, and continuous data were expressed as mean with standard deviation. Independent samples t-tests and chi-squared tests were used to check for the existence of significant differences between the two groups. We considered P<0.05 to be significant for these analyses.
Results
Of the 121 endophthalmitis patients included in the study, 76 subjects (62.8%) belonged to the delayed onset RD group (group 1) and the remaining 45 subjects (37.2%) belonged to the concurrent RD group (group 2). The baseline characteristics and microbiological profiles of groups 1 and 2 are summarized in Table 1.
 |
Table 1 Baseline Characteristics and Microbiological Profiles of Group 1 and Group 2 |
The mean age of patients in group 1 and group 2 was 38.21±21.60 and 46.78±24.42 years, respectively (P=0.047). A male predominance was noted in both groups. Exogenous endophthalmitis was common in both groups, with rates of 86.84% and 84.44%, respectively. Cataract surgery was the most predominant post-surgical etiology of endophthalmitis, with 32 patients (42.10%) and 25 patients (55.55%) in groups 1 and 2, respectively. Intraocular foreign body was noted in five patients in group 1 and two patients in group 2. It was found that 39.47% and 51.11% of the eyes were pseudophakic in groups 1 and 2, respectively. Subjects in group 1 had a statistically significant better mean VA at presentation than those in group 2 (20/3724 and 20/4581, respectively, P=0.047). In both groups 1 and 2, most of the patients were diagnosed with a combination of vitreous and aqueous tap (69.7% and 55.5%). Culture was found to be positive in 38.1% and 28.8% in groups 1 and 2, respectively. The predominant organisms isolated on culture were Gram-positive cocci and Gram-negative bacilli in group 1 (37.9% and 34.4%, respectively), and Gram-negative bacilli in group 2 (53.8%).
All cases in group 1 underwent vitrectomy immediately after diagnosis with endophthalmitis. The mean duration of presentation with RD was 6 days postoperatively. Table 2 shows the characteristics of RD in both groups. The majority of cases in groups 1 and 2 could be diagnosed as RD on clinical examination alone, with the use of indirect ophthalmoscopy (92.1% and 84.4%, respectively). There were no significant differences between the groups in the type of RD, type of retinal break, number of quadrants involved in RD or PVR grade. Most of the cases in groups 1 and 2 were diagnosed as having rhegmatogenous RD, ie 66 eyes (86.8%) in group 1 and 42 eyes in group 2 (93.2%). The rest of the cases had tractional or combined detachments. No cases of exudative detachments were noted.
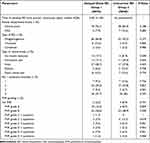 |
Table 2 Details of Initial Treatment and Retinal Status After First Surgery |
Intraoperatively, 22 subjects in group 1 underwent vitrectomy with 20 gauge and 54 subjects with 23 gauge. PVD (the separation of the cortical vitreous from the neurosensory layer of the retina) was noted in 12 subjects in group 1. In group 2 patients, vitrectomy was carried out with 20 gauge in 17 cases and 23 gauge in 28 cases. PVD was present in 15 cases. Silicone oil (SiO) tamponade with 1000 cs was used in 40 cases and SiO with 5000 cs was used in five cases. Relaxing retinotomy and retinectomy was performed in 21 subjects in view of PVR changes.
Figure 1 shows the categories of visual impairment on presentation with RD and on follow-up in both groups. In patients with delayed onset RD, 62 (81.6%) of 76 subjects had near or total blindness on presentation with RD. The final VA improved in 26 subjects (34.21%). Statistically significant differences were seen between preoperative and postoperative vision in the moderate (P=0.005), severe (P=0.011) and near or total blindness (P=0.009) categories in group 2. Likewise, in the concurrent RD group, 41 (91.1%) of 45 subjects belonged to the near or total blindness category, and after surgery, the VA improved in 16 subjects (35.55%). Statistically significant differences were seen in the severe (P=0.034) and near blindness (P=0.049) categories in this group. The difference in VA between the two groups on final follow-up was not statistically significant (P=0.267).
 |
Figure 1 The categories of visual impairment before initial surgery and after final surgery in the two groups. |
Table 3 shows the functional and anatomical outcomes on final follow-up. An attached retina on follow-up was noted in 84.3% and 77.7% in groups 1 and 2, respectively. The majority of the cases had a normal architecture of the globe in both group 1 (77.6%) and group 2 (77.8%). No significant differences were noted in the retinal status and globe architecture between the groups.
 |
Table 3 Functional and Anatomical Outcomes at the Last Follow-Up |
Discussion
This study is a comparative analysis of patients with endophthalmitis diagnosed with either delayed onset or concurrent RD. We compared the demographic, microbiological and RD characteristics, and reported anatomical and functional success in both groups. The patients in group 1 (delayed onset RD) were slightly younger than the patients in group 2 (concurrent RD). The mean age at presentation was in the late 30s for group 1 and the late 40s for group 2. Previous studies have reported a bimodal peak with two predominant presentations in either the third decade or the sixth decade.3,6,9–12 The etiology of endophthalmitis in both of our groups was found to be exogenous in >80% of the study patients. While cataract surgery and trauma was noted as the most common etiology for exogenous endophthalmitis in group 1, cataract surgery alone was the predominant etiology in group 2. In the study by Dave et al, trauma was recorded as the major cause of endophthalmitis in both concurrent RD and delayed onset RD.6 Foster et al reported that in eyes with concurrent endophthalmitis and RD, 81% were noted to have exogenous infections.5 Wang et al described that in patients with delayed onset RD, the etiology was exogenous in 86.1% and a result of postoperative infection in 38.9%.9
We noted that the organisms isolated on culture were predominantly Gram-positive cocci and Gram-negative bacilli in group 1, and Gram-negative bacilli in group 2. Gram-negative endophthalmitis is associated with poor presenting VA and is similarly associated with very poor visual outcomes.13 Ramakrishnan et al also recorded Gram-negative bacilli as the predominant cause of fulminant cases of endophthalmitis.14
In groups 1 and 2 of our study, VA improved in 26 patients (34.21%) and 16 patients (35.55%), respectively. Although there was no statistically significant difference between the two, the final VA in group 1 (20/1291) was noted to be marginally better than in group 2 (20/1625). In the Endophthalmitis Vitrectomy Study, out of the 12 patients who had undergone vitrectomy for RD, eight patients achieved a VA of 20/40.2 In the study by Lee et al, 17 eyes with endophthalmitis developed rhegmatogenous RD and were recorded as having a VA of 20/3271, 6 months after initial presentation. They described six eyes as having redetachments and a VA of light perception or no light perception on follow-up. Also, 11 rhegmatogenous RD eyes with an attached macula were found to have a mean VA of 20/121.12
The majority of detachments in both groups in this study were noted to be due to atrophic holes. This reemphasizes the importance of a thorough peripheral retinal evaluation in follow-up cases with endophthalmitis and during the primary vitrectomy itself, if possible. Most of the eyes in both groups were noted to have grade B PVR changes. Bonnet and Guenoun described grade B PVR as a significant risk factor for poor reattachment rates following a single surgical intervention.15 In our study, an attached retina on follow-up was noted in 84.3% and 77.7% in groups 1 and 2, respectively. Nelson et al, Olson et al and Ficker et al have similarly reported reattachment rates of 85.7%, 50% and 66.7%, respectively, following surgical repair for RD after endophthalmitis.3,4,16 In the study by Dave et al, complete retinal reattachment and VA of 20/400 or better was achieved in 73.7% and 30% of the cases with concurrent RD, and in 98.5% and 39.7% of cases with delayed onset RD, respectively.6
Although the two categories of RD differed in their time frame of presentation and whether or not surgical intervention has been performed prior to the development, they did not present significant differences in terms of etiology, microbiological profile, type and extent of RD, type of break, or final anatomical and functional outcomes, along with PVR changes. One reason for this could be that all of our delayed RD cases developed RD within 2 weeks of vitrectomy, when the infection was still not completely resolved and directly contributed to the final outcomes. Also, as both conditions are driven by a similar etiological process in terms of the type of hole, organisms and similar PVR grades, the outcomes after very similar surgical procedures were comparable.
Our study has limitations that were inherent to its retrospective nature. There was no standardization of the treatment protocol or surgical option, as multiple surgeons were involved. We did not include the associated risk factors, but our study was not designed to explore these. Future multi-center studies with large sample sizes are required to address these limitations.
Conclusion
Our study presents the outcomes in patients with endophthalmitis with concurrent or delayed onset RD. Although the presenting visual acuity and status of the retina showed significant variation at presentation, the anatomical and functional outcomes were almost the same. Hence, the visual acuity and final retinal status did not differ significantly based on whether the RD was concurrent or delayed onset in nature.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Kresloff MS, Castellarin AA, Zarbin MA. Endophthalmitis. Surv Ophthalmol. 1998;43(3):193–224. doi:10.1016/s0039-6257(98)00036-8
2. Doft BM, Kelsey SF, Wisniewski SR; Endophthalmitis Vitrectomy Study Group. Retinal detachment in the endophthalmitis vitrectomy study. Arch Ophthalmol. 2000;118(12):1661–1665. doi:10.1001/archopht.118.12.1661
3. Nelsen PT, Marcus DA, Bovino JA. Retinal detachment following endophthalmitis. Ophthalmology. 1985;92(8):1112–1117. doi:10.1016/S0161-6420(85)33916-7
4. Olson JC, Flynn HW, Forster RK, Culbertson WW. Results in the treatment of postoperative endophthalmitis. Ophthalmology. 1983;90(6):692–699. doi:10.1016/S0161-6420(83)34511-5
5. Foster RE, Rubsamen PE, Joondeph BC, Flynn HW, Smiddy WS. Concurrent endophthalmitis and retinal detachment. Ophthalmology. 1994;101(3):490–498. doi:10.1016/S0161-6420(94)31308-X
6. Dave VP, Pathengay A, Relhan N, et al. Endophthalmitis and concurrent or delayed-onset rhegmatogenous retinal detachment managed with pars plana vitrectomy, intravitreal antibiotics, and silicone oil. Ophthalmic Surg Lasers Imaging. 2017;48(7):546–551. doi:10.3928/23258160-20170630-05
7. Colenbrander A. Aspects and ranges of vision loss.
8. Hilton G, Machemer R, Michels R, Okun E, Schepens C, Schwartz A. The classification of retinal detachment with proliferative vitreoretinopathy. Ophthalmology. 1983;90(2):121–125. doi:10.1016/s0161-6420(83)34588-7
9. Wang T, Moinuddin O, Abuzaitoun R, et al. Retinal Detachment after endophthalmitis: risk factors and outcomes. Clin Ophthalmol. 2021;15:1529. doi:10.2147/OPTH.S302757
10. Cohen SM, Flynn HW, Murray TG, et al. Endophthalmitis after pars plana vitrectomy. Ophthalmology. 1995;102(5):705–712. doi:10.1016/S0161-6420(95)30965-7
11. Eifrig CW, Scott IU, Flynn HW, Smiddy WE, Newton J. Endophthalmitis after pars plana vitrectomy: incidence, causative organisms, and visual acuity outcomes. Am J Ophthalmol. 2004;138(5):799–802. doi:10.1016/j.ajo.2004.06.035
12. Lee T, Robbins CB, Feng HL, Fekrat S. Rhegmatogenous retinal detachment in the setting of endophthalmitis: risk factors and visual outcomes. Ophthalmic Surg Lasers Imaging. 2021;52(5):257–262. doi:10.3928/23258160-20210429-03
13. Stevenson LJ, Dawkins RCH, Sheorey H, McGuinness MB, Hurley AH, Allen PJ. Gram-negative endophthalmitis: a prospective study examining the microbiology, clinical associations and visual outcomes following infection. Clin Exp Ophthalmol. 2020;48(6):813–820. doi:10.1111/ceo.13768
14. Ramakrishnan R, Bharathi MJ, Shivkumar C, et al. Microbiological profile of culture-proven cases of exogenous and endogenous endophthalmitis: a 10-year retrospective study. Eye. 2009;23(4):945–956. doi:10.1038/eye.2008.197
15. Bonnet M, Guenoun S. Surgical risk factors for severe postoperative proliferative vitreoretinopathy (PVR) in retinal detachment with grade B PVR. Graefes Arch Clin Exp Ophthalmol. 1995;233(12):789–791. doi:10.1007/BF00184091
16. Ficker LA, Meredith TA, Wilson LA, Kaplan HJ. Role of vitrectomy in Staphylococcus epidermidis endophthalmitis. Br J Ophthalmol. 1988;72(5):386–389. doi:10.1136/bjo.72.5.386
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
